Abstract
Introduction
The LapSim (Surgical Science, Sweden) laparoscopic simulator is a high-fidelity virtual reality simulator for use in endoscopic surgical training. This review critiques the current validity evidence for the LapSim laparoscopic simulator, specifically with respect to its potential use as a tool and method of training and assessment in surgery.
Methods
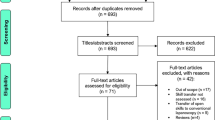
A scoping review of the MEDLINE (PubMed), EMBASE, Cochrane and Web of Science databases was conducted in accordance with PRISMA guidelines (2020)—scoping review extension. Articles were included if they presented validity evidence for the use of the LapSim in operative skill training or assessment, in accordance with Messick’s validity framework. European Association of Endoscopic Surgeons (EAES) guidelines (2005) were used to provide recommendations for the use of the LapSim in operative performance training and assessments.
Results
Forty-nine articles were included. An EAES level 2 recommendation was provided with regard to the internal consistency reliability of automated performance metrics in assessing performance. An EAES recommendation of 2 was awarded with respect to the ability of the LapSim to discriminate based on case volume and overall laparoscopic experience (relationships with other variables). Performance assessment metrics on the LapSim correlate with improved performance in the operating room (EAES level of recommendation 1—consequential validity).
Conclusion
The LapSim has accumulated substantial evidence supporting the validity of its use in surgical training and assessment. Future studies should explore the relationship between the achievement of performance benchmarks on the LapSim and subsequent patient outcomes, and interrogate the benefits of implementing virtual reality simulation training and assessment curricula in post-graduate surgical training programmes.

(Adapted from [63]
Similar content being viewed by others
References
Hong M, Rozenblit JW, Hamilton AJ (2021) Simulation-based surgical training systems in laparoscopic surgery: a current review. Virtual Real 25:491–510
Toale C, Morris M, Kavanagh D (2021) Perceptions and experiences of simulation-based assessment of technical skill in surgery: a scoping review. Am J Surg 222:723–730
McDougall EM (2007) Validation of surgical simulators. J Endourol 21:244–247
Carter FJ, Schijven MP, Aggarwal R, Grantcharov T, Francis NK, Hanna GB, Jakimowicz JJ (2005) Consensus guidelines for validation of virtual reality surgical simulators. Surg Endosc 19:1523–1532
Fairhurst K, Strickland A, Maddern G (2011) The LapSim virtual reality simulator: promising but not yet proven. Surg Endosc 25:343–355
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169:467–473
Smyer P (2011) The medical education research study quality instrument (MERSQI)
Hambleton RK, Arrasmith G, Sheehan DS, Grobe RP, Hathaway W, Doherty V, Forbes D, Houser R, Ingebo G, Kingsbury G (1986) Standards for educational and psychological testing: six reviews. JSTOR
Cook DA, Lineberry M (2016) Consequences validity evidence: evaluating the impact of educational assessments. Acad Med 91:785–795
Cook DA, Hatala R (2016) Validation of educational assessments: a primer for simulation and beyond. Adv Simul 1:31
Doneza JA, Palvia V, Lerner VT, Overbey J, Levie M, Brodman M, Ascher-Walsh C (2021) Correlation of surgical case volume and fellowship training with performance on simulated procedural tasks. Am J Obstet Gynecol 225:548.e541-548.e510
Haidari TA, Bjerrum F, Hansen HJ, Konge L, Petersen RH (2022) Simulation-based VATS resection of the five lung lobes: a technical skills test. Surg Endosc 36:1234–1242
