Abstract
Objective
We aimed to investigate compensatory hyperhidrosis (CH) and recurrence based on an online survey of patients who underwent endoscopic thoracic sympathicotomy(ETS) for palmar and/or axillary hyperhidrosis.
Methods
We enrolled 231 patients who underwent ETS for palmar and/or axillary hyperhidrosis from January 2008 to April 2021. Patients responded to an online questionnaire regarding CH and recurrence, their electronic medical records were reviewed. Logistic regression was performed to find the risk factors related to CH and recurrence.
Results
The median time of survey from surgery was 20 months. Although 94% of patients were satisfied with the surgery, 86.1% experienced CH; of them, it was severe in 30.7%. Three months after surgery, there was no long-term change in the severity of CH. The development of CH showed a close relationship with age of 20 years or more (OR: 2.73). Recurrence occurred in 44(19.0%) patients, and the use of anti-adhesive agents was a significant preventive factor against recurrence after ETS (OR: 0.42).
Conclusions
We observed that CH and recurrence after ETS for palmar and/or axillary hyperhidrosis were relatively common. Age at the time of surgery was associated with CH, and the use of anti-adhesive agents showed to lower the risk of recurrence after ETS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Endoscopic thoracic sympathicotomy (ETS) with interruption of the sympathetic chain is the treatment of choice for patients with primary hyperhidrosis [1]. Despite the successful outcome of ETS, compensatory hyperhidrosis (CH), which produces subjective and objectively increased sweating in other body segments that did not have hyperhidrosis prior to surgery, is a well-known side effect. Recurrence after surgery, which occurs with re-sweating on the affected area, is also common cause of dissatisfaction among patients who underwent ETS [2]. Therefore, other treatment modalities have been introduced and explored to avoid or manage CH and recurrent hyperhidrosis [3,4].
The rate of CH after ETS has been shown to range from 3 to 100% [1,5,6]. Previous studies evaluating the risk factors related to CH have paid particular attention to the level of sympathicotomy, age, body mass index, sympathetic ganglion excitability, or type of surgery [7,8,9,10,11]. Meanwhile, the recurrence rate of hyperhidrosis after ETS has been reported to range from 0 to 65% [12,13]. To investigate the possible factors causing recurrence, previous studies focused on the strategy and completeness of surgery [1].
In this study, we aimed to investigate the incidence, severity, distribution, and temporal aspect of CH based on an online survey of patients who underwent ETS for palmar and/or axillary hyperhidrosis. Moreover, we also analysed our surgical strategy in detail to identify possible preventive factors for recurrence after ETS.
Methods
Study population and design
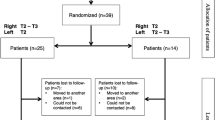
An online survey questionnaire request was sent to patients who previously underwent ETS for palmar and/or axillary hyperhidrosis at our institution between January 2008 and April 2021. Informed consent was received via an online process; then, their electronic medical records were reviewed. A text message, which explained the purpose of the study, was sent via U-severance 3.0 Information Technology Service Management in our institution. This study was approved by the Institutional Review Board of our institution (Approval No. 3–2021-0018). Of the 826 eligible patients, 248 (30.0%) patients consented to participate in the study and answered the online questionnaire. Of the 248 respondents, 231 (93.1%) patients answered all the questions appropriately, and as such, they were finally included in this study.
Online survey
The online survey was performed using Google Forms, and code numbers were used to avoid disclosing patients’ names or other personally identifiable information. The questionnaire contained 35 questions in 6 sections: demographic variables, preoperative treatment, current status of palmar and/or axillary hyperhidrosis, concurrent hyperhidrosis (e.g., gustatory or plantar), compensatory hyperhidrosis, and recurrence after surgery. To assess the severity of hyperhidrosis, we used the Hyperhidrosis Disease Severity Score (HDSS) [14]. The HDSS has only one question with four options; hence, it is an easy method to assess the severity of hyperhidrosis. Additionally, this method has been validated in other studies, and it is the most commonly used assessment tool for hyperhidrosis [15]. The four scores in HDSS were as follows:
(1) HDSS 1: My sweating is never noticeable and never interferes with my daily activities.
