Abstract
Background
Despite standardization, the 2016 ISGPF criteria are limited by their wider applicability and oversimplification of grade B POPF. This work applied the 2016 ISGPF grading criteria within a US academic cancer center to verify clinical and fiscal distinctions and sought to improve grading criteria for grade B POPF.
Methods
The 2008–2018 cost and NSQIP data from pancreaticoduodenectomy to postoperative day 90 were merged. All POPFs were coded by 2016 ISGPF criteria. The Clavien-Dindo Classification (CD) defined complication severity. On sub-analyses, grade B POPFs were divided into those with adequate drainage and those requiring additional drainage. Chi-square, ANOVA, and Fisher’s least significant difference test were employed.
Results
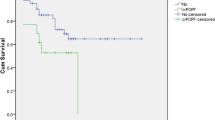
Two hundred thirty-two patients were in the final analyses, 72 (31%) of whom had POPFs: 16 (7%) biochemical leaks, 54 (23%) grade B (28% required additional drainage), and 2 (1%) grade C. There was no significant difference in length of stay, CD, readmission, or cost in patients without a POPF, with biochemical leak or grade B POPF. On sub-analyses, 92% of adequately drained grade B POPFs had CD 1–2 and readmission equivalent to patients without POPF (p > 0.05). One hundred percent of grade B POPF requiring drainage had CD 3–4a, and 67% were readmitted. Cost was significantly increased in grade B POPF requiring additional drainage (p = 0.02) and grade C POPF (p < 0.01).
Conclusions
This analysis did not confirm an incremental increase in morbidity and cost with POPF grade. Sub-analyses enabled accurate clinical and cost distinctions in grade B POPF; adequately drained grade B POPF are low risk and clinically insignificant.


Similar content being viewed by others
References
Bassi, C., et al., Pancreatic fistula rate after pancreatic resection. The importance of definitions. Dig Surg, 2004. 21(1): p. 54-9.
Bassi, C., et al., The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery, 2017. 161(3): p. 584-591.
Butturini, G., et al., Pancreatic fistula: definition and current problems. J Hepatobiliary Pancreat Surg, 2008. 15(3): p. 247-51.
Bassi, C., et al., Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery, 2005. 138(1): p. 8-13.
Daskalaki, D., et al., A grading system can predict clinical and economic outcomes of pancreatic fistula after pancreaticoduodenectomy: results in 755 consecutive patients. Langenbecks Arch Surg, 2011. 396(1): p. 91-8.
Kim, W.S., et al., Clinical validation of the ISGPF classification and the risk factors of pancreatic fistula formation following duct-to-mucosa pancreaticojejunostomy by one surgeon at a single center. J Gastrointest Surg, 2011. 15(12): p. 2187-92.
Pratt, W.B., et al., Clinical and economic validation of the International Study Group of Pancreatic Fistula (ISGPF) classification scheme. Ann Surg, 2007. 245(3): p. 443-51.
Pratt, W.B., M.P. Callery, and C.M. Vollmer, Jr., Risk prediction for development of pancreatic fistula using the ISGPF classification scheme. World J Surg, 2008. 32(3): p. 419-28.
Pulvirenti, A., et al., Clinical Implications of the 2016 International Study Group on Pancreatic Surgery Definition and Grading of Postoperative Pancreatic Fistula on 775 Consecutive Pancreatic Resections. Ann Surg, 2018. 268(6): p. 1069-1075.
Marchegiani, G., et al., Current Definition of and Controversial Issues Regarding Postoperative Pancreatic Fistulas. Gut Liver, 2019. 13(2): p. 149-153.
Roberts, R.R., et al., Distribution of variable vs fixed costs of hospital care. JAMA, 1999. 281(7): p. 644-9.
Dindo, D., N. Demartines, and P.A. Clavien, Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg, 2004. 240(2): p. 205-13.
Kim, H.Y., Analysis of variance (ANOVA) comparing means of more than two groups. Restor Dent Endod, 2014. 39(1): p. 74-7.
Maggino, L., et al., Decoding Grade B Pancreatic Fistula: A Clinical and Economical Analysis and Subclassification Proposal. Ann Surg, 2019. 269(6): p. 1146-1153.
Kitahata, Y., M. Kawai, and H. Yamaue, Clinical trials to reduce pancreatic fistula after pancreatic surgery-review of randomized controlled trials. Transl Gastroenterol Hepatol, 2016. 1: p. 4.
Funding
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Number T32 CA090217. This content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
Alexandra W. Acher MD: Study design, data acquisition, data analysis and interpretation, manuscript writing and critical revision, final review and approval.
James R. Barrett MD: Study design, interpretation of analysis, manuscript critical revision, manuscript final review and approval.
Patrick B. Schwartz MD: Study design, interpretation of analysis, manuscript critical revision, manuscript final review and approval.
Christopher Stahl MD: Study design, interpretation of analysis, manuscript critical revision, manuscript final review and approval.
Taylor Aiken MD: Study design, interpretation of analysis, manuscript critical revision, manuscript final review and approval.
Sean Ronnekleiv-Kelly MD: Study design, interpretation of analysis, manuscript critical revision, manuscript final review and approval.
Rebecca M. Minter MD: Study design, interpretation of analysis, manuscript critical revision, manuscript final review and approval.
Glen Leverson PhD: Study design, data analysis, interpretation of analysis, manuscript critical revision, manuscript final review and approval.
Sharon M. Weber MD: Study design, interpretation of analysis, manuscript critical revision, manuscript final review and approval.
Daniel E. Abbott MD: Study design, interpretation of analysis, manuscript critical revision, manuscript final review and approval.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Acher, A.W., Stahl, C., Barrett, J.R. et al. Clinical and Cost Profile of Controlled Grade B Postoperative Pancreatic Fistula: Rationale for Their Consideration as Low Risk. J Gastrointest Surg 25, 2336–2343 (2021). https://doi.org/10.1007/s11605-021-04928-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-04928-z