Abstract
Background
The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) uses the Laparoscopic colectomy Train the Trainer (Lapco TT) framework for standardization of instructor training for Hands-On surgical skills courses. The curriculum focuses on teaching structure, skills deconstruction, trainer intervention framework, and performance enhancing feedback. A halt in the in-person Lapco TT courses due to the Coronavirus Disease 2019 (COVID-19) pandemic necessitated creation of a virtual alternative. We investigated the effectiveness of this virtual course.
Methods
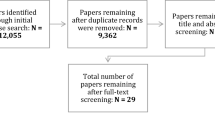
Adaptation of the in-person Lapco TT course to the virtual format retained the majority of content as well as the 4:6 instructor-to-participant ratio. The virtual platform and simulators chosen allowed maximal interactivity and ease of use. After participating in the day and one half course, participants completed an 8-item post-course survey using a 5-point Likert scale related to the training experience. In addition, they had the opportunity to provide answers to several open-ended questions regarding the course. For the survey, frequency counts provided an assessment of each item. For the open questions, qualitative analysis included determination of themes for each question. Frequency counts of each theme provided quantitative analysis.
Results
Thirty-six total participants completed a Lapco TT virtual course (six sessions of six participants). Of this number, 32 participants completed post-course surveys and questions. All the participants completing the survey would very likely or definitely (Likert scale 4, 5) recommend the course to a colleague and incorporate the teaching in their practice. The majority of participants completing open-ended questions felt the virtual course format was effective; half thought that post-course follow-up would be useful. Technical concerns were an issue using the virtual format.
Conclusion
A virtual Lapco TT course is feasible and well received by participants. It presents a potentially more cost effective option to faculty development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The origins of the laparoscopic colectomy (Lapco) teaching program date back to 2006, when the National Institute for Health and Clinical Excellence for England and Wales made a formal recommendation for the standard use of laparoscopy for colorectal surgery by appropriately trained surgeons [1]. At the time, only a small number of colorectal consultants were facile in this approach, resulting in the suspension of the recommendation until the creation of a national training initiative [1]. The National Training Program for laparoscopic colorectal surgery was therefore instituted in 2007 to address this need. Regional training centers were established for experienced consultant surgeons, and evaluation mechanisms were put in place. Validated global assessments were submitted by both trainer and trainee after each training case. Once both agreed on the quality of the operative performance, monitored videos of cases were reviewed, and clinical outcomes were collected for up to 1 year. By this method, Coleman et al. were able to demonstrate the success of this national training initiative [1].
The National Training Program in Laparoscopic Colorectal Surgery recognized the need to “improve, standardize, and benchmark the quality of training” [2]. Therefore, a “training the trainer” course, modeled after the Training the Colonoscopy Trainers course developed by the United Kingdom (UK) National Joint Advisory Group for Gastrointestinal Endoscopy, was designed and implemented starting in 2010 [2]. This curriculum focuses on teaching structure, skills deconstruction, a trainer intervention framework, and performance enhancing feedback [2]. The elements of teaching structure include a 3-part framework of a set, dialogue, and closure. Skills deconstruction, a proven model of teaching skill acquisition, includes moving surgeons from being unconsciously competent to becoming consciously competent educators [2]. The trainer intervention framework introduces the concept of the Six Steps, a six-part progression of intervention to assist a trainee who fails to progress [2]. Finally, performance enhancing feedback provides a mechanism for the delegate to improve their own as well as their learners’ skills [2]. By analyzing courses delivered over a 1-year period, Mackenzie et al. were able to show improvement over all 4 Kirkpatrick levels of training effectiveness, using both quantitative and qualitative measures [2].
The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) first began using the Lapco TT format to prepare faculty involved in its 2015 Acquisition of Data for Outcomes and Procedure Transfer (ADOPT) program [3]. Its purpose was to standardize the mentorship and teaching techniques delivered by faculty in hands-on courses as part of ADOPT. UK consultant colorectal surgeons Mark Coleman and Tom Cecil helped to introduce the program to the USA and an initial group of SAGES surgeons underwent training in 2014. Many of these initial learners completed the necessary additional work to become faculty for the Lapco TT course itself. Since then, the number of both Lapco TT-trained surgeons and faculty have increased as more ADOPT courses were given each year. To date, over 100 surgeons have participated in Lapco TT courses sponsored by SAGES [4].
Across the globe, much has been written about remote surgical teaching of medical students and surgical residents [5,6,7,8,9,10] but a paucity of literature exist related to virtual train the trainer style courses for surgeons teaching technical skills. The Coronavirus disease 2019 (COVID-19) pandemic prevented SAGES from having any face-to-face interactions in 2020, including the scheduled ADOPT program and its concomitant Lapco TT sessions for faculty development. Consequently, SAGES successfully pivoted to adapting both Lapco TT and the ADOPT course to a virtual format [11]. We decided to investigate the effectiveness of the virtual Lapco TT format as a faculty development tool.
