Abstract
Objectives
Postoperative pancreatic fistula (POPF) is the main complication of distal pancreatectomy (DP) and affects the prognosis of patients. The impact of several clinical factors mentioned in recent studies on POPF remains controversial. This study aimed to investigate the impact of a remnant pancreas and other perioperative factors on POPFs occurring after robot-assisted distal pancreatectomy (RDP) for nonmalignant pancreatic neoplasms.
Methods
A total of 197 patients who received robot-assisted distal pancreatectomy (RDP) for nonmalignant pancreatic neoplasms at the Pancreatic Disease Center, Ruijin Hospital Shanghai Jiaotong University School of Medicine from January 2018 to December 2020 were included in this retrospective study. According to the intraoperative transection plan, patients were divided into an RDP body group and an RDP tail group. Clinical and pathological features and perioperative factors affecting POPF were analyzed and compared between the two groups.
Results
The results showed that a transection plan involving the tail of the pancreas (OR = 2.133, 95% CI 1.109–4.103, p = 0.023) and spleen preservation (OR = 2.588, 95% CI 1.435–4.665, p = 0.001) independently increased the incidence of POPF in patients with nonmalignant pancreatic neoplasms treated by RDP. A transection plan involving the tail of the pancreas was also an independent risk factor (OR = 3.464, 95% CI 1.270–9.450, p = 0.015) for grade B/C POPF. Length of remnant pancreas > 6.23 cm was an independent risk factor for POPF (OR = 3.116, 95% CI 1.364–7.121, p = 0.007). Length of remnant pancreas > 9.82 cm was an independent risk factor for grade B/C POPF (OR = 3.340, 95% CI 1.386–8.051, p = 0.007).
Conclusion
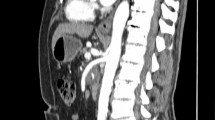
This retrospective study suggests that a transection plan involving the tail of the pancreas is an independent risk factor for POPF in patients with nonmalignant neoplasms treated by RDP. We also propose that the postoperative length of the remnant pancreas evaluated by computed tomography scans can be used to identify patients with a high risk of POPF in order to optimize the individualized strategy.


Similar content being viewed by others
References
Burk KS, Knipp D, Sahani DV (2018) Cystic pancreatic tumors. Magn Reson Imaging C 26:405–420
O’Grady HL, Conlon KC (2008) Pancreatic neuroendocrine tumours. Eur J Surg Oncol (EJSO) 34:324–332
Imamura T, Yamamoto Y, Sugiura T (2021) Reconsidering the optimal regional lymph node station according to tumor location for pancreatic cancer. Ann Surg Oncol 28:1602–1611
Zhou J, Lv Z, Zou H (2020) Up-to-date comparison of robotic-assisted versus open distal pancreatectomy: a PRISMA-compliant meta-analysis. Medicine (Baltimore) 99:e20435
Bassi C, Marchegiani G, Dervenis C (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 161:584–591
Miao Y, Lu Z, Yeo CJ (2020) Management of the pancreatic transection plane after left (distal) pancreatectomy: Expert consensus guidelines by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 168:72–84
Tomasello G, Ghidini M, Costanzo A (2019) Outcome of head compared to body and tail pancreatic cancer: a systematic review and meta-analysis of 93 studies. J Gastrointest Oncol 10:259–269
Galchina YS, Karmazanovsky GG, Kondratyev EV (2020) Contrast-enhanced computed tomography in evaluation of pancreatic stump volume in pancreaticoduodenectomy. Khirurgiya. Zhurnal im. N.I. Pirogova 31
Hirono S, Kawai M, Okada K (2021) Division of the pancreas at the neck reduces postoperative pancreatic fistula in laparoscopic distal pancreatectomy: comparison of pancreatic division at the body. Pancreatology 21:480–486
Klupp F, Klauss M, Rahbari NN (2020) Volume changes of the pancreatic head remnant after distal pancreatectomy. Surgery 167:455–467
Nakamura H, Murakami Y, Uemura K (2011) Reduced pancreatic parenchymal thickness indicates exocrine pancreatic insufficiency after pancreatoduodenectomy. J Surg Res 171:473–478
Klompmaker S, van der Vliet WJ, Thoolen SJ (2021) Procedure-specific training for robot-assisted distal pancreatectomy. Ann Surg 274:e18–e27
Pendola F, Gadde R, Ripat C (2017) Distal pancreatectomy for benign and low grade malignant tumors: short-term postoperative outcomes of spleen preservation—a systematic review and update meta-analysis. J Surg Oncol 115:137–143
Warshaw AL (1988) Conservation of the spleen with distal pancreatectomy. Arch Surg 123:550–553
Kimura W, Inoue T, Futakawa N (1996) Spleen-preserving distal pancreatectomy with conservation of the splenic artery and vein. Surgery 120:885–890
Weng Y, Jin J, Huo Z (2021) Robotic-assisted versus open distal pancreatectomy for benign and low-grade malignant pancreatic tumors: a propensity score-matched study. Surg Endosc 35:2255–2264
Tempero MA (2019) NCCN guidelines updates: pancreatic cancer. J Natl Compr Canc Netw 17:603–605
Bardol T, Delicque J, Hermida M (2020) Neck transection level and postoperative pancreatic fistula after pancreaticoduodenectomy: a retrospective cohort study of 195 patients. Int J Surg 82:43–50
