Abstract
Background
The results of laparoscopic pancreaticoduodenectomy combining with mesentericoportal vein resection and reconstruction (LPD-MPVRs) for pancreatic head adenocarcinoma are rarely reported. The aim of present study was to explore the short- and long-term outcomes of different type of LPD-MPVRs.
Methods
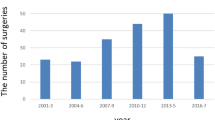
Patients who underwent LPD-MPVRs in 14 Chinese high-volume pancreatic centers between June 2014 and December 2020 were selected and compared.
Results
In total, 142 patients were included and were divided into primary closure (n = 56), end-end anastomosis (n = 43), or interposition graft (n = 43). Median overall survival (OS) and median progress-free survival (PFS) between primary closure and end-end anastomosis had no difference (both P > 0.05). As compared to primary closure and end-end anastomosis, interposition graft had the worst median OS (12 months versus 19 months versus 17 months, P = 0.001) and the worst median PFS (6 months versus 15 months versus 12 months, P < 0.000). As compared to primary closure, interposition graft had almost double risk in major morbidity (16.3 percent versus 8.9 percent) and about triple risk (10 percent versus 3.6 percent) in 90-day mortality, while End-end anastomosis had only one fourth major morbidity (2.3 percent versus 8.9 percent). Multivariate analysis revealed postoperation hospital stay, American Society of Anesthesiologists (ASA) score, number of positive lymph nodes had negative impact on OS, while R0, R1 surgical margin had protective effect on OS. Postoperative hospital stay had negative impact on PFS, while primary closure, end-end anastomosis, short-term vascular patency, and short-term vascular stenosis positively related to PFS.
Conclusions
In LPD-MPVRs, interposition graft had the worst OS, the worst PFS, the highest rate of major morbidity, and the highest rate of 90-day mortality. While there were no differences in OS and PFS between primary closure and end-end anastomosis.


Similar content being viewed by others
References
Gagner M, Pomp A (1994) Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 8(5):408–410
Whipple AO (1945) Pancreaticoduodenectomy for islet carcinoma : a five-year follow-up. Ann Surg 121(6):847–852
Traverso LW, Longmire WP Jr (1980) Preservation of the pylorus in pancreaticoduodenectomy a follow-up evaluation. Ann Surg 192(3):306–310
Palanivelu C et al (2007) Laparoscopic pancreaticoduodenectomy: technique and outcomes. J Am Coll Surg 205(2):222–230
Kendrick ML, Cusati D (2010) Total laparoscopic pancreaticoduodenectomy: feasibility and outcome in an early experience. Arch Surg 145(1):19–23
Mizrahi JD et al (2020) Pancreatic cancer. Lancet 395(10242):2008–2020
Strijker M et al (2019) Treatment and survival of resected and unresected distal cholangiocarcinoma: a nationwide study. Acta Oncol 58(7):1048–1055
Tol JA et al (2014) Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery 156(3):591–600
Wang X et al (2020) Laparoscopic pancreaticoduodenectomy: outcomes and experience of 550 patients in a single institution. Ann Surg Oncol 27(11):4562–4573
Han SH et al (2020) The Yonsei experience of 104 laparoscopic pancreaticoduodenectomies: a propensity score-matched analysis with open pancreaticoduodenectomy. Surg Endosc 34(4):1658–1664
Poves I et al (2018) Comparison of perioperative outcomes between laparoscopic and open approach for pancreatoduodenectomy: the padulap randomized controlled trial. Ann Surg 268(5):731–739
Khatkov I et al (2017) One hundred and forty five total laparoscopic pancreatoduodenectomies: a single centre experience. Pancreatology 17(6):936–942
Asbun HJ, Stauffer JA (2012) Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the accordion severity grading system. J Am Coll Surg 215(6):810–819
Bockhorn M et al (2014) Borderline resectable pancreatic cancer: a consensus statement by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 155(6):977–988
Machairas N et al (2021) The impact of neoadjuvant treatment on survival in patients undergoing pancreatoduodenectomy with concomitant portomesenteric venous resection: an international multicenter analysis. Ann Surg 274(5):721–728
Groen JV et al (2021) Venous wedge and segment resection during pancreatoduodenectomy for pancreatic cancer: impact on short- and long-term outcomes in a nationwide cohort analysis. Br J Surg 109(1):96–104
Ravikumar R et al (2017) Impact of portal vein infiltration and type of venous reconstruction in surgery for borderline resectable pancreatic cancer. Br J Surg 104(11):1539–1548
Wang X et al (2019) Laparoscopic pancreatoduodenectomy combined with portal-superior mesenteric vein resection and reconstruction with interposition graft: case series. Medicine (Baltimore) 98(3):e14204
