Abstract
Background
Recently, in the field of abdominal wall repair surgery, some minimally invasive procedures introduced the use of staplers to provide a retromuscular prosthetic repair. However, to the knowledge of the authors, there are little data in the literature about the outcomes of stapled sutures adoption for midline reconstruction. This study aims to investigate the biomechanics of stapled sutures, simple (stapled), or oversewn (hybrid), in comparison with handsewn suture. From the results obtained, we tried to draw indications for their use in a clinical context.
Methods
Human cadaver fascia lata specimens, sutured (handsewn, stapled, or hybrid) or not, underwent tensile tests. The data on strength (maximal stress), ultimate strain (deformability), Young’s modulus (rigidity), and dissipated specific energy (ability to absorb mechanical energy up to the breaking point) were recorded for each type of specimens and analyzed.
Results
Stapled and hybrid suture showed a significantly higher strength (handsewn 0.83 MPa, stapled 2.10 MPa, hybrid 2.68 MPa) and a trend toward a lower ultimate strain as compared to manual sutures (handsewn 344%, stapled 249%, hybrid 280%). Stapled and hybrid sutures had fourfold higher Young’s modulus as compared to handsewn sutures (handsewn 1.779 MPa, stapled 7.374 MPa, hybrid 6.964 MPa). Handsewn and hybrid sutures showed significantly higher dissipated specific energy (handsewn 0.99 mJ-mm3, stapled 0.73 mJ-mm3, hybrid 1.35 mJ-mm3).
Conclusion
Stapled sutures can resist high loads, but are less deformable and rigid than handsewn suture. This suggests a safer employment in case of small defects or diastasis (< W1 in accord to EHS classification), where the presumed tissutal displacement is minimal.
Oversewing a stapled suture improves its efficiency, becoming crucial in case of larger defects (> W1 in accord to EHS classification) where the expected tissutal displacement is maximal. Hybrid sutures seem to be a good compromise.






Similar content being viewed by others
References
LeBlanc KA, Booth WV (1993) Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc 3:39–41
Bittner R, Bain K, Bansal VK, Berrevoet F, Bingener-Casey J, Chen D, Chen J, Chowbey P, Dietz UA, de Beaux A, Ferzli G, Fortelny R, Hoffmann H, Iskander M, Ji Z, Jorgensen LN, Khullar R, Kirchhoff P, Köckerling F, Kukleta J, LeBlanc K, Li J, Lomanto D, Mayer F, Meytes V, Misra M, Morales-Conde S, Niebuhr H, Radvinsky D, Ramshaw B, Ranev D, Reinpold W, Sharma A, Schrittwieser R, Stechemesser B, Sutedja B, Tang J, Warren J, Weyhe D, Wiegering A, Woeste G, Yao Q (2019) Update of Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))—Part A. Surg Endosc 33:3069–3139. https://doi.org/10.1007/S00464-019-06907-7/FIGURES/4
Claus CMP, Malcher F, Cavazzola LT, Furtado M, Morrell A, Azevedo M, Meirelles LG, Santos H, Garcia R (2018) Subcutaneous onlay laparoscopic approach (SCOLA) for ventral hernia and rectus abdominis diastasis repair: technical description and initial results. Arq Bras Cir Dig 31:1–5. https://doi.org/10.1590/0102-672020180001e1399
Chowbey PK, Sharma A, Khullar R, Soni V, Baijal M (2003) Laparoscopic ventral hernia repair with extraperitoneal mesh: surgical technique and early results. Surg Laparosc Endosc Percutaneous Tech 13:101–105. https://doi.org/10.1097/00129689-200304000-00008
Schwarz J, Reinpold W, Bittner R (2017) Endoscopic mini/less open sublay technique (EMILOS)-a new technique for ventral hernia repair. Langenbeck’s Arch Surg 402:173–180. https://doi.org/10.1007/s00423-016-1522-0
