Abstract
Introduction
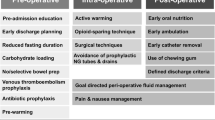
Enhanced recovery after surgery (ERAS) programs provide a framework for optimal perioperative care to improve post-operative outcomes following surgical procedures. However, there is no consensus regarding an ERAS protocol following foregut surgery. The purpose of this study was to develop an ERAS protocol for these patients and determine whether they improved outcomes.
Methods
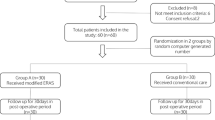
An IRB approved prospectively maintained database was retrospectively reviewed for all patients undergoing benign minimally invasive foregut surgery from October 2018 to January 2020. All patients were entered into the ACS risk calculator to determine their predicted rate of complications and length of stay for comparison between the ERAS and control groups. Propensity matching was used to compare post-ERAS implementation to pre-ERAS implementation patients. Firth logistic and Poisson regression analysis were used to assess the rate of complications and length of stay among the different groups of patients.
Results
There were 255 patients (60 Post-ERAS, 195 Pre-ERAS) who underwent foregut operations and met inclusion criteria. ERAS was implemented, and patients were then subdivided based on those who completed ERAS (44) and those who deviated from the protocol (16). Propensity matching analysis was performed to compare the different cohorts and showed ERAS patients had 41% decreased odds of complications and 33% reduction in length of stay compared to pre-ERAS patients. Completion of the ERAS protocol resulted in even further reductions in odds of complication and length of stay compared to patients who deviated from the protocol.
Conclusions
ERAS has shown to improve perioperative outcomes, but there is limited literature supporting the use of ERAS in foregut surgery. Usage of an ERAS protocol can decrease complications and reduce the length of stay in patients.





Similar content being viewed by others
References
Slim K, Delaunay L, Joris J, Léonard D, Raspado O, Chambrier C, Ostermann S (2016) How to implement an enhanced recovery program? proposals from the francophone group for enhanced recovery after surgery (GRACE). J Visc Surg 153(6):S45–S49
Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, Nygren J, Hausel J, Soop M, Andersen J, Kehlet H (2005) Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 24(3):466–477
Martin TD, Lorenz T, Ferraro J, Chagin K, Lampman RM, Emery KL, Zurkan JE, Boyd JL, Montgomery K, Lang RE, Vandewarker JF (2016) Newly implemented enhanced recovery pathway positively impacts hospital length of stay. Surg Endosc 30(9):4019–4028
Šerclová Z, Dytrych P, Marvan J, Nová K, Hankeová Z, Ryska O, Šlégrová Z, Burešová L, Trávníková L, Antoš F (2009) Fast-track in open intestinal surgery: prospective randomized study (Clinical Trials Gov Identifier no NCT00123456). Clin Nutr 28(6):618–624
Basse L, Raskov HH, Hjort Jakobsen D, Sonne E, Billesbølle P, Hendel H, Rosenberg J, Kehlet H (2002) Accelerated postoperative recovery programme after colonic resection improves physical performance, pulmonary function and body composition. J Br Surg 89(4):446–453
Damani T, Ballantyne G (2020) Robotic foregut surgery. Surg Clin 100(2):249–264
Xie J, Vatsan MS, Gangemi A (2021) Laparoscopic versus robotic-assisted Heller myotomy for the treatment of achalasia: a systematic review with meta-analysis. Int J Med Robot Comput Assist Surg 24:e2253
McKinley SK, Dirks RC, Walsh D, Hollands C, Arthur LE, Rodriguez N, Jhang J, Abou-Setta A, Pryor A, Stefanidis D, Slater BJ (2021) Surgical treatment of GERD: systematic review and meta-analysis. Surg Endosc 2:1–29
Luo RB, Montalvo D, Suzuki T, Sandler BJ, Jacobsen GR, Horgan S (2016) Complications of robotic foregut surgery: risks and advantages. Minerva Chir 72(1):44–60
Soliman BG, Nguyen DT, Chan EY, Chihara RK, Meisenbach LM, Graviss EA, Kim MP (2020) Robot-assisted hiatal hernia repair demonstrates favorable short-term outcomes compared to laparoscopic hiatal hernia repair. Surg Endosc 34(6):2495–2502
ACS NSQIP Surgical Risk Calculator (2020) https://riskcalculator.facs.org/RiskCalculator/: Accessed 16 Feb 2020
Thorell A, MacCormick AD, Awad S, Reynolds N, Roulin D, Demartines N, Vignaud M, Alvarez A, Singh PM, Lobo DN (2016) Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg 40(9):2065–2083
Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N, Rockall TA, Young-Fadok TM, Hill AG, Soop M, de Boer HD (2019) Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS®) society recommendations: 2018. World J Surg 43(3):659–695
Low DE, Allum W, De Manzoni G, Ferri L, Immanuel A, Kuppusamy M, Law S, Lindblad M, Maynard N, Neal J, Pramesh CS (2019) Guidelines for perioperative care in esophagectomy: enhanced recovery after surgery (ERAS®) society recommendations. World J Surg 43(2):299–330
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205
Clavien PA, Barkun J, De Oliveira ML, Vauthey JN, Dindo D, Schulick RD, De Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Lemanu DP, Singh PP, Berridge K, Burr M, Birch C, Babor R, MacCormick AD, Arroll B, Hill AG (2013) Randomized clinical trial of enhanced recovery versus standard care after laparoscopic sleeve gastrectomy. J Br Surg 100(4):482–489
Wind J, Hofland J, Preckel B, Hollmann MW, Bossuyt PM, Gouma DJ, van Berge Henegouwen MI, Fuhring JW, Dejong CH, van Dam RM, Cuesta MA (2006) Perioperative strategy in colonic surgery; laparoscopy and/or fast track multimodal management versus standard care (LAFA trial). BMC Surg 6(1):1–8
Basse L, Jakobsen DH, Billesbølle P, Werner M, Kehlet H (2000) A clinical pathway to accelerate recovery after colonic resection. Ann Surg 232(1):51
Alanazi AA (2014) Reducing anxiety in preoperative patients: a systematic review. Br J Nurs 23(7):387–393
Ronco M, Iona L, Fabbro C, Bulfone G, Palese A (2012) Patient education outcomes in surgery: a systematic review from 2004 to 2010. Int J Evid Based Healthc 10(4):309–323
Stacey D, Taljaard M, Dervin G, Tugwell P, O’Connor AM, Pomey MP, Boland L, Beach S, Meltzer D, Hawker G (2016) Impact of patient decision aids on appropriate and timely access to hip or knee arthroplasty for osteoarthritis: a randomized controlled trial. Osteoarthr Cartil 24(1):99–107
Granziera E, Guglieri I, Del Bianco P, Capovilla E, Ciccarese AA, Kilmartin D, Manfredi V, De Salvo GL (2013) A multidisciplinary approach to improve preoperative understanding and reduce anxiety: a randomised study. Eur J Anaesthesiol (EJA) 30(12):734–742
Kurz A, Sessler DI, Lenhardt R (1996) Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. N Engl J Med 334(19):1209–1216
Scott EM, Buckland R (2006) A systematic review of intraoperative warming to prevent postoperative complications. AORN J 83(5):1090–1113
Nelson R, Edwards S, Tse B (2004) Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD004929.pub2
Rao W, Zhang X, Zhang J, Yan R, Hu Z, Wang Q (2011) The role of nasogastric tube in decompression after elective colon and rectum surgery: a meta-analysis. Int J Colorectal Dis 26(4):423–429
Andersen HK, Lewis SJ, Thomas S (2006) Early enteral nutrition within 24h of colorectal surgery versus later commencement of feeding for postoperative complications. Cochrane Database Syst. https://doi.org/10.1002/14651858.CD004080.pub2
Kim MP, Chan EY, Meisenbach LM, Dumitru R, Brown JK, Masud FN (2018) Enhanced recovery after thoracic surgery reduces discharge on highly dependent narcotics. J Thorac Dis 10(2):984
Kim MP, Godoy C, Nguyen DT, Meisenbach LM, Chihara R, Chan EY, Graviss EA (2020) Preemptive pain-management program is associated with reduction of opioid prescriptions after benign minimally invasive foregut surgery. J Thorac Cardiovasc Surg 159(2):734–744
Adamina M, Guller U, Weber WP, Oertli D (2006) Propensity scores and the surgeon. J Br Surg 93(4):389–394
Cepeda MS, Boston R, Farrar JT, Strom BL (2003) Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am J Epidemiol 158(3):280–287
Joffe MM, Rosenbaum PR (1999) Invited commentary: propensity scores. Am J Epidemiol 150(4):327–333
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Steven Leeds is a consultant for Ethicon and Boston Scientific. Dr. Marc Ward is a consultant for Boston Scientific. Drs. Madeline Rasmussen, Edward Whitfield, Bola Aladegbami, and Gerald Ogola have no conflict of interest to financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rasmussen, M.L., Leeds, S.G., Whitfield, E.P. et al. Enhanced recovery after surgery (ERAS) decreases complications and reduces length of stay in foregut surgery patients. Surg Endosc 37, 2842–2850 (2023). https://doi.org/10.1007/s00464-022-09806-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09806-6