Khatkov IE et al (2017) Superior mesenteric-portal vein resection during laparoscopic pancreatoduodenectomy. Surg Endosc 31(3):1488–1495
Croome KP et al (2015) Pancreaticoduodenectomy with major vascular resection: a comparison of laparoscopic versus open approaches. J Gastrointest Surg 19(1):189–94
Wang M et al (2021) Practice patterns and perioperative outcomes of laparoscopic pancreaticoduodenectomy in China: a retrospective multicenter analysis of 1029 patients. Ann Surg 273(1):145–53
Tempero MA et al (2021) Pancreatic adenocarcinoma, version 2.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 19(4):439–457
Declaration of Helsinki (1967) Recommendations guiding doctors in clinical research adopted by the World Medical Association in 1964. Wis Med J 66(1):25–6
von Elm E et al (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370(9596):1453–1457
Liao X, Zhang D (2021) The 8th edition American Joint Committee on Cancer Staging for Hepato-pancreato-biliary cancer: a review and update. Arch Pathol Lab Med 145(5):543–553
Wente MN et al (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142(5):761–768
Bassi C et al (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery 161(3):584–591
Wente MN et al (2007) Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142(1):20–25
Koch M et al (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149(5):680–688
Besselink MG et al (2017) Definition and classification of chyle leak after pancreatic operation: a consensus statement by the International Study Group on Pancreatic Surgery. Surgery 161(2):365–372
Dindo D et al (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Terasaki F et al (2019) Comparison of end-to-end anastomosis and interposition graft during pancreatoduodenectomy with portal vein reconstruction for pancreatic ductal adenocarcinoma. Langenbecks Arch Surg 404(2):191–201
Kantor O et al (2018) The extent of vascular resection is associated with perioperative outcome in patients undergoing pancreaticoduodenectomy. HPB (Oxford) 20(2):140–146
Han S et al (2021) Long-term outcomes following en bloc resection for pancreatic ductal adenocarcinoma of the head with portomesenteric venous invasion. Asian J Surg 44(1):313–320
Snyder RA et al (2018) Vein resection during pancreaticoduodenectomy for pancreatic adenocarcinoma: Patency rates and outcomes associated with thrombosis. J Surg Oncol 117(8):1648–1654
Gao W et al (2016) Comparison of patency rates and clinical impact of different reconstruction methods following portal/superior mesenteric vein resection during pancreatectomy. Pancreatology 16(6):1113–1123
Labori KJ et al (2021) Graft type for superior mesenteric and portal vein reconstruction in pancreatic surgery - a systematic review. HPB (Oxford) 23(4):483–494
Glebova NO et al (2015) Technical risk factors for portal vein reconstruction thrombosis in pancreatic resection. J Vasc Surg 62(2):424–433
Groen JV et al (2021) Resection of the portal-superior mesenteric vein in pancreatic cancer: pathological assessment and recurrence patterns. Pancreas 50(8):1218–1229
Al Farai A et al (2019) International Study Group of Pancreatic Surgery type 3 and 4 venous resections in patients with pancreatic adenocarcinoma:the Paoli-Calmettes Institute experience. Eur J Surg Oncol 45(10):1912–1918
Strobel O et al (2017) Pancreatic cancer surgery: the new R-status counts. Ann Surg 265(3):565–573
Bell R et al (2017) Meta-analysis and cost effective analysis of portal-superior mesenteric vein resection during pancreatoduodenectomy: Impact on margin status and survival. Surg Oncol 26(1):53–62
Tewari M (2016) Significance of pathological positive superior mesenteric/portal venous invasion in pancreatic cancer. Hepatobiliary Pancreat Dis Int 15(6):572–578
Ramacciato G et al (2016) Pancreatectomy with mesenteric and portal vein resection for borderline resectable pancreatic cancer: multicenter study of 406 patients. Ann Surg Oncol 23(6):2028–2037
Mierke F et al (2016) Impact of portal vein involvement from pancreatic cancer on metastatic pattern after surgical resection. Ann Surg Oncol 23(Suppl 5):730–736
Lyu S et al (2021) Long-term survival in patients with distal cholangiocarcinoma after pancreaticoduodenectomy combined with portal vein system resection and reconstruction. Langenbecks Arch Surg 406(6):1917–1924
Geers J et al (2020) 3D-laparoscopic pancreaticoduodenectomy with superior mesenteric or portal vein resection for pancreatic cancer. Surg Endosc 34(12):5616–5624
Roch AM et al (2016) Significance of portal vein invasion and extent of invasion in patients undergoing pancreatoduodenectomy for pancreatic adenocarcinoma. J Gastrointest Surg 20(3):479–87
