Abstract
Background
Femoral hernia (FH) is traditionally treated by open surgery (OS). Laparoscopic treatment has also shown good results in treating FH. However, there have been few comparative studies of these two techniques. Therefore, our aim was to compare the outcomes of open and laparoscopic surgical FH treatment.
Methods
Adult patients with primary unilateral FH undergoing OS or transabdominal preperitoneal (TAPP) hernia repair at our hospital from January 2013 to June 2018 were included in this study. Patients with history of abdominal surgery, contraindications to general anesthesia and those not wishing to receive general anesthesia received OS. Demographics, operation details and complications were compared retrospectively between the two groups.
Results
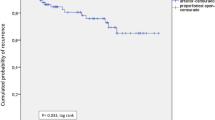
A total of 132 patients were recruited to the study, 62 and 70 of whom underwent OS and TAPP, respectively. Compared to OS group, the TAPP group had a significantly shorter hospital stay (3.0 vs. 2.0 days, respectively, P < 0.05) and a lower postoperative pain score (3.0 vs. 1.0, P < 0.05), and took less time to return to normal activities (13.0 vs. 6.0 days, respectively, P < 0.05). The overall complication rates were equivalent between the groups (10 vs. 9.7%, OR = 1.037, 95% CI 0.329–3.270).
Conclusions
Both laparoscopic and open surgery appear to be safe and effective in a cohort of patients with femoral hernia and laparoscopic surgery might offer some advantages in reducing length of hospital stay, lower postoperative pain score and quicker return to activities.
Graphical abstract

Similar content being viewed by others
References
Burcharth J, Pedersen M, Bisgaard T, Pedersen C, Rosenberg J (2013) Nationwide prevalence of groin hernia repair. PLoS ONE 8(1):e54367
Dahlstrand U, Wollert S, Nordin P, Sandblom G, Gunnarsson U (2009) Emergency femoral hernia repair: a study based on a national register. Ann Surg 249(4):672–676
Humes DJ, Radcliffe RS, Camm C, West J (2013) Population-based study of presentation and adverse outcomes after femoral hernia surgery. Br J Surg 100(13):1827–1832
Beadles CA, Meagher AD, Charles AG (2015) Trends in emergent hernia repair in the United States. JAMA Surg 150(3):194–200
Koch A, Edwards A, Haapaniemi S, Nordin P, Kald A (2005) Prospective evaluation of 6895 groin hernia repairs in women. Br J Surg 92(12):1553–1558
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22(1):1–65
Fitzgibbons RJ Jr, Giobbie-Hurder A, Gibbs JO, Dunlop DD, Reda DJ, McCarthy M Jr, Neumayer LA, Barkun JS, Hoehn JL, Murphy JT, Sarosi GA Jr, Syme WC, Thompson JS, Wang J, Jonasson O (2006) Watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomized clinical trial. JAMA Surg 295(3):285–292
Andresen K, Bisgaard T, Kehlet H, Wara P, Rosenberg J (2014) Reoperation rates for laparoscopic vs open repair of femoral herniasin Denmark: a nationwide analysis. JAMA Surg 49(8):853–857
Chen D, Su N, Wang W, Zhang Z, Guo M, Lu C, Zhang H (2018) Laparoscopic transabdominal preperitoneal technique versus open surgery with the ULTRAPRO Hernia System for the repair of female primary femoral hernias-an observational retrospective study. Medicine (Baltimore) 97(49):e13575
Pélissier EP, Blum D, Marre P, Damas JM (2001) Inguinal hernia: a patch covering only the myopectineal orifice is effective. Hernia 5(2):84–87
Ferzli GS, Fitzgibbons RJ, Fortelny RH, Klinge U, Kockerling F, Kuhry E, Kukleta J, Lomanto D, Misra MC, Montgomery A, Morales-Conde S, Reinpold W, Rosenberg J, Sauerland S, Schug-Pass C, Singh K, Timoney M, Weyhe D, Chowbey P (2009) Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc 25(9):2773–2843
Hernández-Irizarry R, Zendejas B, Ramirez T, Moreno M, Ali SM, Lohse CM, Farley DR (2012) Trends in emergent inguinal hernia surgery in Olmsted County, MN: a population-based study. Hernia 16(4):397–403
Kurt N, Oncel M, Ozkan Z, Bingul S (2003) Risk and outcome of bowel resection in patients with incarcerated groin hernias: retrospective study. World J Surg 27(6):741–743
