Abstract
Background
Major vascular resection when necessary for margin control during pancreaticoduodenectomy is relatively universal with perioperative and oncological outcomes that are similar to those of patients undergoing a PD without venous involvement. The present study compares total laparoscopic pancreaticoduodenectomy (TLPD) versus open pancreaticoduodenectomy (OPD) with major vascular resection.
Methods
We reviewed data for all patients undergoing TLPD or OPD with vascular resection at Mayo Clinic Rochester, between the dates of July 2007 and July 2013.
Results
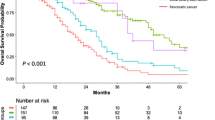
A total of 31 patients undergoing TLPD and 58 patients undergoing OPD with major vascular resection were identified. Mean operative blood loss was significantly less in the laparoscopic (842 cc) compared to the open group (1,452 cc) (p < 0.001), as was median hospital stay, 6 (4–118) versus 9 (6–73) days, respectively (p = 0.006). There was no significant difference in the total number of complications (lap 35 %, open 48 %) (p = 0.24) or severe complications (≥III) (lap 6.4 %, open 3.4 %) (p = 0.51) in the two groups. In-hospital mortality or 30-day mortality was not statistically different between the laparoscopic and open groups, 3.2 and 3.4 %, respectively (p = 0.96). Patency of the reconstructed vessels on postoperative imaging was not significantly different between the TLPD (93 %) and OPD groups (91 %) (p = 0.76). In patients with a diagnosis of adenocarcinoma, there was no significant difference in overall survival between the two groups (p = 0.22).
Conclusion
The present study clearly demonstrates that not only is TLPD with major vascular resection feasible and safe but that it can achieve results that are similar in morbidity and mortality as well as oncologic outcome compared to patients undergoing OPD with major vascular resection.

Similar content being viewed by others
Abbreviations
- TLPD:
-
Total laparoscopic pancreaticoduodenectomy
- OPD:
-
Open pancreaticoduodenectomy
- PD:
-
Pancreaticoduodenectomy
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- SD:
-
Standard deviation
- PV:
-
Portal vein
- SMV:
-
Superior mesenteric vein
References
Lujan J, Valero G, Hernandez Q, Sanchez A, Frutos MD, Parrilla P. Randomized clinical trial comparing laparoscopic and open surgery in patients with rectal cancer. Br J Surg. 2009;96:982–989.
Venkat R, Edil BH, Schulick RD, Lidor AO, Makary MA, Wolfgang CL. Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique: a systematic review and meta-analysis. Ann Surg. 2012 Jun;255(6):1048-59.
Croome K, Yamashita, M. Laparoscopic vs Open Hepatic Resection for Benign and Malignant Tumors: An Updated Meta-Analysis. Archives of Surgery 2010;145(11):1109-1118.
Kendrick ML, Cusati D. Total laparoscopic pancreaticoduodenectomy: feasibility and outcome in an early experience. Arch Surg. 2010 Jan;145(1):19-23.
Asbun HJ, Stauffer JA. Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the Accordion Severity Grading System. J Am Coll Surg. 2012 Dec;215(6):810-9.
Palanivelu C, Rajan PS, Rangarajan M, Vaithiswaran V, Senthilnathan P, Parthasarathi R et al. (2009) Evolution in techniques of laparoscopic pancreaticoduodenectomy: a decade long experience from a tertiary center. J Hepatobiliary Pancreat Surg 16:731–740.
Buchs NC, Addeo P, Bianco FM, et al. Robotic versus open pancreaticoduodenectomy: a comparative study at a single institution. World J Surg 2011;35:2739e2746.
Zeh HJ, Zureikat AH, Secrest A, et al. Outcomes after robot-assisted pancreaticoduodenectomy for periampullary lesions. Ann Surg Oncol 2012;19:864e870.
Gagner M, Pomp A: Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 1994; 8:408-410.
Yekebas EF, Bogoevski D, Cataldegirmen G, Kunze C, Marx A, Vashist YK et al. (2008) En bloc vascular resection for locally advanced pancreatic malignancies infiltrating major blood vessels: perioperative outcome and long-term survival in 136 patients. Ann Surg 247:300– 309.
Muller SA, Hartel M, Mehrabi A, Welsh T, Martin DJ, Hinz U et al. (2009) Vascular resection in pancreatic cancer surgery: survival determinates. J Gastrointest Surg 13:784–792.
Kaneoka Y, Yamaguchi A, Isogai M. (2009) Portal or superior mesenteric vein resection for pancreatic head adenocarcinoma: prognostic value of the length of venous resection. Surgery 145:417–425.