(2) HDSS 2: My sweating is tolerable but sometimes interferes with my daily activities.
(3) HDSS 3: My sweating is barely tolerable and frequently interferes with my daily activities.
(4) HDSS 4: My sweating is intolerable and always interferes with my daily activities.
We reviewed participants' electronic medical records to have more precise information in terms of the quality of life and complications, such as recurrence or compensatory hyperhidrosis. When there was a discrepancy between the online answers and medical records, we prioritized the information on the medical records to minimize possible biases from patients. However, respondents who had surgery prior to 2019 did not have sufficient data due to limited information.
Surgery
Under general anaesthesia, all patients underwent ETS using a bilateral simultaneous two-portal video-assisted thoracoscopic surgery (VATS). From January 2008 to July 2014, R3 or R4 clipping was performed. However, our institution had adopted a new approach starting in November 2014, whereby it shifted to R4 or R4-R5 sympathicotomy as the principal surgical strategy. Patients were put in a semi-seated position and two 3 mm incisions were made on each side; one for the thoracoscope at the 4th intercostal space (ICS) on the mid-axillary line, and another for instruments at the 3rd ICS on the anterior axillary line. After the installation of carbon dioxide gas, sympathicotomy was performed. The transection range was extended by about 2 cm, laterally along the surface with continuity from the sympathicotomy lesion, to complete the interruption of the potential bypass nerve fibers. We routinely conducted the operation on the right side first to view the imbalanced innervation of the heart by bilateral sympathetic nerves. In addition, we started using anti-adhesive agents beginning in September 2018, after observing severe lung adhesion around the sympathicotomy area of patients who revisited for a second surgery due to recurrence. The same procedure was performed on the left side. To prevent visceral pleural adhesion at the sympathicotomy site, we sprayed an anti-adhesive barrier agent (hyaluronic acid, InterBlock, BioPlus Company, Seongnam, South Korea) onto the sympathicotomy site, using a long-dispensing needle. This measure was taken because we firmly believe that visceral pleural adhesion after sympathicotomy may be a dominant contributing factor to recurrence. After the completion of ETS, a 10-Fr chest tube was placed in the pleural cavity, while inflating the lungs, and the chest tube was removed once the air ceased to escape. Postoperative routine chest radiography was obtained in all patients prior to extubation in the operating room to detect signs of pneumothorax. Most patients were discharged on the same day or the following day.
Statistical analysis
All continuous variables were analyzed after testing the normality using the Shapiro–Wilk test. Continuous variables were expressed as the median and interquartile ranges, or the mean and standard deviation. Categorical variables were indicated as counts or percentages of patients in the group. Mann–Whitney test or two-sample t-test was used to analyse continuous variables, and the Chi-square test or the Fisher’s exact test was used to analyse categorical variables. To analyse the temporal change of CH, we used the Friedmann test by comparing the proportion of patients in different HDSS scores by three time periods (1 month, 3 months, and 12 months). Post-hoc analysis was done through the Bonferroni method. Logistic regression was performed to find risk factors related to CH and recurrence. Age, which was a continuous variable, was transformed to categorical variables with the cut-off of 20 after analyzing its relevance in CH and receiver operating characteristic curve. R package version 4.0.5 was used for statistical analysis, and a p-value of less than 0.05 was defined as statistically significant.
Results
The general outcome of surgery
Of the 231 patients who were enrolled in this study, half of them (52.8%) were male and the median age was 23 years [interquartile range (IQR): 19–28]. The median time of the survey from surgery was 20 months (IQR: 13 -38.5). More than three-quarters of patients (n = 188, 81.4%) had received other treatments before surgery; 34 (14.7%) of them had tried more than three treatment methods. Table 1 shows the preoperative treatments and the main reason for surgery. The most frequent treatment prior to surgery was topical use of aluminium chloride solution (68.0%), followed by herbal medicine (33.8%), botulinum toxin injection (18.2%), oral medication (16.5%), and iontophoresis (10%). Sixteen percent of patients chose surgery due to substantial inconvenience related to their jobs requiring heavy use of hands; for example, a physical therapist, a music performer, or a technician.