Iacono C, Verlato G, Ruzzenente A (2013) Systematic review of central pancreatectomy and meta-analysis of central versus distal pancreatectomy. Brit J Surg 100:873–885
Lu X, Wang X, Fang Y (2016) Systematic review and meta-analysis of pancreatic amylase value on postoperative day 1 after pancreatic resection to predict postoperative pancreatic fistula. Medicine 95:e2569
Shi Y, Wang W, Qiu W (2021) Learning curve from 450 cases of robot-assisted pancreaticoduocectomy in a high-volume pancreatic center. Ann Surg 274:e1277–e1283
Wang S, Shyr B, Chen S (2018) Robotic distal pancreatectomy: comparison of spleen-preservation by the Warshaw technique and splenectomy. Int J Med Robot Comput Assist Surg 14:e1922
Lai EC, Tang CN (2013) Current status of robot-assisted laparoscopic pancreaticoduodenectomy and distal pancreatectomy: a comprehensive review. Asian J Endosc Surg 6:158–164
Djuric-Stefanovic A, Masulovic D, Kostic J (2012) CT volumetry of normal pancreas: correlation with the pancreatic diameters measurable by the cross-sectional imaging, and relationship with the gender, age, and body constitution. Surg Radiol Anat 34:811–817
Antoniou EA, Damaskos C, Garmpis N (2017) Solid pseudopapillary tumor of the pancreas: a single-center experience and review of the literature. In Vivo 31:501–510
Hasan A, Visrodia K, Farrell JJ (2019) Overview and comparison of guidelines for management of pancreatic cystic neoplasms. World J Gastroentero 25:4405–4413
Royall NA, Walsh RM (2017) Robotic distal pancreatectomy and splenectomy: rationale and technical considerations. J Vis Surg 3:135
Peng Y, Zhu X, Yin L (2017) Risk factors of postoperative pancreatic fistula in patients after distal pancreatectomy: a systematic review and meta-analysis. Sci Rep UK 7:185
Ecker BL, Mcmillan MT, Allegrini V (2019) Risk factors and mitigation strategies for pancreatic fistula after distal pancreatectomy. Ann Surg 269:143–149
Nagakawa Y, Sahara Y, Hosokawa Y (2017) The straightened splenic vessels method improves surgical outcomes of laparoscopic distal pancreatectomy. Digest Surg 34:289–297
Karabicak I, Satoi S, Yanagimoto H (2017) Comparison of surgical outcomes of three different stump closure techniques during distal pancreatectomy. Pancreatology 17:497–503
Hua Y, Javed AA, Burkhart RA (2017) Preoperative risk factors for conversion and learning curve of minimally invasive distal pancreatectomy. Surgery 162:1040–1047
Shi Y, Jin J, Qiu W (2020) Short-term outcomes after robot-assisted vs. open pancreaticoduodenectomy after the learning curve. Jama Surg 155:389
Kanda M, Fujii T, Suenaga M (2014) Estimated pancreatic parenchymal remnant volume accurately predicts clinically relevant pancreatic fistula after pancreatoduodenectomy. Surgery 156:601–610
Umezaki N, Hashimoto D, Nakagawa S (2018) Number of acinar cells at the pancreatic stump predicts pancreatic fistula after pancreaticoduodenectomy. Surg Today 48:790–795
Søreide K, Labori KJ (2016) Risk factors and preventive strategies for post-operative pancreatic fistula after pancreatic surgery: a comprehensive review. Scand J Gastroentero 51:1147–1154
Nishikawa M, Yamamoto J, Hoshikawa M (2020) Stapler sizes optimized for pancreatic thickness can reduce pancreatic fistula incidence after distal pancreatectomy. Surg Today 50:623–631
Melloul E, Lassen K, Roulin D (2020) Guidelines for perioperative care for pancreatoduodenectomy: enhanced recovery after surgery (ERAS) recommendations 2019. World J Surg 44:2056–2084
Kawaida H, Kono H, Hosomura N (2019) Surgical techniques and postoperative management to prevent postoperative pancreatic fistula after pancreatic surgery. World J Gastroentero 25:3722–3737
Acher AW, Stahl C, Barrett JR (2021) Clinical and cost profile of controlled grade b postoperative pancreatic fistula: rationale for their consideration as low risk. J Gastrointest Surg 25:2336–2343
Goess R, Ceyhan GO, Friess H (2016) Pancreatic exocrine insufficiency after pancreatic surgery. Panminerva Med 58:151–159
Kipp JP, Olesen SS, Mark EB (2019) Normal pancreatic volume in adults is influenced by visceral fat, vertebral body width and age. Abdom Radiol 44:958–966
Funding
This work was supported by the Guangci Clinical Technology Sailing Project (YW20210033).
Author information
Authors and Affiliations
Contributions
LQ, BW, and CW: study conception, writing of the manuscript, and creation of tables. LQ, BW, and XL: design and drawing of figures. LQ, BW, CW, XL, MC: acquisition and arrangement of data. LQ, BW, CW, XD and WW: analysis of data. WX, WW, and BS: critical revision.
Corresponding authors
Ethics declarations
Disclosures
Lihan Qian, Binwei Hu, Jiancheng Wang, Xiongxiong Lu, Xiaxing Deng, Weimin Chai, Zhiwei Xu, Weishen Wang, and Baiyong Shen have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qian, L., Hu, B., Wang, J. et al. Impact of the transection plan on postoperative pancreatic fistulas occurring after robot-assisted distal pancreatectomy for nonmalignant pancreatic neoplasms. Surg Endosc 37, 309–318 (2023). https://doi.org/10.1007/s00464-022-09489-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09489-z