Abstract
Background
Several pivotal studies and international guidelines on the perioperative management of rectal cancer have been published. However, little is known about the current state of perioperative management of rectal cancer patients in clinical practice worldwide.
Methods
An online survey including 13 questions focusing on key topics related to the perioperative management of patients with rectal cancer was conducted among colorectal surgeons registered within the database of the Research Institute Against Digestive Cancer (IRCAD).
Results
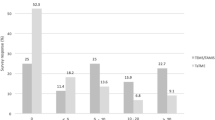
A total of 535 respondents from 89 countries participated in the survey. Most surgeons worked in the European region (40.9%). Two hundred and fifty-four respondents (47.5%) performed less than 25% of surgical procedures laparoscopically. The most commonly used definition of the upper limit of the rectum was a fixed distance from the anal verge (23.4%). Magnetic resonance imaging was used to define the upper limit of the rectum by 258 respondents (48.2%). During total mesorectal excision (TME), 301 respondents (56.3%) used a high-tie technique. The most commonly constructed anastomosis was an end-to-end anastomosis (68.2%) with the majority of surgeons performing a leak test intraoperatively (88.9%). A total of 355 respondents (66.4%) constructed a diverting ostomy, and the majority of these surgeons constructed an enterostomy (82%). A total of 208 respondents (39.3%) closed a stoma within 8 weeks. Lastly, 135 respondents (25.2%) introduced a solid diet on postoperative day 1.
Conclusion
There is considerable heterogeneity in the perioperative management of rectal cancer patients worldwide with several discrepancies between current international practice and recommendations from international guidelines. To achieve worldwide standardization in rectal cancer care, further research is needed to elucidate the cause of this heterogeneity and find ways of improved implementation of best practice recommendations.

Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Heald RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgery–the clue to pelvic recurrence? Br J Surg 69(10):613–616
Baek JH, McKenzie S, Garcia-Aguilar J, Pigazzi A (2010) Oncologic outcomes of robotic-assisted total mesorectal excision for the treatment of rectal cancer. Ann Surg 251(5):882–886
Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T et al (2001) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 345(9):638–646
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage ii or iii rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314(13):1346–1355
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ et al (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314(13):1356–1363
Al-Taher M, Okamoto N, Mutter D, Stassen LPS, Marescaux J, Diana M et al (2022) International survey among surgeons on laparoscopic right hemicolectomy: the gap between guidelines and reality. Surg Endosc. https://doi.org/10.1007/s00464-022-09044-w
Edwards PJ, Roberts I, Clarke MJ, Diguiseppi C, Wentz R, Kwan I et al (2009) Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev 2009(3):Mr000008
D’souza N, de Nereetotbabberich MPM, Dehoore A, Tiret E, Xynos E, Beetstan RGH et al (2019) Definition of the rectum: an international Expert-based delphi consensus. Ann Surg 270(6):955–959
WHO. Definition of Regional Groupings [Available from: https://www.who.int/healthinfo/global_burden_disease/definition_regions/en/#:~:text=WHO%20regions%3A%20WHO%20Member%20States,Region%2C%20and%20Western%20Pacific%20Region.
You YN, Hardiman KM, Bafford A, Poylin V, Francone TD, Davis K et al (2020) The American society of colon and rectal surgeons clinical practice guidelines for the management of rectal cancer. Dis Colon Rectum 63(9):1191–1222
Benson AB, Venook AP, AlHawary MM, Arain MA, Chen YJ, Ciombor KK et al (2020) NCCN guidelines insights: rectal cancer version 6 2020. J Natl Compr Canc Netw 18(7):806–815
Glynne-Jones R, Wyrwicz L, Tiret E, Brown G, Rödel C, Cervantes A et al (2017) Rectal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 28((suppl 4)):iv22–iv40
Li F, Wang B, Lu S, Wang Y, Sun T, Wang H et al (2020) Comparison of the sigmoid take-off with other definitions of the rectosigmoid junction: a retrospective comparative cohort analysis. Int J Surg 80:168–174
Bogveradze N, Lambregts DMJ, el Khababi N, Dresen RC, Maas M, Kusters M et al (2021) The sigmoid take-off as a landmark to distinguish rectal from sigmoid tumours on MRI: Reproducibility, pitfalls and potential impact on treatment stratification. European J Surg Oncol. https://doi.org/10.1016/j.ejso.2021.09.009