Jensen K, Hansen HJ, Petersen RH, Neckelmann K, Vad H, Møller LB, Pedersen JH, Konge L (2019) Evaluating competency in video-assisted thoracoscopic surgery (VATS) lobectomy performance using a novel assessment tool and virtual reality simulation. Surg Endosc 33:1465–1473
Våpenstad C, Hofstad EF, Bø LE, Kuhry E, Johnsen G, Mårvik R, Langø T, Hernes TN (2017) Lack of transfer of skills after virtual reality simulator training with haptic feedback. Minim Invasive Ther Allied Technol 26:346–354
Mathews S, Brodman M, D’Angelo D, Chudnoff S, McGovern P, Kolev T, Bensinger G, Mudiraj S, Nemes A, Feldman D, Kischak P, Ascher-Walsh C (2017) Predictors of laparoscopic simulation performance among practicing obstetrician gynecologists. Am J Obstet Gynecol 217:596.e591-596.e597
Bjerrum F, Strandbygaard J, Rosthøj S, Grantcharov T, Ottesen B, Sorensen JL (2017) Evaluation of procedural simulation as a training and assessment tool in general surgery-simulating a laparoscopic appendectomy. J Surg Educ 74:243–250
Jensen K, Bjerrum F, Hansen HJ, Petersen RH, Pedersen JH, Konge L (2017) Using virtual reality simulation to assess competence in video-assisted thoracoscopic surgery (VATS) lobectomy. Surg Endosc 31:2520–2528
Jensen K, Bjerrum F, Hansen HJ, Petersen RH, Pedersen JH, Konge L (2015) A new possibility in thoracoscopic virtual reality simulation training: development and testing of a novel virtual reality simulator for video-assisted thoracoscopic surgery lobectomy. Interact Cardiovasc Thorac Surg 21:420–426
Alwaal A, Al-Qaoud TM, Haddad RL, Alzahrani TM, Delisle J, Anidjar M (2015) Transfer of skills on LapSim virtual reality laparoscopic simulator into the operating room in urology. Urol Ann 7:172–176
Lin D, Pena G, Field J, Altree M, Marlow N, Babidge W, Hewett P, Maddern G (2016) What are the demographic predictors in laparoscopic simulator performance? ANZ J Surg 86:983–989
Akdemir A, Sendağ F, Oztekin MK (2014) Laparoscopic virtual reality simulator and box trainer in gynecology. Int J Gynaecol Obstet 125:181–185
Khan MW, Lin D, Marlow N, Altree M, Babidge W, Field J, Hewett P, Maddern G (2014) Laparoscopic skills maintenance: a randomized trial of virtual reality and box trainer simulators. J Surg Educ 71:79–84
Akdemir A, Ergenoğlu AM, Yeniel A, Sendağ F (2013) Conventional box model training improves laparoscopic skills during salpingectomy on LapSim: a randomized trial. J Turk Ger Gynecol Assoc 14:157–162
Xafis V, Babidge W, Field J, Altree M, Marlow N, Maddern G (2013) The efficacy of laparoscopic skills training in a Mobile Simulation Unit compared with a fixed site: a comparative study. Surg Endosc 27:2606–2612
Lehmann KS, Gröne J, Lauscher JC, Ritz JP, Holmer C, Pohlen U, Buhr HJ (2012) Simulation training in surgical education—application of virtual reality laparoscopic simulators in a surgical skills course. Zentralbl Chir 137:130–137
Tan SC, Marlow N, Field J, Altree M, Babidge W, Hewett P, Maddern GJ (2012) A randomized crossover trial examining low- versus high-fidelity simulation in basic laparoscopic skills training. Surg Endosc 26:3207–3214
Shetty S, Panait L, Baranoski J, Dudrick SJ, Bell RL, Roberts KE, Duffy AJ (2012) Construct and face validity of a virtual reality-based camera navigation curriculum. J Surg Res 177:191–195
Kovac E, Azhar RA, Quirouet A, Delisle J, Anidjar M (2012) Construct validity of the LapSim virtual reality laparoscopic simulator within a urology residency program. Can Urol Assoc J 6:253–259
Palter VN, Graafland M, Schijven MP, Grantcharov TP (2012) Designing a proficiency-based, content validated virtual reality curriculum for laparoscopic colorectal surgery: a Delphi approach. Surgery 151:391–397
