Abstract
Background
Revision of a failed laparoscopic fundoplication carries higher risk of complication and lower chance of success compared to the original surgery. Transoral incisionless fundoplication (TIF) may be an endoscopic alternative for select GERD patients without need of a moderate/large hiatal hernia repair. The aim of this study was to assess feasibility, efficacy, and safety of TIF 2.0 after failed laparoscopic Nissen or Toupet fundoplication (TIFFF).
Methods
This is a multicenter retrospective cohort study of patients who underwent TIFFF between September 2017 and December 2020 using TIF 2.0 technique (EsophyX Z/Z+) performed by gastroenterologists and surgeons. Patients were included if they had (1) recurrent GERD symptoms, (2) pathologic reflux based upon pH testing or Grade C/D esophagitis or Barrett’s esophagus, and (3) hiatal hernia ≤ 2 cm. The primary outcome was improvement in GERD Health-Related Quality of Life (GERD-HRQL) post-TIFFF. The TIFFF cohort was also compared to a similar surgical re-operative cohort using propensity score matching.
Results
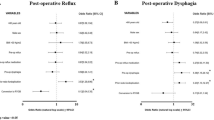
Twenty patients underwent TIFFF (median 4.1 years after prior fundoplication) and mean GERD-HRQL score improved from 24.3 ± 22.9 to 14.75 ± 21.6 (p = 0.014); mean Reflux Severity Index (RSI) score improved from 14.1 ± 14.6 to 9.1 ± 8.0 (p = 0.046) with 8/10 (80%) of patients with normal RSI (< 13) post-TIF. Esophagitis healed in 78% of patients. PPI use decreased from 85 to 55% with 8/20 (45%) patients off of PPI. Importantly, mean acid exposure time decreased from 12% ± 17.8 to 0.8% ± 1.1 (p = 0.028) with 9/9 (100%) of patients with normalized pH post-TIF. There were no statistically significant differences in clinical efficacy outcomes between TIFFF and surgical revision, but TIFFF had significantly fewer late adverse events.
Conclusion
Endoscopic rescue with TIF is a safe and efficacious alternative to redo laparoscopic surgery in symptomatic patients with appropriate anatomy and objective evidence of persistent or recurrent reflux.

Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- GERD:
-
Gastroesophageal reflux disease
- GERD-HRQL:
-
GERD Health-Related Quality of Life
- LNF:
-
Laparoscopic Nissen fundoplication
- PPI:
-
Proton pump inhibitor
- RSI:
-
Reflux Symptom Index
- TIF:
-
Transoral incisionless fundoplication
- TIFF:
-
Transoral incisionless fundoplication after failed fundoplication
References
Richter JE, Rubenstein JH (2018) Presentation and epidemiology of gastroesophageal reflux disease. Gastroenterology 154:267–276
Waring JP, Hunter JG, Oddsdottir M, Wo J, Katz E (1995) The preoperative evaluation of patients considered for laparoscopic antireflux surgery. Am J Gastroenterol 90:35–38
Csendes A, Orellana O, Cuneo N, Martinez G, Figueroa M (2019) Long-term (15-year) objective evaluation of 150 patients after laparoscopic Nissen fundoplication. Surgery 166:886–894
Mickevičius A, Endzinas Z, Kiudelis M, Jonaitis L, Kupčinskas L, Pundzius J, Maleckas A (2013) Influence of wrap length on the effectiveness of Nissen and Toupet fundoplications: 5-year results of prospective, randomized study. Surg Endosc 27:986–991
Furnee EJ, Draaisma WA, Broeders IAM, Gooszen HG (2009) Surgical reintervention after failed antireflux surgery: a systematic review of the literature. J Gastrointest Surg 13:1539–1549
Del Campo SEM, Mansfield SA, Suzo AJ, Hazey JW, Perry KA (2017) Laparoscopic redo fundoplication improves disease-specific and global quality of life following failed laparoscopic or open fundoplication. Surg Endosc 31:4649–4655
Grover BT, Kothari SN (2015) Reoperative antireflux surgery. Surg Clin North Am 95:629–640
Frantzides CT, Carlson MA (1997) Laparoscopic redo nissen fundoplication. J Laparoendosc Adv Surg Tech A 7:235–239