Martin RCG, Scoggins CR, Egnatashvili V, Staley CA, McMasters KM, Kooby DA. (2009) Arterial and venous resection for pancreatic adenocarcinoma: operative and long-term outcomes. Arch Surg144:154–159.
Kendrick ML, Sclabas GM. Major venous resection during total laparoscopic pancreaticoduodenectomy. HPB (Oxford). 2011 Jul;13(7):454-8
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009; 250(2):187-96.
Breitenstein S, DeOliveira ML, Raptis DA, et al. Novel and simple preoperative score predicting complications after liver resection in noncirrhotic patients. Ann Surg 2010; 252(5):726-34.
Tempero MA, Arnoletti JP, Behrman SW, Ben-Josef E, Benson 3rd AB, Casper ES, et al. Pancreatic adenocarcinoma, version 2.2012: featured updates to the NCCN Guidelines. JNCCN. 2012;10(6):703–13.
Howard TJ, Krug JE, Yu J, et al. A margin-negative R0 resection accomplished with minimal postoperative complications is the surgeon’s contribution to long-term survival in pancreatic cancer. J Gastrointest Surg 2006;10:1338e1345; discussion 1345_1336.
Pawlik TM, Gleisner AL, Cameron JL, et al. Prognostic relevance of lymph node ratio following pancreaticoduodenectomy for pancreatic cancer. Surgery 2007;141:610e618.
Kuroki T, Adachi T, Okamoto T, Kanematsu T. A non-randomized comparative study of laparoscopy-assisted pancreaticoduodenectomy and open pancreaticoduodenectomy. Hepatogastroenterology. 2012 Mar-Apr;59(114):570-3.
Chalikonda S, Aguilar-Saavedra JR, Walsh RM. Laparoscopic robotic-assisted pancreaticoduodenectomy: a case-matched comparison with open resection. Surg Endosc. 2012 Sep;26(9):2397-402.
Conflict of Interest
None of the authors have any conflict of interest to disclose. The manuscript did not receive any funding.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussant
Dr. R Matthew Walsh (Cleveland Heights, OH):
This study represents a great achievement in laparoscopic vein resection with laparoscopic Whipple procedure. It compares the results of one outstanding laparoscopic surgeon with his colleagues of equally outstanding success with open resections.
I have a few questions:
1. Can you readily tell that a vein resection needs to be done during laparoscopic dissection since imaging may be unreliable and some patients had neoadjuvant treatments? Did you compare pathologic vein involvement to be sure it is not over utilized?
2. Given the results of the NSQIP HPB demonstration project show nationally poor outcomes in adopting lap Whipple procedures, when in the learning curve should this be considered and what did you learn from the four patients you could not reconstruct as your own patient selection criteria?
3. The time to reconstruct in your expert hands was twice that of open. That did not change the outcomes here, but is that an important outcome measure for those embarking on this procedure?
Closing Discussant
Dr. Croome
Thank you Dr. Walsh for your comments and insightful questions.
It is our opinion that the magnification and fine dissection afforded by laparoscopic approaches enhances the intraoperative assessment of vascular involvement. Our pathologists do not consistently report confirmation of vascular invasion. Based on preoperative imaging and intraoperative assessment, we recommend vein resection for all patients with tumor adherence to avoid dissemination of tumor.
The learning curve for minimally invasive pancreaticoduodenectomy is quite long secondary to the advanced skills of resection and reconstruction required. The addition of a complex vascular resection and reconstruction certainly increases the difficulty. We recommend that laparoscopic major vascular resection be attempted only after considerable experience in open and laparoscopic pancreaticoduodenectomy as well as open major vascular resection and reconstruction. Conversion to an open approach should not be considered a complication, but rather sound clinical judgment to assure the best possible outcome for any given patient. In this study, the four patients were converted to open for either expected difficult reconstruction of the pancreatic anastomosis or vascular reconstruction and occurred at various stages of our learning curve.
The duration of reconstruction, and therefore clamp time, was longer for the laparoscopic group. This not only may be due to the learning curve of a new approach but also may be attributed to the greater time required to reconstruct using a long bovine pericardial patch venorrhaphy. We identified no complications that could be attributed to a longer clamp time.
Rights and permissions
About this article
Cite this article
Croome, K.P., Farnell, M.B., Que, F.G. et al. Pancreaticoduodenectomy with Major Vascular Resection: a Comparison of Laparoscopic Versus Open Approaches. J Gastrointest Surg 19, 189–194 (2015). https://doi.org/10.1007/s11605-014-2644-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2644-8