D’Souza N, Lord A, Shaw A, Patel A, Balyasnikova S, Tudyka V et al (2020) The sigmoid take-off: an anatomical imaging definition of the rectum validated on specimen analysis. Eur J Surg Oncol 46(9):1668–1672
Faletti R, Gatti M, Arezzo A, Stola S, Benedini MC, Bergamasco L et al (2018) Preoperative staging of rectal cancer using magnetic resonance imaging: comparison with pathological staging. Minerva Chir 73(1):13–19
Klessen C, Rogalla P, Taupitz M (2007) Local staging of rectal cancer: the current role of MRI. Eur Radiol 17(2):379–389
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372(14):1324–1332
Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM et al (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC trial group. J Clin Oncol 25(21):3061–3068
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB et al (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15(7):767–774
Fleshman J, Branda ME, Sargent DJ, Boller AM, George VV, Abbas MA et al (2019) Disease-free survival and local recurrence for laparoscopic resection compared with open resection of stage II to III rectal cancer: follow-up results of the ACOSOG Z6051 randomized controlled trial. Ann Surg 269(4):589–595
Stevenson ARL, Solomon MJ, Brown CSB, Lumley JW, Hewett P, Clouston AD et al (2019) Disease-free survival and local recurrence after laparoscopic-assisted resection or open resection for rectal cancer: the Australasian laparoscopic cancer of the rectum randomized clinical trial. Ann Surg 269(4):596–602
Charan I, Kapoor A, Singhal MK, Jagawat N, Bhavsar D, Jain V et al (2015) High ligation of inferior mesenteric artery in left colonic and rectal cancers: lymph node yield and survival benefit. Indian J Surg 77(Suppl 3):1103–1108
Kessler H, Hohenberger W (2013) Extended lymphadenectomy in colon cancer is crucial. World J Surg 37(8):1789–1798
Chin CC, Yeh CY, Tang R, Changchien CR, Huang WS, Wang JY (2008) The oncologic benefit of high ligation of the inferior mesenteric artery in the surgical treatment of rectal or sigmoid colon cancer. Int J Colorectal Dis 23(8):783–788
Alici A, Kement M, Gezen C, Akin T, Vural S, Okkabaz N et al (2010) Apical lymph nodes at the root of the inferior mesenteric artery in distal colorectal cancer: an analysis of the risk of tumor involvement and the impact of high ligation on anastomotic integrity. Tech Coloproctol 14(1):1–8
Zeng J, Su G (2018) High ligation of the inferior mesenteric artery during sigmoid colon and rectal cancer surgery increases the risk of anastomotic leakage: a meta-analysis. World J Surg Oncol 16(1):157
Komen N, Slieker J, de Kort P, de Wilt JH, van der Harst E, Coene PP et al (2011) High tie versus low tie in rectal surgery: comparison of anastomotic perfusion. Int J Colorectal Dis 26(8):1075–1078
Fan D, Zhang C, Li X, Yao C, Yao T (2018) Evaluation of the clinical efficacy of preserving the left colic artery in laparoscopic resection for rectal cancer: a meta-analysis. Mol Clin Oncol 9(5):553–560
Hajibandeh S, Hajibandeh S, Maw A (2020) Meta-analysis and trial sequential analysis of randomized controlled trials comparing high and low ligation of the inferior mesenteric artery in rectal cancer surgery. Dis Colon Rectum 63(7):988–999
Zhang C, Chen L, Cui M, Xing J, Yang H, Yao Z et al (2020) Short- and long-term outcomes of rectal cancer patients with high or improved low ligation of the inferior mesenteric artery. Sci Rep 10(1):15339
Yang Y, Wang G, He J, Zhang J, Xi J, Wang F (2018) High tie versus low tie of the inferior mesenteric artery in colorectal cancer: a meta-analysis. Int J Surg 52:20–24
Mari GM, Crippa J, Cocozza E, Berselli M, Livraghi L, Carzaniga P et al (2019) Low ligation of inferior mesenteric artery in laparoscopic anterior resection for rectal cancer reduces genitourinary dysfunction: results from a randomized controlled trial (HIGHLOW trial). Ann Surg 269(6):1018–1024
Brown CJ, Fenech DS, McLeod RS (2008) Reconstructive techniques after rectal resection for rectal cancer. Cochrane Database Syst Rev 2:Cd006040
Liao C, Gao F, Cao Y, Tan A, Li X, Wu D (2010) Meta-analysis of the colon J-pouch vs transverse coloplasty pouch after anterior resection for rectal cancer. Colorectal Dis 12(7):624–631
Hüttner FJ, Tenckhoff S, Jensen K, Uhlmann L, Kulu Y, Büchler MW et al (2015) Meta-analysis of reconstruction techniques after low anterior resection for rectal cancer. Br J Surg 102(7):735–745
