Abstract
Introduction
There are a paucity of data regarding the safety of laparoscopic inguinal hernia repair in patients on antiplatelet and anticoagulant therapy (APT/ACT). We aim to compare the postoperative outcomes of laparoscopic (LIHR) vs. open repair of inguinal hernias (OIHR) in patients on APT/ACT.
Method
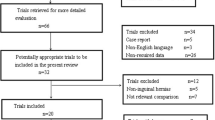
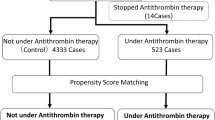
We conducted a retrospective cohort study using the Vizient Clinical DataBase. We included adults receiving APT/ACT who underwent outpatient, elective, and primary inguinal hernia repair between 2017 and 2019. Subgroup analysis was performed on patients receiving aspirin, non-aspirin antiplatelet, and anticoagulant therapy. Mixed-effects logistic regression was used to assess both the effect of APT/ACT on the probability of receiving LIHR vs OIHR and their respective outcomes.
Result
A total of 142,052 repairs were included, of which 21,441 (15%) were performed on patients receiving APT/ACT. Mean age was 69 years (± 10.5) and 93% were male. 19% of hernias were bilateral. 40% of operations were performed at teaching hospitals. On multivariable analysis, patients on non-aspirin antiplatelet or anticoagulant therapy were more likely to receive an open procedure (Odds Ratio (OR) = 1.2; 95% Confidence Intervals (CI) [1.1, 1.4] and OR = 1.4; CI [1.3, 1.5], respectively). LIHR was associated with a lower rate of length of stay > 1 day (OR = 0.65; CI [0.5, 0.9]). Rates of 30-day postoperative hematoma, transfusions, stroke, myocardial infarction, deep venous thrombosis, pulmonary embolism, readmission, and emergency department visits were similar between the two operative approaches.
Conclusion
Patients on APT/ACT represent a substantial proportion of those undergoing inguinal hernia repair. Non-aspirin antiplatelet or anticoagulant therapy are independent predictors of choosing an open repair. Laparoscopic repair appears to be safe in patients receiving APT/ACT under current perioperative management patterns.


Similar content being viewed by others
References
Hammoud M, Gerken J (2021) Inguinal Hernia, StatPearls [Internet]. StatPearls Publishing, Treasure Island, FL
(2018) International guidelines for groin hernia management. Hernia 22(1): 1–165. doi: https://doi.org/10.1007/s10029-017-1668-x
Morales-Conde S, Socas M, Fingerhut A (2012) Endoscopic surgeons’ preferences for inguinal hernia repair: TEP, TAPP, or OPEN. Surg Endosc 26(9):2639–2643. https://doi.org/10.1007/s00464-012-2247-y
Ashburner JM, Singer DE, Lubitz SA, Borowsky LH, Atlas SJ (2017) Changes in use of anticoagulation in patients with atrial fibrillation within a primary care network associated with the introduction of direct oral anticoagulants. Am J Cardiol 120(5):786–791. https://doi.org/10.1016/j.amjcard.2017.05.055
McLemore EC, Harold KL, Cha SS, Johnson DJ, Fowl RJ (2006) The safety of open inguinal herniorraphy in patients on chronic warfarin therapy. Am J Surg 192(6):860–864. https://doi.org/10.1016/j.amjsurg.2006.08.058
Ong W, Shen T, Tan WB, Lomanto D (2016) Is preoperative withdrawal of aspirin necessary in patients undergoing elective inguinal hernia repair? Surg Endosc 30(12):5542–5549. https://doi.org/10.1007/s00464-016-4926-6
Chu EW, Telem DA, Chernoguz A, Divino CM (2011) Assessing the risk of clopidogrel-related bleeding complications in patients undergoing inguinal herniorrhaphy. Hernia 15(1):31–35. https://doi.org/10.1007/s10029-010-0732-6
Vizient, Inc., Irving, TX. 2021. http://vizientinc.com.