Suppiah A, Gatt M, Barandiaran J, Heng MS, Perry EP (2007) Outcomes of emergency and elective femoral hernia surgery in four district general hospitals: a 4-year study. Hernia 11(6):509–512
de Guzma´n CA-R, Picazo-Yeste J, Tenı´as-Burillo JM, Moreno-Sanz C, (2013) Improved outcomes of incarcerated femoral hernia: a multivariate analysis of predictive factors of bowel ischemia and potential impact on postoperative complication. Am J Surg 205(2):188–193
Scheuermann U, Niebisch S, Lyros O, Jansen-Winkeln B, Gockel I (2017) Transabdominal preperitoneal (TAPP) versus lichtenstein operation for primary inguinal hernia repair—a systematic review and meta-analysis of randomized controlled trials. BMC Surg 17(1):55
Köninger J, Redecke J, Butters M (2004) Chronic pain after hernia repair: a randomized trial comparing shouldice lichtenstein and TAPP. Langenbecks Arch Surg 389(5):361–365
Li J, Wang X, Feng X, Gu Y, Tang R (2013) Comparison of open and laparoscopic preperitoneal repair of groin hernia. Surg Endosc 27(12):4702–4710
Singh AN, Bansal VK, Misra MC, Kumar S, Rajeshwari S, Kumar A, Sagar R, Kumar, (2012) Testicular functions, chronic groin pain, and quality of life after laparoscopic and open mesh repair of inguinal hernia: a prospective randomized controlled trial. Surg Endosc 26(5):1304–1317
Eklund A, Montgomery A, Bergkvist L, Rudberg C (2010) Chronic pain 5 years after randomized comparison of laparoscopic and lichtenstein inguinal hernia repair. Br J Surg 97(4):600–608
Collaboration EHT (2002) Repair of groin hernia with synthetic mesh: meta-analysis of randomized controlled trials. Ann Surg 235(3):322–332
Douek M, Smith G, Oshowo A, Stoker DL, Wellwood JM (2003) Prospective randomised controlled trial of laparoscopic versus open inguinal hernia mesh repair: five year follow up. BMJ 326(7397):1012–1013
Pisanu A, Podda M, Saba A, Porceddu G, Uccheddu A (2015) Meta-analysis and review of prospective randomized trials comparing laparoscopic and lichtenstein techniques in recurrent inguinal hernia repair. Hernia 19(3):355–366
Johansson B, Hallerbäck B, Glise H, Anesten B, Smedberg S, Román J (1999) Laparoscopic mesh versus open preperitoneal mesh versus conventional technique for inguinal hernia repair. Ann Surg 230(2):225–231
Gong K, Zhang N, Lu Y, Zhu B, Zhang Z, Du D, Zhao X, Jiang H (2011) Comparison of the open tension-free mesh-plug, transabdominal preperitoneal (TAPP), and totally extraperitoneal (TEP) laparoscopic techniques for primary unilateral inguinal hernia repair: a prospective randomized controlled trial. Surg Endosc 25(1):234–239
McCormack K, Scott NW, Go PM, Ross S, Grant AM (2003) EU hernia trialists collaboration laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev 1:001785
Pironi D, Palazzini G, Panarese A, La Gioia G, Vendettuoli M, Romani AM, Filippini A (2008) Open mesh technique versus laparoscopic transabdominal preperitoneal (TAPP) approach in inguinal hernia repair our experience. G Chir 29(11–12):497–504
Lyu Y, Cheng Y, Wang B, Du W, Xu Y (2020) Comparison of endoscopic surgery and lichtenstein repair for treatment of inguinal hernias: a network meta-analysis. Medicine (Baltimore) 99(6):e19134
Reddy VM, Sutton CD, Bloxham L, Garcea G, Ubhi SS, Robertson GS (2007) Laparoscopic repair of direct inguinal hernia: a new technique that reduces the development of postoperative seroma. Hernia 11(5):393–396
Köckerling F, Bittner R, Jacob DA, Seidelmann L, Keller T, Adolf D, Kraft B, Kuthe A (2015) TEP versus TAPP: comarison of the perioperative outcome in 17,587 patients with a primary unilateral inguinal hernia. Surg Endosc 29(12):3750–3760
Köckerling F, Stechemesser B, Hukauf M, Kuthe A, Schug-Pass C (2016) TEP versus lichtenstein: which technique is better for the repair of primary unilateral inguinal hernias in men? Surg Endosc 30(8):3304–3313
Schmedt CG, Sauerland S, Bittner R (2005) Comparison of endoscopic procedures vs lichtenstein and other open meshtechniques for inguinal hernia repair: a meta-analysis of randomizedcontrolled trials. Surg Endosc 19(2):188–199
Bittner R, Sauerland S, Schmedt C-G (2005) Comparison of endoscopic techniques vs shouldice and other open nonmesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials. Surg Endosc 19(5):605–615