Kleive D et al (2020) Pancreatoduodenectomy with venous resection for ductal adenocarcinoma rarely achieves complete (R0) resection. HPB (Oxford) 22(1):50–57
Hristov B et al (2010) Outcomes of adjuvant chemoradiation after pancreaticoduodenectomy with mesenterico-portal vein resection for adenocarcinoma of the pancreas. Int J Radiat Oncol Biol Phys 76(1):176–180
Murakami Y et al (2013) Benefit of portal or superior mesenteric vein resection with adjuvant chemotherapy for patients with pancreatic head carcinoma. J Surg Oncol 107(4):414–421
Maeda S et al (2020) Impact of resection margin status on survival in pancreatic cancer patients after neoadjuvant treatment and pancreatoduodenectomy. Surgery 167(5):803–811
Chandrasegaram MD et al (2014) Anticoagulation policy after venous resection with a pancreatectomy: a systematic review. HPB (Oxford) 16(8):691–698
Ouaissi M et al (2008) Therapeutic anticoagulant does not modify thromboses rate vein after venous reconstruction following pancreaticoduodenectomy. Gastroenterol Res Pract 2008:896320
Hashimoto D et al (2017) Efficacy and safety of postoperative anticoagulation prophylaxis with enoxaparin in patients undergoing pancreatic surgery: a prospective trial and literature review. Pancreatology 17(3):464–470
Chu CK et al (2010) Prosthetic graft reconstruction after portal vein resection in pancreaticoduodenectomy: a multicenter analysis. J Am Coll Surg 211(3):316–324
Stauffer JA et al (2009) Interposition graft with polytetrafluoroethylene for mesenteric and portal vein reconstruction after pancreaticoduodenectomy. Br J Surg 96(3):247–252
Kleive D et al (2018) Portal vein reconstruction using primary anastomosis or venous interposition allograft in pancreatic surgery. J Vasc Surg Venous Lymphat Disord 6(1):66–74
Cai Y et al (2018) Laparoscopic pancreaticoduodenectomy with major venous resection and reconstruction: anterior superior mesenteric artery first approach. Surg Endosc 32(10):4209–4215
Lapshyn H et al (2021) Postoperative outcomes of tangential versus segmental resection and end-to-end reconstruction of the superior mesenterico-portal vein during pancreatoduodenectomy for pancreatic adenocarcinoma: a single-center experience. Anticancer Res 41(10):5123–5130
Chan KS et al (2020) Comparison between long and short-term venous patencies after pancreatoduodenectomy or total pancreatectomy with portal/superior mesenteric vein resection stratified by reconstruction type. PLoS ONE 15(11):e0240737
Beane JD et al (2017) Pancreatoduodenectomy with venous or arterial resection: a NSQIP propensity score analysis. HPB (Oxford) 19(3):254–263
Kleespies A et al (2009) Blumgart anastomosis for pancreaticojejunostomy minimizes severe complications after pancreatic head resection. Br J Surg 96(7):741–750
Chen XP et al (2014) Chen’s U-suture technique for end-to-end invaginated pancreaticojejunostomy following pancreaticoduodenectomy. Ann Surg Oncol 21(13):4336–4341
Cai Y et al (2019) A novel technique of pancreaticojejunostomy for laparoscopic pancreaticoduodenectomy. Surg Endosc 33(5):1572–1577
Hong DF et al (2017) The role of Hong’s single-stitch duct to mucosa pancreaticojejunostomy in laparoscopic pancreaticoduodenectomy. Zhonghua Wai Ke Za Zhi 55(2):136–140
Acknowledgements
The authors would like to acknowledge Man Zhang, Yifeng Liu, Hui Wang, Guangsheng Yu, Xiaolong Liu, Yigang Wang, and Xuehui Peng for assistance in following-up patients.
Funding
This study was supported by National Institutes of Health of China (Grant No. W2017ZWS07).
Author information
Authors and Affiliations
Contributions
BP and GO: designed the study. GO, XZ, ZC, JL, SZ, DH, XY, JY, XB, YL, JL, XH, YX, JX, YC, ZJ and RC: collected and analyzed the data. GO: wrote the manuscript and all authors revised the manuscript. YC, ZJ, RC and BP: made the final approval of the version to be published.
Corresponding authors
Ethics declarations
Disclosures
Drs. Guoqing Ouyang, Xiaosheng Zhong, Zhiwei Cai, Jianhua Liu, Shangyou Zheng, Defei Hong, Xinmin Yin, Jian Yu, Xueli Bai, Yahui Liu, Jun Liu, Xiaobing Huang, Yong Xiong, Jie Xu, Yunqiang Cai, Zhongyi Jiang, Rufu Chen, and Bing Peng had no conflict of interests or financial ties to be disclosed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ouyang, G., Zhong, X., Cai, Z. et al. The short- and long-term outcomes of laparoscopic pancreaticoduodenectomy combining with different type of mesentericoportal vein resection and reconstruction for pancreatic head adenocarcinoma: a Chinese multicenter retrospective cohort study. Surg Endosc 37, 4381–4395 (2023). https://doi.org/10.1007/s00464-023-09901-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09901-2