Munie S, Nasser H, Gould JC (2019) Salvage options for fundoplication failure. Curr Gastroenterol Rep 21:41
Van Beek DB, Auyang ED, Soper NJ (2011) A comprehensive review of laparoscopic redo fundoplication. Surg Endosc 25:706–712
Al Hashmi AW, de Chambrun GP, Souche R, Bertrand M, Blasi VD, Jacques E, Azagra S, Fabre JM, Borie F, Prudhomme M, Nagot N, Navarro F, Panaro F (2019) A retrospective multicenter analysis on redo-laparoscopic anti-reflux surgery: conservative or conversion fundoplication? Surg Endosc 33:243–251
Yadlapati R, Hungness ES, Pandolfino JE (2018) Complications of antireflux surgery. Am J Gastroenterol 113:1137–1147
Stefanidis D, Navarro F, Augenstein VA, Gersin KS, Heniford BT (2012) Laparoscopic fundoplication takedown with conversion to Roux-en-Y gastric bypass leads to excellent reflux control and quality of life after fundoplication failure. Surg Endosc 26:3521–3527
Singhal S, Kirkpatrick DR, Masuda T, Gerhardt J, Mittal SK (2018) Primary and redo antireflux surgery: outcomes and lessons learned. J Gastrointest Surg 22:177–186
Ihde GM (2020) The evolution of TIF: transoral incisionless fundoplication. Therap Adv Gastroenterol 13:1–16
Bell RCW, Cadiere GB (2011) Transoral rotation esophagogastric fundoplication: technical, anatomical, and safety considerations. Surg Endosc 25:2387–2399
Testoni S, Hassan C, Mazzoleni G, Antonelli G, Fanti L, Passaretti S, Correale L, Cavestro GM, Testoni PA (2021) Long-term outcomes of transoral incisionless fundoplication for gastro-esophageal reflux disease: systematic review and meta-analysis. Endosc Int Open. https://doi.org/10.1055/a-1322-2209
Velanovich V (2007) The development of the GERD-HRQL symptom severity instrument. Dis Esophagus 20:130–134
Belafsky PC, Postma GN, Koufman JA (2002) Validity and reliability of the reflux symptom index (RSI). J Voice 16:274–277
Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71:446–454
Funk LM, Kanji A, Melvin WS, Perry KA (2014) Elective antireflux surgery in the US: an analysis of national trends in utilization and inpatient outcomes from 2005 to 2010. Surg Endosc 28:1712–1719
Patti MG, Allaix ME, Fisichella PM (2015) Analysis of the causes of failed antireflux surgery and the principles of treatment a review. JAMA Surg 150:585–590
Carlson MA, Frantzides CT (2001) Complications and results of primary minimally invasive antireflux procedures: a review of 10,735 reported cases. J Am Coll Surg 193:428–439
Symons NR, Purkayastha S, Dillemans B, Athanasiou T, Hanna GB, Darzi A, Zacharakis E (2011) Laparoscopic revision of failed antireflux surgery: a systematic review. Am J Surg 202:336–343
Bell RCW, Hufford RJ, Fearon J, Freeman KD (2013) Revision of failed traditional fundoplication using EsophyX transoral fundoplication. Surg Endosc. https://doi.org/10.1007/s00464-012-2542-7
Bell RCW, Barnes WE, Carter B, Sewell RW, Mavrelis PG, Ihde GM, Hoddinott KM, Fox MA, Freeman KD, Gunsberger T, Hausmann MG, Dargis D, Gill BD, Wilson E, Trad KS (2014) Transoral incisionless fundoplication: 2-year results from the prospective multicenter US Study. Am Surg 80:1093–1105
Hunter JG, Kahrilas PJ, Bell RCW, Wilson EB, Trad KS, Dolan JP, Perry KA, Oelschlager BK, Soper NJ, Snyder BE, Burch MA, Melvin WS, Reavis KM, Turgeon DG, Hungness ES, Diggs BS (2015) Efficacy of transoral fundoplication vs omeprazole for treatment of regurgitation in a randomized controlled trial. Gastroenterology 148:324–333
Trad KS, Simoni G, Barnes WE, Shughoury AB, Raza M, Heise JA, Turgeon DG, Fox A, Mavrelis PG (2014) Efficacy of transoral fundoplication for treatment of chronic gastroesophageal reflux disease incompletely controlled with high-dose proton-pump inhibitors therapy: a randomized, multicenter, open label, crossover study. BMC Gastroenterol 14:174