Materials and methods
Format of virtual course and logistics
The existing live face-to-face Lapco TT course structure required several changes in order to create a virtual format that was executable. SAGES convened an ad hoc task force of three individuals to re-imagine the course into a virtual format (“Virtual TT Task Force”).
The SAGES Project 6 Technology working group minimal requirements served to guide the technology requirements for this endeavor [12]. First, the existing hands-on laparoscopic activities underwent simplification. After reviewing several models, the Virtual TT Task Force chose the EndoSim [Bolton, MA] LapEASIE-R Laparoscopic Simulator for use during the surgical hands-on portion of the course (Fig. 1). Prior to the course start, SAGES shipped learners the necessary components (i.e., laparoscopic trainer, cameras, laptop, and all additional equipment with instructions needed for setup). Participants then set up the simulator following instructions. For troubleshooting any problems, a technical support specialist was available in advance and also for one hour at the beginning of the first day of the course.
The virtual TT course faculty also received EndoSim laparoscopic trainer boxes shipped to their homes or institutions. In addition, EndoSim shipped tissue specimens to those faculty responsible for recruiting novice learners for hands-on sessions and for the practice teaching session at the end of the course. The faculty recruited these novice learners from their local institutions and/or friends and family, for ease in setup and fluidity of transitioning between learners and between portions of the novice-learner education.
Second, the Virtual TT Task Force evaluated available teleconferencing platforms for use during the virtual course. They chose Zoom [San Jose, CA] to serve this function due to its perceived advantages. They included the ability to control and optimize user participation, lock meetings, and minimize disruption. One example of the ability to minimize disruption was the use of the ‘hide all non-video participants’ function on Zoom. This allowed the faculty to be logged in for the entire course without being on video unless they were actively teaching. Zoom also allowed recording of the course, allowing clips of select courses to be used for future course iterations to expand the learning potential of each session. Additional advantages included the ability of course participants to interact via video and chat. Finally, the ability to use screen sharing allowed all participants to see the course syllabus and shared notes.
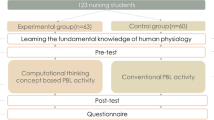
The course occurred over a two-day period. The first day focused on introducing participants to the key concepts related to the course including the set-dialogue-closure teaching format, skill deconstruction, the Six Steps trainer intervention framework, and performance enhancing feedback. Interactive activities and practice sessions were interspersed with small group discussions. The second day involved consolidation of learning through practice teaching sessions with novice learners, incorporating all the concepts from the first day using ex vivo porcine liver and bowel explants.
Evaluation
Participants completed an 8-item survey using a 5-point Likert scale at the end of the course. In addition, they answered several open-ended questions included with the survey. Analysis of the survey included calculation of frequency counts for each item. Qualitative theme analysis of the open-ended questions allowed for frequency counts of theme responses.
Assessment of the teaching during the second-day practice sessions included observer-based evaluation using the course—Structured Training Trainer Assessment Report (cSTTAR) [13]. The face-to-face Lapco TT courses use this validated instrument to evaluate course effectiveness. The cSTTAR evaluates a course participant’s instruction according to three components of teaching: (1) the set or pre-brief, (2) the dialogue or actual teaching, and (3) the closure or debrief. It uses a Likert-type scale to do so. Mean scores for the set, dialogue, and closure subscales are calculated for each course participant.
Results
Faculty conducted six virtual courses between October 2020 and September 2021. Six participants partook in each course, totaling 36 total learners during the period. In addition, these courses sought to increase the faculty roster for eligible Lapco TT faculty facile in running these courses. This requires 1–2 observation sessions of the course, after which faculty can co-lead the Lapco course. To this end, eight faculty ‘observers’ watched a session as part of faculty development for the course, two of whom later participated as new Lapco TT faculty. One of these observers became a full faculty member during the interval. Figures 2 and 3 represent a typical virtual learning environment appearance during group exercises as well as small group breakout periods.
Of the 36 participants, 31 completed post-course surveys, a response rate of 86%. Figure 4 summarizes the frequency count for the survey questions. In brief, 94% of respondents found that the course allowed guidance and reflection and felt likely to adopt components of the course in their practice. Ninety percent felt it provided a useful structure to use during teaching cases in future. In addition, 90% strongly felt that the virtual format of the course was effective and engaging throughout, and 100% found it well organized. Most importantly, 90% agreed that they would recommend this course to colleagues.
Table 1 summarizes common themes found in the responses given by the delegates completing the survey to the open-ended questions. In general, participant comments emphasized the high-quality, interactive nature of this course (90% of commenters) with little need for improvements. In addition, the key themes indicated that 55% of attendees felt the course was no different than a comparable in-person course. An additional 28% felt the virtual format was a good substitute, and 28% missed the in-person interaction provided by the in-person format.