Våpenstad C, Hofstad E, Bø LE, Chmarra M, Kuhry E, Johnsen G, Mårvik R, Langø T (2012) Limitations of haptic feedback devices on construct validity of the LapSim((R)) virtual reality simulator. Surg Endosc 27
Panait L, Larios JM, Brenes RA, Fancher TT, Ajemian MS, Dudrick SJ, Sanchez JA (2011) Surgical skills assessment of applicants to general surgery residency. J Surg Res 170:189–194
Calatayud D, Arora S, Aggarwal R, Kruglikova I, Schulze S, Funch-Jensen P, Grantcharov T (2010) Warm-up in a virtual reality environment improves performance in the operating room. Ann Surg 251:1181–1185
van Dongen KW, Ahlberg G, Bonavina L, Carter FJ, Grantcharov TP, Hyltander A, Schijven MP, Stefani A, van der Zee DC, Broeders IA (2011) European consensus on a competency-based virtual reality training program for basic endoscopic surgical psychomotor skills. Surg Endosc 25:166–171
Gauger PG, Hauge LS, Andreatta PB, Hamstra SJ, Hillard ML, Arble EP, Kasten SJ, Mullan PB, Cederna PS, Minter RM (2010) Laparoscopic simulation training with proficiency targets improves practice and performance of novice surgeons. Am J Surg 199:72–80
Tanoue K, Uemura M, Kenmotsu H, Ieiri S, Konishi K, Ohuchida K, Onimaru M, Nagao Y, Kumashiro R, Tomikawa M, Hashizume M (2010) Skills assessment using a virtual reality simulator, LapSim, after training to develop fundamental skills for endoscopic surgery. Minim Invasive Ther Allied Technol 19:24–29
Maagaard M, Sorensen JL, Oestergaard J, Dalsgaard T, Grantcharov TP, Ottesen BS, Larsen CR (2011) Retention of laparoscopic procedural skills acquired on a virtual-reality surgical trainer. Surg Endosc 25:722–727
Schreuder HW, van Dongen KW, Roeleveld SJ, Schijven MP, Broeders IA (2009) Face and construct validity of virtual reality simulation of laparoscopic gynecologic surgery. Am J Obstet Gynecol 200:540.e541-548
Larsen CR, Soerensen JL, Grantcharov TP, Dalsgaard T, Schouenborg L, Ottosen C, Schroeder TV, Ottesen BS (2009) Effect of virtual reality training on laparoscopic surgery: randomised controlled trial. BMJ 338:b1802
Sinha P, Hogle NJ, Fowler DL (2008) Do the laparoscopic skills of trainees deteriorate over time? Surg Endosc 22:2018–2025
Hogle NJ, Widmann WD, Ude AO, Hardy MA, Fowler DL (2008) Does training novices to criteria and does rapid acquisition of skills on laparoscopic simulators have predictive validity or are we just playing video games? J Surg Educ 65:431–435
Kundhal PS, Grantcharov TP (2009) Psychomotor performance measured in a virtual environment correlates with technical skills in the operating room. Surg Endosc 23:645–649
Salgado J, Grantcharov TP, Papasavas PK, Gagne DJ, Caushaj PF (2009) Technical skills assessment as part of the selection process for a fellowship in minimally invasive surgery. Surg Endosc 23:641–644
Panait L, Bell RL, Roberts KE, Duffy AJ (2008) Designing and validating a customized virtual reality-based laparoscopic skills curriculum. J Surg Educ 65:413–417
Botden SM, Buzink SN, Schijven MP, Jakimowicz JJ (2007) Augmented versus virtual reality laparoscopic simulation: what is the difference? A comparison of the ProMIS augmented reality laparoscopic simulator versus LapSim virtual reality laparoscopic simulator. World J Surg 31:764–772
van Dongen KW, Tournoij E, van der Zee DC, Schijven MP, Broeders IA (2007) Construct validity of the LapSim: can the LapSim virtual reality simulator distinguish between novices and experts? Surg Endosc 21:1413–1417
Newmark J, Dandolu V, Milner R, Grewal H, Harbison S, Hernandez E (2007) Correlating virtual reality and box trainer tasks in the assessment of laparoscopic surgical skills. Am J Obstet Gynecol 197:546.e541–544