Garg P, Rajagopal M, Varghese V, Ismail M (2009) Laparoscopic total extraperitoneal inguinal hernia repair with nonfixation of the mesh for 1692 hernias. Surg Endosc 23(6):1241–1245
Teng YJ, Pan SM, Liu YL, Yang KH, Zhang YC, Tian JH, Han JX (2011) A meta-analysis of randomized controlled trials offixation versus nofixation of mesh in laparoscopic total extraperitonealinguinal hernia repair. Surg Endosc 25(9):2849–2858
Köckerling F, Bittner R, Adolf D, Fortelny R, Niebuhr H, Mayer F, Schug-Pass C (2018) Seroma following transabdominal preperitoneal patch plasty (tapp): incidence, risk factors, and preventive measures. Surg Endosc 32(5):2222–2231
Bjurstrom MF, Nicol AL, Amid PK, Chen DC (2014) Pain control following inguinal herniorrhaphy: current perspectives. J Pain Res 7:277–290
Aasvang EK, Gmaehle E, Hansen JB, Gmaehle B, Forman JL, Schwarz J, Bittner R, Kehlet H (2010) Predictive risk factors for persistent postherniotomy pain. Anesthesiology 112(4):957–969
Aasvang E, Kehlat H (2005) Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth 95(1):69–76
Kumar S, Wilson RG, Nixon SJ, Macintyre IM (2002) Chronic pain after laparoscopic and open mesh repair of groin hernia. Br J Surg 89(11):1476–1479
Bower S, Moore BB, Weiss SM (1996) Neuralgia after inguinal hernia repair. Am Surg 62(8):664–667
Wijsmuller AR, Lange JF, Kleinrensink GJ, van Geldere D, Simons MP, Huygen FJ, Jeekel J, Lange JF (2007) Nerve-identifying inguinal hernia repair: a surgical anatomical study. World J Surg 31(2):414–420
Reinpold W, Schroeder AD, Schroeder M, Berger C, Rohr M, Wehrenberg U (2015) Retroperitoneal anatomy of the iliohypogastric, ilioinguinal, genitofemoral, and lateral femoral cutaneous nerve: consequences for prevention and treatment of chronic inguinodynia. Hernia 19(4):539–548
Alfieri S, Amid PK, Campanelli G, Izard G, Kehlet H, Wijsmuller AR, Di Miceli D, Doglietto GB (2011) International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia 15(3):239–249
Graham DS, MacQueen IT, Chen DC (2018) Inguinal neuroanatomy: implications for prevention of chronic postinguinal hernia pain. Int J Abdom Wall Hernia Surg 1(1):1–8
Li J, Ji Z, Li Y (2014) Comparison of laparoscopic versus open procedure in the treatment of recurrent inguinal hernia: a metaanalysis of the results. Am J Surg 207(4):602–612
Burcharth J, Andresen K, Pommergaard HC, Bisgaard T, Rosenberg J (2014) Direct inguinal hernias and anterior surgical approach are risk factors for female inguinal hernia recurrences. Langenbecks Arch Surg 399(1):71–76
Bay-Nielsen M, Kehlet H, Strand L, Malmstrøm J, Andersen FH, Wara P, Juul P, Callesen T (2001) Quality assessment of 26,304 herniorrhaphies in Denmark: a prospective nationwide study. Lancet 358(9288):1124–1128
Schmidt L, Öberg S, Andresen K, Rosenberg J (2018) Recurrence rates after repair of inguinal hernia in women: a systematic review. JAMA Surg 153(12):1135–1142
Chen J, Lv Y, Shen Y, Wang M (2010) A prospective comparison of preperitoneal tension-free open herniorrhaphy with mesh plug herniorrhaphy for the treatment of femoral hernias. Surgery 148(5):976–981
Acknowledgements
We thank Textcheck (http://www.textcheck.com), for editing the English text of a draft of this manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
JC and JL: developed the study concept, acquired, analyzed, interpreted the data, and drafted the manuscript. YS: acquired data and literature. JC and RB: acquired literature and revised the manuscript. All authors read and approved the final manuscript. Furthermore, all authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Disclosures
Drs. Jing Liu, Reinhard Bittner, Yingmo Shen and Jie Chen have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, J., Bittner, R., Shen, Y. et al. Comparison of open preperitoneal and transabdominal preperitoneal hernia repair for primary unilateral femoral hernia: a retrospective cohort study of 132 case. Surg Endosc 37, 2712–2718 (2023). https://doi.org/10.1007/s00464-022-09759-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09759-w