This format, however, did lack interactive aspects unique to live teaching. One common negative feedback was the complicated nature of the simulator used in the course, and many delegates questioned whether it was necessary at all. 80% of participants felt the trainer worked as intended. 20% felt it was too complicated. When asked what they would change about the simulator, 38% felt no change was needed and 52% felt the trainer was either too complicated or not needed. This feedback was considered seriously by the Virtual TT Task Force, but ultimately the importance of laparoscopic skills in the teaching methodology of this course was paramount and we continued to use the EndoSim simulator. Although many participants have some type of simulator in their home institution, we wanted access to course resources to be fully equitable and consistent. The Virtual TT Task Force worked with EndoSim to streamline and simplify the trainer boxes as much as possible to decrease the footprint of shipped materials needed for the course.
Suggested course structure changes included increasing the frequency of breaks (17%) and adding more practice sessions with novice learners (17%). Finally, 22% wished more people could take the course and half of delegates expressed a desire for continued follow-up with faculty after the course. Because of the last request, three follow-up webinar sessions were offered to participants 1–6 months after course completion as a refresher on Set-Dialogue-Closure and Six-Step frameworks. Participants are invited to attend these sessions indefinitely as desired.
Discussion
While we were forced to pivot from an in-person to a virtual environment for our Lapco Train the Trainer course, we quickly identified benefits. Over 90% of our course participants favorably rated our virtual course. We feel as though this positive response was in part due to our ability to maintain the high faculty-to-learner ratio necessary for its intense interactivity and learner engagement. Additionally, we were able to keep the overall structure and content of the course, making it very similar to its live face-to-face counterpart. In fact, some participants identified aspects of the virtual format that are potentially superior to a face-to-face course for similar instructor training. Although participants did not attend both in-person and virtual Lapco TT courses, some of them have had the opportunity to attend similar educational courses in the past and were thus able to compare and contrast experiences in person and virtual. One stated advantage was the avoidance of travel, allowing faculty and attendees more opportunity to fit the course into their schedules. Additionally, the virtual course did not require coordination with other events, such as the Annual Meeting, to help minimize time away from clinical care. Thus, the virtual format was a cost savings for faculty and learners without travel expenses and with less time away from practice. The cost of shipping simulators was higher than materials costs for in-person courses, but rental of lab space was not needed. The overhead costs including meals and travel for faculty were lower compared to the face-to-face courses.
Although very successful, the virtual format did present some difficulties. These are detailed in Table 2. Some themes were common and were addressed with each iteration of the virtual course. For example, participant feedback and dialogue with EndoSim allowed us to move to a smaller, simplified simulator over time. As difficulties arose, modifications to the virtual platform were necessary and carried over to subsequent courses. Some difficulties like outside distractions are unique to the virtual format. Future studies will aim to evaluate how those difficulties evolve as virtual meetings and work become more prevalent in our day-to-day workflow.
Small group discussion sessions, followed by hands-on practice, are a common structure for technical courses. In the Lapco TT virtual course, virtual one-on-one skills teaching replaced in-person, hands-on instruction. This virtual teaching was limited by video buffering speeds, lack of body language interpretation, and was subject to each site’s facility with troubleshooting audiovisual failures in real time. Dedicated time built into the course schedule for audiovisual troubleshooting was key to successful hands-on sessions. Adjusting cameras for the hands-on portion (i.e., providing a view of both the learner’s position in relation to the trainer box as well as the view from within the trainer box) did help overcome some of these issues.
The Lapco TT method, with its focus on the use of words for guidance rather than demonstrating or manually assisting learners, suits itself to use in a virtual format. SAGES uses it to standardize instructor training for hand-on courses. More recently, it has proved an invaluable tool for improving the well-being of our membership. You cannot attend a medical conference without encountering a session on combating burnout. Burnout usually arises from work related stressors including workload, clerical burden, and inefficient work processes. Overall, academic settings correlate with a lower rate of burnout as compared to private practice [14]. Other independent factors positively associated with career satisfaction include hours spent in the operating room and hours spent in nonpatient care activities [14]. One of the primary drivers in teacher burnout is feelings of diminished personal accomplishment and a perception of being ineffective teachers [15]. Surgeons are often pressed into service as teachers without any background in theory and practice of adult education. Thus, it is reasonable to hope that providing a structure for teaching, deconstructing skills, and intervening with verbal communication can uniformly improve the well-being of the instructors we have trained. It likely has a downstream impact on the people and local institutions where SAGES members practice. Follow-up studies will focus on the impact of the Lapco TT instruction beyond its original intended use as a structure for SAGES clinical courses and to try to elucidate its effect on clinical teaching effectiveness overall. Additionally, we will be offering both virtual and in-person courses so there will be a follow-up study to compare outcomes of these two formats.