Within two weeks of surgery, 82 patients (35.5%) reported CH, 9 (3.9%) patients complained of severe postoperative pain, and 43 (18.6%) experienced dry hands. Most patients were discharged within 1 day after surgery, and there was no Horner syndrome and no major adverse events (Table 2). When patients were asked about their satisfaction regarding to the quality of life after surgery, 94% replied that they were content with surgery; the median satisfaction score was 5 out of 5 (IQR: 4–5) (Fig. 1). The median degree of current perspiration at their axilla or hands was 10% (IQR: 5.0–30.0) when the preoperative degree was considered as 100%.
Compensatory hyperhidrosis
A total of 199 (86.1%) patients had CH after ETS, and among them, 71 (30.7%) experienced severe CH, with HDSS of 3 or more. Figure 2 describes the areas that were frequently affected by CH. In brief, the areas affected by CH were as follows: upper back (24.7%), thigh (14.8%), chest (13.4%), and face (11.1%). In a comparison between patients with and without CH, there were less young patients aged 20 years or under in the CH group. However, there was no long-term difference between those with and without CH with respect to the palmar and/or axillary sweating grade and patients’ satisfaction score for surgery (Table 2 and 3).
After one month of surgery, 23.1% (46/199) of those with CH reported HDSS of 3 or more. The proportion of those with HDSS of 3 or more increased over time; 30.2% (60/199) at around three months, and 31.7% (63/199) at around the 1-year mark. The temporal change was significant between one month and three months, but the difference was not as prevalent between three months and one year. Based on this, we could assume that CH manifests within the first three months after surgery (Table 4 and Fig. 3).
The temporal change of HDSS score in Compensatory Hyperhidrosis (CH); HDSS: Hyperhidrosis disease severity score[14], NA: not available. The proportion of compensatory hyperhidrosis severity using HDSS which measured in three different periods; 1 month, 3 months, and 12 months
The risk factors included patients’ demographic variables (body-mass index, age, gender, height, weight, heart rate), the level of sympathicotomy, concurrent plantar or gustatory hyperhidrosis, and the use of an anti-adhesive agent in surgery. Multivariable analysis with logistic regression revealed that an age of 20 years or more (OR: 2.73 [95% CI 1.27–5.85], P = 0.010) may be a significant risk factor for the occurrence of CH (Table 5).
Recurrence after surgery
A total of 44 (19.0%) patients experienced recurrence of palmar and/or axillary hyperhidrosis. There was no difference between the recurrence and non-recurrence groups with respect to the demographic variables and preoperative characteristics of hyperhidrosis. However, the recurrence group received more clipping than sympathicotomy, and there were fewer patients with R4 and R5 sympathicotomy in terms of the level of surgery (Table 5). The non-recurrence group also had more patients treated with an anti-adhesive agent. There was no difference in the early postoperative outcome, but patient’ long-term satisfaction was lower in the recurrence group (5[IQR 4–5] vs. 3.5[IQR 3–5], P < 0.001). Also, the current degree of palmar and/or axillar sweating was significantly higher in the recurrence group (10[IQR 3–20]% vs 40[IQR 30–70]%, P < 0.001) (Table 2 and 3). Furthermore, multivariable analysis with logistic regression found that anti-adhesive agent (OR: 0.42 [95% CI 0.197 – 0.895], P = 0.025) was the only significant factor in reducing recurrence of hyperhidrosis (Table 5).
Discussion
The present study demonstrated the actual experiences of patients who underwent ETS at our institution. Based on an online survey regarding CH and recurrence, we were able to observe and analyse post-ETS problems of CH and recurrence. First, we were able to review how patients were treated before surgery. In this study population, 18% of patients had no previous treatment, and about half of them (45%) had received multiple prior treatments before ETS. Among preoperative modalities, herbal medicine accounted for 33.8%, representing a unique clinical characteristic of South Korea and neighboring eastern Asian countries. We also found that some patients were looking for surgery primarily due to problems related to their jobs. This is meaningful as it suggests that many hyperhidrosis patients are active members of the working group.