Harrell FE (2010) Regression modeling strategies with applications to linear models, logistic regression and survival-analysis, 2nd edn. Springer, New York
Aiolfi A, Cavalli M, Del Ferraro S, Manfredini L, Bonitta G, Bruni PG et al (2021) Treatment of inguinal hernia: systematic review and updated network meta-analysis of randomized controlled trials. Ann Surg. https://doi.org/10.1097/sla.0000000000004735
Dedemadi G, Sgourakis G, Radtke A, Dounavis A, Gockel I, Fouzas I et al (2010) Laparoscopic versus open mesh repair for recurrent inguinal hernia: a meta-analysis of outcomes. Am J Surg 200(2):291–297. https://doi.org/10.1016/j.amjsurg.2009.12.009
Li J, Wang M, Cheng T (2019) The safe and risk assessment of perioperative antiplatelet and anticoagulation therapy in inguinal hernia repair, a systematic review. Surg Endosc 33(10):3165–3176. https://doi.org/10.1007/s00464-019-06956-y
Köckerling F, Roessing C, Adolf D, Schug-Pass C, Jacob D (2016) Has endoscopic (TEP, TAPP) or open inguinal hernia repair a higher risk of bleeding in patients with coagulopathy or antithrombotic therapy? Data from the Herniamed Registry. Surg Endosc 30(5):2073–2081. https://doi.org/10.1007/s00464-015-4456-7
Peng M, Southern DA, Williamson T, Quan H (2017) Under-coding of secondary conditions in coded hospital health data: Impact of co-existing conditions, death status and number of codes in a record. Health Informatics J 23(4):260–267. https://doi.org/10.1177/1460458216647089
Nouraei SA, Virk JS, Hudovsky A, Wathen C, Darzi A, Parsons D (2016) Accuracy of clinician-clinical coder information handover following acute medical admissions: implication for using administrative datasets in clinical outcomes management. J Public Health (Oxf) 38(2):352–362. https://doi.org/10.1093/pubmed/fdv041
Chen Y, Zivkovic M, Wang T, Su S, Lee J, Bortnichak EA (2018) A systematic review of coding systems used in pharmacoepidemiology and database research. Methods Inf Med 57(1):1–42. https://doi.org/10.3414/me17-05-0006
Hornor MA, Duane TM, Ehlers AP, Jensen EH, Brown PS Jr, Pohl D et al (2018) American college of surgeons’ guidelines for the perioperative management of antithrombotic medication. J Am Coll Surg 227(5):521–36.e1. https://doi.org/10.1016/j.jamcollsurg.2018.08.183
Biccard BM, Sigamani A, Chan MTV, Sessler DI, Kurz A, Tittley JG et al (2018) Effect of aspirin in vascular surgery in patients from a randomized clinical trial (POISE-2). Br J Surg 105(12):1591–1597. https://doi.org/10.1002/bjs.10925
Chu EW, Chernoguz A, Divino CM (2016) The evaluation of clopidogrel use in perioperative general surgery patients: a prospective randomized controlled trial. Am J Surg 211(6):1019–1025. https://doi.org/10.1016/j.amjsurg.2015.05.036
Stucky CC, Garvey EM, Johnson DJ, Chapital AB, Gossage CM, Wasif N et al (2015) Challenging a surgical dictum: results from a 10-year experience on the safety of open inguinal herniorrhaphy in patients on chronic warfarin therapy. Hernia 19(1):83–87. https://doi.org/10.1007/s10029-014-1257-1
Beyer-Westendorf J, Gelbricht V, Förster K, Ebertz F, Köhler C, Werth S et al (2014) Peri-interventional management of novel oral anticoagulants in daily care: results from the prospective Dresden NOAC registry. Eur Heart J 35(28):1888–1896. https://doi.org/10.1093/eurheartj/eht557
Acknowledgements
We would like to acknowledge the staff at Vizient for their provision of the data and technical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Mazen Al-Mansour has received educational payments from Intuitive Surgical, Inc. and general payments (food and beverage) from W. L Gore & Associated, Inc. and ConMed Corporation. Jeremy A. Balch, Dan Neal, Cristina Crippen, Crystal N. Johnson-Mann, Thomas E. Read, and Tyler J. Loftus have no disclosures to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Balch, J.A., Neal, D., Crippen, C. et al. Safety of laparoscopic inguinal hernia repair in the setting of antithrombotic therapy. Surg Endosc 36, 9011–9018 (2022). https://doi.org/10.1007/s00464-022-09360-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09360-1