Limitations
This study is limited by its small number of participants and the fact that participants had no personal experience with the in-person format used prior. It was also limited by the Likert nature of the survey and the limit of the feedback received from the participants. For example, the feedback from the novice learners in teaching efficacy was not formally captured as part of the course. Costs to ship the simulator were substantial and led to little effective cost difference to SAGES between the in-person and virtual courses. The coordination of multiple sites, multiple time zones, and advanced faculty preparation were unique to this course and presented a challenge.
Conclusion
The COVID-19 pandemic, by halting in-person Lapco TT courses, forced SAGES to pivot to a virtual format to continue this form of faculty development. This pivot maintained the structure and content of the course, and many participants found it a superior format to its in-person variant. It is a feasible option with potential cost benefits to faculty, participants, and organizational sponsors. Expansion of the course offerings even during the course of this study demonstrate that at-home virtual courses can successfully train a cadre of faculty in a standardized, effective way.
References
Coleman MG, Hanna GB, Kennedy R (2011) The National Training Programme for laparoscopic colorectal surgery in England: a new training paradigm. Colorectal Dis 13(6):614–616
Mackenzie H et al (2015) Design, delivery, and validation of a trainer curriculum for the national laparoscopic colorectal training program in England. Ann Surg 261(1):149–156
Dort J et al (2017) Hands-on 2.0: improving transfer of training via the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Acquisition of Data for Outcomes and Procedure Transfer (ADOPT) program. Surg Endosc 31(8):3326–3332
Dort J et al (2019) Something for everyone: the benefits of longitudinal mentorship with the application of the acquisition of data for outcomes and procedure transfer (ADOPT) program to a SAGES hands-on colectomy course. Surg Endosc 33(9):3062–3068
Laloo R et al (2020) Virtual surgical education for core surgical trainees in the Yorkshire deanery during the COVID-19 pandemic. Scott Med J 65(4):138–143
Gonzalez-Urquijo M et al (2021) Transferring face-to-face sessions to virtual sessions in surgical education: a survey-based assessment of a single academic general surgery program. Eur Surg 53(2):55–59
Co M, Chu KM (2020) Distant surgical teaching during COVID-19—a pilot study on final year medical students. Surg Pract 24(3):105–109
Chandrasinghe PC et al (2020) A novel structure for online surgical undergraduate teaching during the COVID-19 pandemic. BMC Med Educ 20(1):324
Co M, Chung PH, Chu KM (2021) Online teaching of basic surgical skills to medical students during the COVID-19 pandemic: a case-control study. Surg Today 51(8):1404–1409
Mishra K, Boland MV, Woreta FA (2020) Incorporating a virtual curriculum into ophthalmology education in the coronavirus disease-2019 era. Curr Opin Ophthalmol 31(5):380–385
Greenberg JA et al (2021) At-home hands-on surgical training during COVID19: proof of concept using a virtual telementoring platform. Surg Endosc 35(5):1963–1969
Bogen EM, Schlachta CM, Ponsky T (2019) White paper: technology for surgical telementoring-SAGES Project 6 Technology Working Group. Surg Endosc 33(3):684–690
Wyles SM et al (2016) Development and implementation of the Structured Training Trainer Assessment Report (STTAR) in the English National Training Programme for laparoscopic colorectal surgery. Surg Endosc 30(3):993–1003
Balch CM et al (2011) Distress and career satisfaction among 14 surgical specialties, comparing academic and private practice settings. Ann Surg 254(4):558–568
Byrne BM (1994) Burnout: testing for the validity, replication, and invariance of causal structure across elementary, intermediate, and secondary teachers. Am Educ Res J 31(3):645–673
Funding
The September 2020, November 2020, February 2021, and May 2021 virtual TT courses were supported by a grant from the SAGES Foundation and medical education grants from Applied Medical and Ethicon USA/Johnson & Johnson Medical Devices Co. The July 2021 and September 2021 virtual courses were supported by a grant from the SAGES Foundation and by SAGES.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Choi has a proctor role for Johnson and Johnson for the LINX device. Dr. Paige has received grants from LSU LIFT, IAMSE, and Avita medical for research grants as a co-investigator. Ms. Schwarz has a staff support role at Society of American Gastrointestinal and Endoscopic Surgeons. Drs. Shada, Sanchez, Dort, Moudgill, and Bernier have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shada, A.L., Sanchez, J., Choi, Y. et al. Better than the real thing? Success of a virtual platform for an established “Train the Trainer” course. Surg Endosc 37, 2673–2681 (2023). https://doi.org/10.1007/s00464-022-09750-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09750-5