Abstract
Background
Pain is a contributing factor to the low compliance rate for performing a colonoscopy on screening for colorectal cancer.
Purpose
This meta-analysis aimed to evaluate the effect of visual distraction on adults undergoing colonoscopy.
Methods
We searched PubMed, EMBASE, Web of Science, and Cochrane Library Database from their inception to February 2022. Randomized controlled trials comparing visual distraction with non-visual distraction were considered for inclusion. The fixed-effects and random-effects models were used to pool the data from individual studies and the Cochrane risk of bias assessment tool was used to determine the methodology quality.
Results
This meta-analysis included four studies (N = 301) for pain level and total procedure time, three studies (N = 181) for satisfaction score, three studies (N = 196) for anxiety level, and four studie (N = 402) for willingness to repeat the procedure. The pooled analysis shown that significantly lower pain levels (SMD, − 0.25; 95% CI − 0.47 to − 0.02; P = 0.03), higher satisfaction score with the procedure (SMD, 0.63; 95% CI, 0.33 to 0.93; P < 0.0001), and higher willingness to repeat the procedure (OR, 2.66; 95% CI 1.70 to 4.17; P < 0.0001) in the visual distraction group than those in the non-visual distraction group, with no significant differences in total procedure time (SMD,− 0.07; 95% CI − 0.30 to 0.15; P = 0.53) or anxiety level (SMD,− 0.27; 95% CI − 0.55 to 0.01; P = 0.06).
Conclusions
Visual distraction improved the patient’s pain, satisfaction, and willingness to repeat the procedure. Thus, visual stimulation is an effective way to reduce pain during colonoscopy and should be recommended.








Similar content being viewed by others
References
Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, Cercek A, Smith RA, Jemal A (2020) Colorectal cancer statistics, 2020. CA Cancer J Clin 70(3):145–164. https://doi.org/10.3322/caac.21601
Shaukat A, Kahi CJ, Burke CA, Rabeneck L, Sauer BG, Rex DK (2021) ACG clinical guidelines: colorectal cancer screening 2021. Am J Gastroenterol 116(3):458–479. https://doi.org/10.14309/ajg.0000000000001122
Montminy EM, Jang A, Conner M, Karlitz JJ (2020) Screening for colorectal cancer. Med Clin North Am 104(6):1023–1036. https://doi.org/10.1016/j.mcna.2020.08.004
Bynum SA, Davis JL, Green BL, Katz RV (2012) Unwillingness to participate in colorectal cancer screening: examining fears, attitudes, and medical mistrust in an ethnically diverse sample of adults 50 years and older. Am J Health Promot 26(5):295–300. https://doi.org/10.4278/ajhp.110113-QUAN-20
Ghevariya V, Duddempudi S, Ghevariya N, Reddy M, Anand S (2013) Barriers to screening colonoscopy in an urban population: a study to help focus further efforts to attain full compliance. Int J Colorectal Dis 28(11):1497–1503. https://doi.org/10.1007/s00384-013-1708-7
Trevisani L, Zelante A, Sartori S (2014) Colonoscopy, pain and fears: Is it an indissoluble trinomial? World J Gastrointest Endosc 6(6):227–233. https://doi.org/10.4253/wjge.v6.i6.227
Childers RE, Williams JL, Sonnenberg A (2015) Practice patterns of sedation for colonoscopy. Gastrointest Endosc 82(3):503–511. https://doi.org/10.1016/j.gie.2015.01.041
Trummel JM, Chandrasekhara V, Kochman ML (2017) Anesthesia for colonoscopy and lower endoscopic procedures. Anesthesiol Clin 35(4):679–686. https://doi.org/10.1016/j.anclin.2017.08.007
Lin OS (2017) Sedation for routine gastrointestinal endoscopic procedures: a review on efficacy, safety, efficiency, cost and satisfaction. Intest Res 15(4):456–466. https://doi.org/10.5217/ir.2017.15.4.456
Wernli KJ, Brenner AT, Rutter CM, Inadomi JM (2016) Risks associated with anesthesia services during colonoscopy. Gastroenterology 150(4):888–894. https://doi.org/10.1053/j.gastro.2015.12.018
Bani Mohammad E, Ahmad M (2019) Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: a randomized control trial. Palliat Support Care 17(1):29–34. https://doi.org/10.1017/S1478951518000639