Jani K, Contractor S (2019) Retrorectus sublay mesh repair using polypropylene mesh: Cost-effective approach for laparoscopic treatment of ventral abdominal wall hernias. J Min Access Surg 15:287–292. https://doi.org/10.4103/jmas.JMAS_20_19
Li B, Qin C, Bittner R (2018) Totally endoscopic sublay (TES) repair for midline ventral hernia: surgical technique and preliminary results. Surg Endosc 34(4):1543–1550. https://doi.org/10.1007/S00464-018-6568-3
Andreuccetti J, Sartori A, Lauro E, Crepaz L, Sanna S, Pignata G, Bracale U, di Leo A (2021) Extended totally extraperitoneal rives-stoppa (eTEP-RS) technique for ventral hernia: initial experience of The Wall Hernia Group and a surgical technique update. Updates Surg 73(5):1955–1961. https://doi.org/10.1007/S13304-021-01067-7
Abdalla RZ, Garcia RB, da Costa RID, Abdalla BMZ (2013) Treatment of mid-line abdominal wall hernias with the use of endo-stapler for mid-line closure. Arq Bras Cir Dig 26:335–337. https://doi.org/10.1590/S0102-67202013000400016
Costa TN, Abdalla RZ, Santo MA, Tavares RRFM, Abdalla BMZ, Cecconello I (2016) Transabdominal midline reconstruction by minimally invasive surgery: technique and results. Hernia 20(2):257–265. https://doi.org/10.1007/S10029-016-1457-Y
Moore AM, Anderson LN, Chen DC (2016) Laparoscopic stapled sublay repair with self-gripping mesh: a simplified technique for minimally invasive extraperitoneal ventral hernia repair. Surg Technol Int 29:131–139
Nguyen DK, Chen DC (2017) Laparoendoscopic stapled rives stoppa sublay technique for extraperitoneal ventral hernia repair. Eur Surg 49:175–179. https://doi.org/10.1007/S10353-017-0483-Z
Carrara A, Lauro E, Fabris L, Frisini M, Rizzo S (2019) Endo-laparoscopic reconstruction of the abdominal wall midline with linear stapler, the THT technique. Early results of the first case series. Ann Med Surg 38:1–7. https://doi.org/10.1016/J.AMSU.2018.12.002
Maeda K, Maruta M, Utsumi T, Sato H, Masumori K, Matsumoto M (2002) Minimally invasive surgery for carcinoid tumors in the rectum. Biomed Pharmacother 56(Suppl 1):222s–226s. https://doi.org/10.1016/s0753-3322(02)00218-4
Tejedor P, Sagias F, Nock D, Flashman K, Naqvi S, Kandala NL, Khan JS (2019) Advantages of using a robotic stapler in rectal cancer surgery. J Robot Surg 14(2):365–370. https://doi.org/10.1007/S11701-019-00993-4
Roberts KE, Renee Hilton L, Friedman DT, Frieder JS, Zhang X, Duffy AJ (2018) Safety and feasibility of a lower-cost stapler in bariatric surgery. Obes Surg 29(2):401–405. https://doi.org/10.1007/S11695-018-3580-6
Müller-Stich B, Schmidt T, Nienhüser H, Nickel F, Billeter A, Diener M, Ulrich A, Büchler MW (2020) Total-minimalinvasive Ösophagektomie. Chirurg 91(1):13–14. https://doi.org/10.1007/S00104-020-01152-4
Makanyengo SO, Thiruchelvam D (2020) Literature review on the incidence of primary stapler malfunction. Surg Innov 27:229–234. https://doi.org/10.1177/1553350619889274
Gossot D, Merlusca G, Tudor A, Boudaya MS, Radu C, Magdeleinat P (2008) Pitfalls related to the use of endostaplers during video-assisted thoracic surgery. Surg Endosc 23(1):189–192. https://doi.org/10.1007/S00464-008-9765-7
Yano M, Yokoi K, Numanami H, Kondo R, Ohde Y, Sugaya M, Narita K, Chihara K, Matsushima Y, Kobayashi R, Hikosaka Y (2013) Complications of bronchial stapling in thoracic surgery. World J Surg 38(2):341–346. https://doi.org/10.1007/S00268-013-2292-2
Major P, Wysocki M, Pędziwiatr M, Pisarska M, Małczak P, Wierdak M, Dembiński M, Migaczewski M, Rubinkiewicz M, Budzyński A (2018) More stapler firings increase the risk of perioperative morbidity after laparoscopic sleeve gastrectomy. Videosurg Other Miniinvasive Tech 13:88–94. https://doi.org/10.5114/wiitm.2017.70197