To the best of our knowledge, the potential effect of age on CH has not been investigated in previous studies. Leiderman and colleagues reported better outcomes of sympathicotomy in older patients; however, this was mainly about the improvement in main lesions, not about CH [16]. If age plays a vital role in CH, as we suggested in this study, it could guide patients to have surgery as early as possible. Vasconselos-Castro et al. reported a good surgical outcome in 23 patients under the age of 19 years [17]. Therefore, younger age can be an indication of better outcome in terms of symptom improvement and reduced risk of CH development.
To understand the process of CH, several previous studies attempted to track the pattern or severity of CH through various time periods. Chiou et al. reported that CH occurred at the median time of 8.2 weeks after surgery [18]. Our finding is in agreement with this because the severity of CH did not change after 3 months in this study. However, Bryant et al. described that the frequency of clinically bothersome CH peaked at one year postoperatively [6]. This was not verified in this study due to insufficient data after 1 year; future studies are warranted to further investigate the temporal aspects related to CH. The recurrence of hyperhidrosis after ETS has also been a problem, deterring patients from surgery. The recurrence rate has been reported to vary from 0% to as high as 65% [12,13]. Since an online survey is highly subjective – and thus, based on patients’ judgement, the recurrence rate could be overestimated in this study. Moreover, the subjectivity of the survey is further fuelled by the fact that there is no clear definition of recurrent hyperhidrosis; as such, the recurrence rate reported in this study (19.0%) requires further assessment and confirmation.
To the best of our knowledge, reasons for recurrence include inadequate surgery due to variation in the anatomy of the sympathetic chain, failure of surgical technique, or intense pleural adhesion [1]. The incidence of pleural adhesion was highly reported in patients who had unsuccessful previous sympathetic surgery [19,20,21,22,23,24,25]. In agreement with these assumptions, we discovered that the benefit of using anti-adhesive agents is to prevent recurrence. Possible explanations for recurrent sympathetic activity after surgery are varied and unclear; the development of alternate neuroanatomic pathways, the impact of incomplete surgery, and sympathetic nerve regenerations were suggested [22,23,24]. It is our impression, albeit without specific data support, that adhesive tissues and fibrosis could assist the sympathetic neural tissues in recovering their electric conductions. Though we still do not understand the precise mechanism, improving surgical procedures for long-term outcomes is always meaningful.
Other than the related issues of CH and recurrence, this study has illuminated the benefits of an online survey for the future healthcare. As most hyperhidrosis patients are of the age to be a part of the working group, it would not be easy for them to visit the hospital regularly during normal working hours. The online survey, however, still allowed them to report their experiences and condition to healthcare professionals. Southwick et al. reported the benefits of a patient-initiated online survey for providing meaningful feedback and improving patient care [26]. With the recent shift in the clinical environment due to the COVID-19 pandemic, this type of patient-healthcare interaction – or telemedicine – would increasingly provide convenience to patients, allowing them to be able to share their experiences and conditions more easily. This would also help clinicians to better decipher on how best to strategize in providing healthcare to patients, further improving patient care, especially in the aspects of patients’ quality of life.
The present study has several limitations. First, there is a non-response bias. If there is a significant difference between respondents and non-respondents, it could impact the outcome of this study. However, many studies utilizing online surveys have explained that a low response rate does not necessarily mean non-response bias because non-respondents were quite similar in their substantive responses [27,28,29]. If we add the data from interviews of non-respondents, it will complement the result of this study. Second, this is a retrospective study based on an online survey questionnaire, and as such, there may be recall bias and subjective bias that can affect the responses and analysis. Though we tried to minimize the recall bias by reviewing participants' medical records, it was not sufficient, especially among patients who had surgery before 2019 (n = 79, 34.2%) who did not have systematic data of their hospital visits. Another limitation is that only 32 patients did not have CH, and 44 patients reported recurrence; therefore, some factors may not be well considered.
Despite these limitations, this study provides valuable information that can be helpful in identifying and preventing CH and recurrence after ETS. We concluded that patients aged 20 years or more had a greater risk of developing CH after ETS for palmar and/or axillary hyperhidrosis. In addition, we also found that an application of anti-adhesive agents may serve to prevent recurrence after ETS.
Data availability
The data underlying this article will be shared by the corresponding author on reasonable request.