Koticha P, Katge F, Shetty S, Patil DP (2019) Effectiveness of virtual reality eyeglasses as a distraction aid to reduce anxiety among 6–10-year-old children undergoing dental extraction procedure. Int J Clin Pediatr Dent 12(4):297–302. https://doi.org/10.5005/jp-journals-10005-1640
Matheve T, Bogaerts K, Timmermans A (2020) Virtual reality distraction induces hypoalgesia in patients with chronic low back pain: a randomized controlled trial. J Neuroeng Rehabil 17(1):55. https://doi.org/10.1186/s12984-020-00688-0
Sajeev MF, Kelada L, Yahya Nur AB, Wakefield CE, Wewege MA, Karpelowsky J, Akimana B, Darlington AS, Signorelli C (2021) Interactive video games to reduce paediatric procedural pain and anxiety: a systematic review and meta-analysis. Br J Anaesth 127(4):608–619. https://doi.org/10.1016/j.bja.2021.06.039
Celebi D, Yilmaz E, Sahin ST, Baydur H (2020) The effect of music therapy during colonoscopy on pain, anxiety and patient comfort: a randomized controlled trial. Complement Ther Clin Pract 38:101084. https://doi.org/10.1016/j.ctcp.2019.101084
De Silva AP, Niriella MA, Nandamuni Y, Nanayakkara SD, Perera KRP, Kodisinghe SK, Subasinghe KCE, Pathmeswaran A, de Silva HJ. (2016). Effect of audio and visual distraction on patients undergoing colonoscopy: a randomized controlled study. Endoscopy international open, 4(11) E1211-E1214. <Go to ISI>://MEDLINE:27853748
Bechtold ML, Puli SR, Othman MO, Bartalos CR, Marshall JB, Roy PK (2009) Effect of music on patients undergoing colonoscopy: a meta-analysis of randomized controlled trials. Dig Dis Sci 54(1):19–24. https://doi.org/10.1007/s10620-008-0312-0
Sorkpor SK, Johnson CM, Santa Maria DM, Miao H, Moore C, Ahn H (2021) The effect of music listening on pain in adults undergoing colonoscopy: a systematic review and meta-analysis. J Perianesth Nurs 36(5):573-580 e571. https://doi.org/10.1016/j.jopan.2020.12.012
Tam WW, Wong EL, Twinn SF (2008) Effect of music on procedure time and sedation during colonoscopy: a meta-analysis. World J Gastroenterol 14(34):5336–5343. https://doi.org/10.3748/wjg.14.5336
Indovina P, Barone D, Gallo L, Chirico A, De Pietro G, Giordano A (2018) Virtual reality as a distraction intervention to relieve pain and distress during medical procedures: a comprehensive literature review. Clin J Pain 34(9):858–877. https://doi.org/10.1097/ajp.0000000000000599
Jiang XL, Li XL, Lan ZH (2015) Effects of visual and audiovisual distraction on pain and anxiety among patients undergoing colonoscopy. Gastroenterol Nurs 38(1):55–61. https://doi.org/10.1097/sga.0000000000000089
Lee DW, Chan AC, Wong SK, Fung TM, Li AC, Chan SK, Mui LM, Ng EK, Chung SC (2004) Can visual distraction decrease the dose of patient-controlled sedation required during colonoscopy? a prospective randomized controlled trial. Endoscopy 36(3):197–201. https://doi.org/10.1055/s-2004-814247
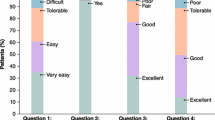
Sheng LP, Han CQ, Nie C, Xu T, Zhang K, Li XJ, Xie XR, Lin R, Ding Z (2021) Watching videos of colonoscopies and receiving interpretations reduce pain and anxiety while increasing the satisfaction of patients. Dig Dis Sci 66(2):541–546. https://doi.org/10.1007/s10620-020-06186-6
Umezawa S, Higurashi T, Uchiyama S, Sakai E, Ohkubo H, Endo H, Nonaka T, Nakajima A (2015) Visual distraction alone for the improvement of colonoscopy-related pain and satisfaction. World J Gastroenterol 21(15):4707–4714. https://doi.org/10.3748/wjg.v21.i15.4707
Veldhuijzen G, Klaassen NJM, Van Wezel RJA, Drenth JPH, Van Esch AA (2020) Virtual reality distraction for patients to relieve pain and discomfort during colonoscopy. Endosc Int Open 8(7):E959–E966. https://doi.org/10.1055/a-1178-9289
Higgins JPT, TJ, Chandler J, Cumpston MLiT, Page MJ, et al. (2022). Cochrane handbook for systematic reviews of interventions version 6.3 (updated Feb 2022). www.training.cochrane.org/handbook.