Hogle NJ, Briggs WM, Fowler DL (2007) Documenting a learning curve and test-retest reliability of two tasks on a virtual reality training simulator in laparoscopic surgery. J Surg Educ 64:424–430
Ahlberg G, Enochsson L, Gallagher AG, Hedman L, Hogman C, McClusky DA 3rd, Ramel S, Smith CD, Arvidsson D (2007) Proficiency-based virtual reality training significantly reduces the error rate for residents during their first 10 laparoscopic cholecystectomies. Am J Surg 193:797–804
Hassan I, Gerdes B, Koller M, Langer P, Rothmund M, Zielke A (2006) Clinical background is required for optimum performance with a VR laparoscopy simulator. Comput Aided Surg 11:103–106
Woodrum DT, Andreatta PB, Yellamanchilli RK, Feryus L, Gauger PG, Minter RM (2006) Construct validity of the LapSim laparoscopic surgical simulator. Am J Surg 191:28–32
Larsen CR, Grantcharov T, Aggarwal R, Tully A, Sørensen JL, Dalsgaard T, Ottesen B (2006) Objective assessment of gynecologic laparoscopic skills using the LapSimGyn virtual reality simulator. Surg Endosc 20:1460–1466
Aggarwal R, Grantcharov TP, Eriksen JR, Blirup D, Kristiansen VB, Funch-Jensen P, Darzi A (2006) An evidence-based virtual reality training program for novice laparoscopic surgeons. Ann Surg 244:310–314
Aggarwal R, Tully A, Grantcharov T, Larsen CR, Miskry T, Farthing A, Darzi A (2006) Virtual reality simulation training can improve technical skills during laparoscopic salpingectomy for ectopic pregnancy. BJOG 113:1382–1387
Eriksen JR, Grantcharov T (2005) Objective assessment of laparoscopic skills using a virtual reality stimulator. Surg Endosc 19:1216–1219
Hassan I, Sitter H, Schlosser K, Zielke A, Rothmund M, Gerdes B (2005) A virtual reality simulator for objective assessment of surgeons’ laparoscopic skill. Chirurg 76:151–156
Langelotz C, Kilian M, Paul C, Schwenk W (2005) LapSim virtual reality laparoscopic simulator reflects clinical experience in German surgeons. Langenbecks Arch Surg 390:534–537
Sherman V, Feldman LS, Stanbridge D, Kazmi R, Fried GM (2005) Assessing the learning curve for the acquisition of laparoscopic skills on a virtual reality simulator. Surg Endosc 19:678–682
Duffy AJ, Hogle NJ, McCarthy H, Lew JI, Egan A, Christos P, Fowler DL (2005) Construct validity for the LAPSIM laparoscopic surgical simulator. Surg Endosc 19:401–405
Hassan I, Sitter H, Schlosser K, Zielke A, Rothmund M, Gerdes B (2005) Laparoskopiesimulator. Chirurg 76:151–156
Cosman PH, Hugh TJ, Shearer CJ, Merrett ND, Biankin AV, Cartmill JA (2007) Skills acquired on virtual reality laparoscopic simulators transfer into the operating room in a blinded, randomised, controlled trial. Stud Health Technol Inform 125:76–81
Mazzone E, Puliatti S, Amato M, Bunting B, Rocco B, Montorsi F, Mottrie A, Gallagher AG (2021) A systematic review and meta-analysis on the impact of proficiency-based progression simulation training on performance outcomes. Ann Surg 274:281–289
Zevin B, Aggarwal R, Grantcharov TP (2014) Surgical simulation in 2013: why is it still not the standard in surgical training? J Am Coll Surg 218:294–301
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71
Funding
Financial support was provided as part of a higher degree (C Toale) by the Royal College of Surgeons/Hermitage Medical Clinic Strategic Academic Recruitment (StAR MD) programme.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Mr Conor Toale, Dr Marie Morris and Mr Dara O. Kavanagh have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Toale, C., Morris, M. & Kavanagh, D.O. Training and assessment using the LapSim laparoscopic simulator: a scoping review of validity evidence. Surg Endosc 37, 1658–1671 (2023). https://doi.org/10.1007/s00464-022-09593-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09593-0