Lundvall E, Ottosson J, Stenberg E (2019) The influence of staple height on postoperative complication rates after laparoscopic gastric bypass surgery using linear staplers. Surg Obes Relat Dis 15:404–408. https://doi.org/10.1016/J.SOARD.2019.01.017
Nordholm-Carstensen A, Rasmussen MS, Krarup PM (2019) Increased leak rates following stapled versus handsewn ileocolic anastomosis in patients with right-sided colon cancer: a nationwide cohort study. Dis Colon Rectum 62:542–548. https://doi.org/10.1097/DCR.0000000000001289
Lin S, Li C, Guan W, Liang H (2021) Can staple-line reinforcement eliminate the major early postoperative complications after sleeve gastrectomy? Asian J Surg 44:836–840. https://doi.org/10.1016/j.asjsur.2020.12.036
Baqar AR, Wilkins S, Staples M, Oliva K, McMurrick P (2020) The post-operative impact of oversewing stapled anastomoses in colorectal cancer surgery: a retrospective Australian cohort study. Int J Surg Open 24:91–95. https://doi.org/10.1016/j.ijso.2020.04.004
Demeusy A, Sill A, Averbach A (2018) Current role of staple line reinforcement in 30-day outcomes of primary laparoscopic sleeve gastrectomy: an analysis of MBSAQIP data, 2015–2016 PUF. Surg Obes Relat Dis 14:1454–1461. https://doi.org/10.1016/J.SOARD.2018.06.024
Yo LSF, Consten ECJ, Quarles Van Ufford HME, Gooszen HG, Gagner M (2007) Buttressing of the staple line in gastrointestinal anastomoses: overview of new technology designed to reduce perioperative complications. Dig Surg 23:283–291
Carrara A, Catarci M, Fabris L, Zuolo M, Pellecchia L, Moscatelli P, Dorna A, Motter M, Pertile R, Tirone G (2021) Prospective observational study of abdominal wall reconstruction with THT technique in primary midline defects with diastasis recti: clinical and functional outcomes in 110 consecutive patients. Surg Endosc 35:5104–5114. https://doi.org/10.1007/s00464-020-07997-4
Paolin A, Spagnol L, Battistella G, Trojan D (2018) Evaluation of allograft decontamination with two different antibiotic cocktails at the treviso tissue bank foundation. PLoS ONE. https://doi.org/10.1371/journal.pone.0201792
Otsuka S, Yakura T, Ohmichi Y, Ohmichi M, Naito M, Nakano T, Kawakami Y (2018) Site specificity of mechanical and structural properties of human fascia lata and their gender differences: a cadaveric study. J Biomech 77:69–75. https://doi.org/10.1016/j.jbiomech.2018.06.018
Gras LL, Laporte S, Mitton D, Crevier‐Denoix N, Viot P (2012) Tensile tests on a muscle: influence of experimental conditions and of velocity on its passive response. In: 2012 IRCOBI Conference Location: Dublin, Ireland. https://trid.trb.org/view/1254086. Accessed 7 Mar 2022
Israelsson LA (2015) Abdominal incision closure: small but important bites. Lancet 386:1216–1218. https://doi.org/10.1016/S0140-6736(15)60687-0
Henderson ER, Friend EJ, Toscano MJ, Parsons KJ, Tarlton JF (2015) Biomechanical comparison of canine fascia lata and thoracolumbar fascia: an in vitro evaluation of replacement tissues for body wall reconstruction. Vet Surg 44:126–134. https://doi.org/10.1111/J.1532-950X.2014.12247.X
Deeken CR, Lake SP (2017) Mechanical properties of the abdominal wall and biomaterials utilized for hernia repair. J Mech Behav Biomed Mater 74:411–427
Okami J, Tokunaga T, Kanou T, Kunou H, Ishida D, Fujiwara A, Ito Y, Higashiyama M (2017) Randomized study comparing equal height staples with graduated height staples in bronchial closure. Ann Thorac Surg 104:1012–1019. https://doi.org/10.1016/j.athoracsur.2017.02.070
Shimizu N, Tarlton J, Friend E, Doran I, Parsons K (2017) Tensile comparison of polydioxanone, polyglyconate, and barbed glycolide-trimethylene carbonate suture in canine cadaveric tensor fascia lata. Vet Surg 46:89–94. https://doi.org/10.1111/VSU.12580