Barry MJ, Davidson K, Mangione CM (2021) US preventive services task force recommendation statement on screening for colorectal cancer-reply. JAMA 326(13):1328–1329. https://doi.org/10.1001/jama.2021.13469
Davis JL, Bynum SA, Katz RV, Buchanan K, Green BL (2012) Sociodemographic differences in fears and mistrust contributing to unwillingness to participate in cancer screenings. J Health Care Poor Underserved 23(4):67–76. https://doi.org/10.1353/hpu.2012.0148
McLachlan SA, Clements A, Austoker J (2012) Patients’ experiences and reported barriers to colonoscopy in the screening context–a systematic review of the literature. Patient Educ Couns 86(2):137–146. https://doi.org/10.1016/j.pec.2011.04.010
Ladas SD, Satake Y, Mostafa I, Morse J (2010) Sedation practices for gastrointestinal endoscopy in Europe, North America, Asia Africa and Australia. Digestion 82(2):74–76. https://doi.org/10.1159/000285248
Zhou S, Zhu Z, Dai W, Qi S, Tian W, Zhang Y, Zhang X, Huang L, Tian J, Yu W, Su D (2021) National survey on sedation for gastrointestinal endoscopy in 2758 Chinese hospitals. Br J Anaesth 127(1):56–64. https://doi.org/10.1016/j.bja.2021.01.028
Sato M, Horiuchi A, Tamaki M, Ichise Y, Kajiyama M, Yamamoto Y, Tanaka N (2019) Safety and effectiveness of nurse-administered propofol sedation in outpatients undergoing gastrointestinal endoscopy. Clin Gastroenterol Hepatol 17(6):1098-1104.e1091. https://doi.org/10.1016/j.cgh.2018.06.025
Zacharias P, Mathew S, Mathews J, Somu A, Peethambaran M, Prashanth M, Philip M (2018) Sedation practices in gastrointestinal endoscopy-a survey from southern India. Indian J Gastroenterol 37(2):164–168. https://doi.org/10.1007/s12664-018-0843-z
Ampuero J, Romero-Gomez M (2012) Re: unsedated colonoscopy: an option for some but not for all. Gastrointest Endosc. https://doi.org/10.1016/j.gie.2012.03.003
Cakir SK, Evirgen S (2021) The effect of virtual reality on pain and anxiety during colonoscopy: a randomized controlled trial. Turkish Journal of Gastroenterology 32(5):451–457. https://doi.org/10.5152/tjg.2021.191081
Basak T, Duman S, Demirtas A (2020) Distraction-based relief of pain associated with peripheral intravenous catheterisation in adults: a randomised controlled trial. J Clin Nurs 29(5–6):770–777. https://doi.org/10.1111/jocn.15131
Grabinski ZG, Boscamp NS, Zuckerman WA, Zviti R, O’Brien A, Martinez M, Tsze DS (2022) Efficacy of distraction for reducing pain and distress associated with venipuncture in the pediatric posttransplant population: a randomized controlled trial. Pediatr Emerg Care 38(2):e811–e815. https://doi.org/10.1097/PEC.0000000000002458
Molleman J, Tielemans JF, Braam MJI, Weitenberg B, Koch R (2019) Distraction as a simple and effective method to reduce pain during local anesthesia: a randomized controlled trial. J Plast Reconstr Aesthet Surg 72(12):1979–1985. https://doi.org/10.1016/j.bjps.2019.07.023
Malloy KM, Milling LS (2010) The effectiveness of virtual reality distraction for pain reduction: a systematic review. Clin Psychol Rev 30(8):1011–1018. https://doi.org/10.1016/j.cpr.2010.07.001
Houze B, Streff A, Piche M, Rainville P (2021) Spinal and supraspinal modulation of pain responses by hypnosis, suggestions, and distraction. Am J Clin Hypn 63(4):329–354. https://doi.org/10.1080/00029157.2020.1863184
Canbulat Sahiner N, Turkmen AS (2019) The effect of distraction cards on reducing pain and anxiety during intramuscular injection in children. Worldviews Evid Based Nurs 16(3):230–235. https://doi.org/10.1111/wvn.12359
Johnson MH (2005) How does distraction work in the management of pain? Curr Pain Headache Rep 9(2):90–95. https://doi.org/10.1007/s11916-005-0044-1
Wittkopf PG, Lloyd DM, Coe O, Yacoobali S, Billington J (2020) The effect of interactive virtual reality on pain perception: a systematic review of clinical studies. Disabil Rehabil 42(26):3722–3733. https://doi.org/10.1080/09638288.2019.1610803
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Yuan-Yuan Zhang, Ramoo Vimala, Ping Lei Chui, Ida Normiha Hilmi have no conflicts of interest or financial ties to disclose.
Ethical approval
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, YY., Vimala, R., Chui, P.L. et al. Effect of visual distraction on pain in adults undergoing colonoscopy: a meta-analysis. Surg Endosc 37, 2633–2643 (2023). https://doi.org/10.1007/s00464-022-09724-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09724-7