Yadlapati R, Masihi M, Gyawali CP, Carlson DA, Kahrilas PJ, Nix BD, Jain A, Triggs JR, Vaezi MF, Kia L, Kaizer A, Pandolfino JE (2021) Ambulatory reflux monitoring guides proton pump inhibitor discontinuation in patients with gastroesophageal reflux symptoms: a clinical trial. Gastroenterology 160:174–182
Lord RVN, Kaminski A, Oberg S, Bowrey DJ, Hagen JA, DeMeester SR, Sillin LF, Peters JH, Crookes PF, DeMeester TR (2002) Absence of gastroesophageal reflux disease in a majority of patients taking acid suppression medications after Nissen fundoplication. J Gastrointest Surg 6:3–9
Ihde G, Pena C, Scitern C, Brewer S (2019) pH Scores in hiatal repair with transoral incisionless fundoplication. JSLS 23(e2018):00087
Ashfaq A, Rhee HK, Harold KL (2014) Revision of failed transoral incisionless fundoplication by subsequent laparoscopic Nissen fundoplication. World J Gastroenterol 20:17115–17119
Bell RC, Kurian AA, Freeman KD (2015) Laparoscopic anti-reflux revision surgery after transoral incisionless fundoplication is safe and effective. Surg Endosc 29:1746–1752
Acknowledgements
TIF Research Consortium: Cheguevara Afaneh, Daniella Assis, Christy Dunst, Jon Gabrielsen, Olaya Brewer Gutierrez, Glen Ihde, Harshit Khara, Jennifer Kolb, Michael Marohn, Jason Samarasena, and Erik Wilson.
Funding
This investigator-initiated study was supported in part by the Johns Hopkins Heartburn Center (TIF Registry) and Endogastric Solutions. Endogastric Solutions was not involved in the design, conduct, or analysis of the data and preparation of the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
GG and AC participated in the study conception and design; JG, RZ, MM, PJ, NT, BKA, DD, NTN, and KC participated in the acquisition of data; GG participated in the analysis of data; GG and MD participated in the interpretation of data; GG and AC participated in the drafting of manuscript; DD, MD, and RZ participated in the revision of manuscript; MC and RS participated in the final revision and approval of manuscript.
Corresponding author
Ethics declarations
Disclosures
Michael Murray is a Consultant for Endogastric solutions. Peter Janu is a Consultant and speaker in Endogastric Solutions, Ethicon, J&J, and Olympus. Barham K. Abu-Dayyeh is a Consultant for Endogenex, Endo-TAGSS, Metamodix, and BFKW; receives Consulting and grant/research support from USGI, Cairn Diagnostics, Aspire Bariatrics, and Boston Scientific; speaker in Olympus and Johnson and Johnson; and receives Speaker and rant/research support from Medtronic and Endogastric solutions and research support from Apollo Endosurgery, and Spatz Medical. David Diehl is a Consultant and speaker for Olympus, Boston Scientific, Cook Medical, Cernostics, GI Supply, Lumendi, Microtek, Actuated Medical, and Pentax. Rasa Zarnegar is a Consultant for Bard. Ninh T. Nguyen is a Speaker for Endogastric Solutions and Olympus. Kenneth J. Chang is a Consultant for Apollo, Boston Scientific, Cook Medical, Erbe, Endogastric Solutions, Mauna Kea, Medtronic, Olympus, Ovesco Endoscopy, and Pentax. Marcia Irene Canto receives research grant from Endogastric Solutions. Reem Sharaiha is a Consultant for Boston scientific, Olympus, and Cook Medical. Drs. Gaurav Ghosh, Alyssa Choi, Mohamad Dbouk, Jacques Greenberg, and Nirav Thosani have no conflicts of interest or financial ties to disclose.
Ethical approval
Granted for this study by each center’s respective Institutional Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of TIF Research Consortium have been listed in acknowledgements.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ghosh, G., Choi, A.Y., Dbouk, M. et al. Transoral incisionless fundoplication for recurrent symptoms after laparoscopic fundoplication. Surg Endosc 37, 3701–3709 (2023). https://doi.org/10.1007/s00464-023-09880-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09880-4