Barber FA, Coons DA, Ruiz-Suarez M (2008) Cyclic load testing and ultimate failure strength of biodegradable glenoid anchors. Arthroscopy 24:224–228. https://doi.org/10.1016/J.ARTHRO.2007.08.011
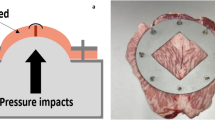
Kallinowski F, Ludwig Y, Löffler T, Vollmer M, Lösel PD, Voß S, Görich J, Heuveline V, Nessel R (2021) Biomechanics applied to incisional hernia repair—considering the critical and the gained resistance towards impacts related to pressure. Clin Biomech. https://doi.org/10.1016/j.clinbiomech.2020.105253
Kallinowski F, Gutjahr D, Harder F, Sabagh M, Ludwig Y, Lozanovski VJ, Löffler T, Rinn J, Görich J, Grimm A, Vollmer M, Nessel R (2021) The grip concept of incisional hernia repair—dynamic bench test, CT Abdomen with Valsalva and 1-year clinical results. Front Surg. https://doi.org/10.3389/fsurg.2021.602181
Sekine Y, Sugo H, Iwanaga N, Neshime S, Watanobe I (2020) Relaparotomy two years after incisional hernia repair using a free fascia lata graft. Case Rep Surg 2020:1–4. https://doi.org/10.1155/2020/1769404
Morse LJ, Barb JS (1943) Free autoplastic transplants of fascia lata in the repair of large incisional hernia. Surgery 13:524–534. https://doi.org/10.5555/URI:PII:S0039606043903691
Goto A, Matsuhashi N, Takahashi T, Tanahashi T, Matsui S, Imai H, Tanaka Y, Yamaguchi K, Yoshida K (2020) Feasibility of the reconstruction with fascia lata patch on the abdominal wall defect after resection of the abdominal desmoid tumor. Clin Exp Gastroenterol 13:249–254. https://doi.org/10.2147/CEG.S249870
Sugo H, Kawai M, Miyano S, Watanobe I, Machida M, Kitabatake T, Lee Y, Kojima K (2019) Surgical repair with free fascia lata graft in patients at risk of surgical site infection: a case series. Int Surg 104:69–74. https://doi.org/10.9738/INTSURG-D-17-00053.1
Miyamoto Y, Watanabe M, Ishimoto T, Baba Y, Iwagami S, Sakamoto Y, Yoshida N, Masuguchi S, Ihn H, Baba H (2015) Fascia lata onlay patch for repairing infected incisional hernias. Surg Today 45:121–124. https://doi.org/10.1007/s00595-014-0936-y
Kim JC, Lee YK, Lim BS, Rhee SH, Yang HC (2007) Comparison of tensile and knot security properties of surgical sutures. J Mater Sci 18:2363–2369. https://doi.org/10.1007/s10856-007-3114-6
Kerr AS, Osende J, Fallon JT, Badimon J (2001) Aortic slimgraft: ex vivo and in vivo study. J Vasc Surg 34:350–352. https://doi.org/10.1067/MVA.2001.115814
Patterson T, Witberg G, Redwood S, Prendergast B (2019) Balloon valve fracture at the time of valve-in-valve transcatheter aortic valve replacement: ex vivo modeling and clinical implications. JACC 12:76–77. https://doi.org/10.1016/J.JCIN.2018.11.021
Acknowledgements
The authors thank the University of Trento and the San Camillo Hospital of Trento for their support. The authors also thank the Treviso Tissue Bank Foundation (FBTV) for providing the anatomic specimens. Special thanks to Prof. Davide Lomanto of the National University of Singapore for his valuable advice.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
The corresponding authors confirm that each author named in the by-line qualify by having participated actively and sufficiently in the study.
Corresponding authors
Ethics declarations
Disclosures
Enrico Lauro, Ilaria Corridori, Lorenzo Luciani, Alberto Di Leo, Alberto Sartori, Jacopo Andreuccetti, Diletta Trojan, Giovanni Scudo, Antonella Motta, and Nicola M. Pugno have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lauro, E., Corridori, I., Luciani, L. et al. Stapled fascial suture: ex vivo modeling and clinical implications. Surg Endosc 36, 8797–8806 (2022). https://doi.org/10.1007/s00464-022-09304-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09304-9