Okkabaz N, Haksal M, Atici AE, Altuntas YE, Gundogan E, Gezen FC, Oncel M (2017) J-pouch vs side-to-end anastomosis after hand-assisted laparoscopic low anterior resection for rectal cancer: a prospective randomized trial on short and long term outcomes including life quality and functional results. Int J Surg 47:4–12
Fazio VW, Zutshi M, Remzi FH, Parc Y, Ruppert R, Fürst A et al (2007) A randomized multicenter trial to compare long-term functional outcome, quality of life, and complications of surgical procedures for low rectal cancers. Ann Surg 246(3):481–488
Wu Z, van de Haar RC, Sparreboom CL, Boersema GS, Li Z, Ji J et al (2016) Is the intraoperative air leak test effective in the prevention of colorectal anastomotic leakage? a systematic review and meta-analysis. Int J Colorectal Dis 31(8):1409–1417
Daams F, Wu Z, Lahaye MJ, Jeekel J, Lange JF (2014) Prediction and diagnosis of colorectal anastomotic leakage: a systematic review of literature. World J Gastrointest Surg 6(2):14–26
Wu SW, Ma CC, Yang Y (2014) Role of protective stoma in low anterior resection for rectal cancer: a meta-analysis. World J Gastroenterol 20(47):18031–18037
Tan WS, Tang CL, Shi L, Eu KW (2009) Meta-analysis of defunctioning stomas in low anterior resection for rectal cancer. Br J Surg 96(5):462–472
Montedori A, Cirocchi R, Farinella E, Sciannameo F, Abraha I (2010) Covering ileo- or colostomy in anterior resection for rectal carcinoma. Cochrane Database Syst Rev 5:cd006878
Hüser N, Michalski CW, Erkan M, Schuster T, Rosenberg R, Kleeff J et al (2008) Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg 248(1):52–60
Pisarska M, Gajewska N, Małczak P, Wysocki M, Witowski J, Torbicz G et al (2018) Defunctioning ileostomy reduces leakage rate in rectal cancer surgery—systematic review and meta-analysis. Oncotarget 9(29):20816–20825
Gu WL, Wu SW (2015) Meta-analysis of defunctioning stoma in low anterior resection with total mesorectal excision for rectal cancer: evidence based on thirteen studies. World J Surg Oncol 13:9
Cheng Z, Dong S, Bi D, Wang Y, Dai Y, Zhang X (2021) Early versus late preventive ileostomy closure following colorectal surgery: systematic review and meta-analysis with trial sequential analysis of randomized controlled trials. Dis Colon Rectum 64(1):128–137
Han-Geurts IJ, Hop WC, Kok NF, Lim A, Brouwer KJ, Jeekel J (2007) Randomized clinical trial of the impact of early enteral feeding on postoperative ileus and recovery. Br J Surg 94(5):555–561
Lloyd GM, Kirby R, Hemingway DM, Keane FB, Miller AS, Neary P (2010) The RAPID protocol enhances patient recovery after both laparoscopic and open colorectal resections. Surg Endosc 24(6):1434–1439
Wallström A, Frisman GH (2014) Facilitating early recovery of bowel motility after colorectal surgery: a systematic review. J Clin Nurs 23(1–2):24–44
Boelens PG, Heesakkers FF, Luyer MD, van Barneveld KW, de Hingh IH, Nieuwenhuijzen GA et al (2014) Reduction of postoperative ileus by early enteral nutrition in patients undergoing major rectal surgery: prospective, randomized, controlled trial. Ann Surg 259(4):649–655
Zhuang CL, Ye XZ, Zhang CJ, Dong QT, Chen BC, Yu Z (2013) Early versus traditional postoperative oral feeding in patients undergoing elective colorectal surgery: a meta-analysis of randomized clinical trials. Dig Surg 30(3):225–232
Andersen HK, Lewis SJ, Thomas S (2006) Early enteral nutrition within 24h of colorectal surgery versus later commencement of feeding for postoperative complications. Cochrane Database Syst Rev 4:cd004080
Osland E, Yunus RM, Khan S, Memon MA (2011) Early versus traditional postoperative feeding in patients undergoing resectional gastrointestinal surgery: a meta-analysis. JPEN J Parenter Enteral Nutr 35(4):473–487
Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N et al (2019) Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS®) society recommendations: 2018. World J Surg 43(3):659–695
Acknowledgements
We would like to thank Thomas Parent and Margaux Diebold for the data collection through the IRCAD and WebSurg databases, as well as Guy Temporal and Christopher Burel for their proofreading assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Jacques Marescaux is the President of IRCAD, which is partly funded by KARL STORZ and Medtronic. Zaid Al-Difaie, Nariaki Okamoto, Mahdi Al-Taher, Max Scheepers, Nicole Bouvy, Laurents Stassen, Didier Mutter, Michele Diana, and Bernard Dallemagne have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Al-Difaie, Z., Okamoto, N., Scheepers, M.H.M.C. et al. International survey among surgeons on the perioperative management of rectal cancer. Surg Endosc 37, 1901–1915 (2023). https://doi.org/10.1007/s00464-022-09702-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09702-z