References
Cerfolio RJ, De Campos JRM, Bryant AS, Connery CP, Miller DL, DeCamp MM et al (2011) The society of thoracic surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg 91:1642–1648. https://doi.org/10.1016/j.athoracsur.2011.01.105
Jung HS, Lee DY, Park JS (2018) Alternative surgical methods in patients with recurrent palmar hyperhidrosis and compensatory hyperhidrosis. Yonsei Med J 59:345–348. https://doi.org/10.3349/ymj.2018.59.2.345
Jeong JY, Park SS, Sim SB, Jo KH, Lee J, Oh S et al (2015) Prediction of compensatory hyperhidrosis with botulinum toxin A and local anesthetic. Clin Auton Res 25:201–205. https://doi.org/10.1007/s10286-015-0288-8
Teivelis MP, Wolosker N, Krutman M, de Campos JRM, Kauffman P, Puech-Leão P (2014) Compensatory hyperhidrosis: results of pharmacologic treatment with oxybutynin. Annals Thoracic Surg 98:1797–802. https://doi.org/10.1016/j.athoracsur.2014.05.087
Chou S-H, Kao E-L, Lin C-C, Chang Y-T, Huang M-F (2006) The importance of classification in sympathetic surgery and a proposed mechanism for compensatory hyperhidrosis: experience with 464 cases. Surg Endosc 20:1749–1753. https://doi.org/10.1007/s00464-005-0829-7
Bryant AS, Cerfolio RJ (2014) Satisfaction and compensatory hyperhidrosis rates 5 years and longer after video-assisted thoracoscopic sympathotomy for hyperhidrosis. J Thorac Cardiovasc Surg 147:1160-1163.e1. https://doi.org/10.1016/j.jtcvs.2013.12.016
Chen J-P, Chen R-F, Peng A-J, Xu C-H, Li G-Y (2017) Is compensatory hyperhidrosis after thoracic sympathicotomy in palmar hyperhidrosis patients related to the excitability of thoracic sympathetic ganglions? J Thorac Dis 9:3069–75. https://doi.org/10.21037/jtd.2017.08.100
Aydemir B, Imamoglu O, Okay T, Celik M (2015) Sympathicotomy versus sympathicotomy in palmar hyperhidrosis comparing T3 ablation. Thorac Cardiovasc Surg 63:715–719. https://doi.org/10.1055/s-0034-1384666
Miller DL, Bryant AS, Force SD, Miller JI (2009) Effect of sympathicotomy level on the incidence of compensatory hyperhidrosis after sympathicotomy for palmar hyperhidrosis. J Thorac Cardiovasc Surg 138:581–585. https://doi.org/10.1016/j.jtcvs.2009.03.059
Teivelis MP, Varella AY, Wolosker N (2014) Expanded level of sympathicotomy and incidence or severity of compensatory hyperhidrosis. J Thorac Cardiovasc Surg 148:2443–2444. https://doi.org/10.1016/j.jtcvs.2014.08.025
Du X, Zhu X, Wang T, Hu X, Lin P, Teng Y et al (2018) Compensatory hyperhidrosis after different surgeries at the same sympathetic levels: a meta-analysis. Ann Transl Med 6:203. https://doi.org/10.21037/atm.2018.05.24
Gossot D, Galetta D, Pascal A, Debrosse D, Caliandro R, Girard P et al (2003) Long-term results of endoscopic thoracic sympathicotomy for upper limb hyperhidrosis. Ann Thorac Surg 75:1075–1079. https://doi.org/10.1016/s0003-4975(02)04657-x
Yazbek G, Wolosker N, de Campos JRM, Kauffman P, Ishy A, Puech-Leão P (2005) Palmar hyperhidrosis–which is the best level of denervation using video-assisted thoracoscopic sympathicotomy: T2 or T3 ganglion? J Vasc Surg 42:281–285. https://doi.org/10.1016/j.jvs.2005.03.041
Solish N, Bertucci V, Dansereau A, Hong HC-H, Lynde C, Lupin M et al (2007) A comprehensive approach to the recognition, diagnosis, and severity-based treatment of focal hyperhidrosis: recommendations of the Canadian Hyperhidrosis Advisory Committee. Dermatol Surg 33:908–23. https://doi.org/10.1111/j.1524-4725.2007.33192.x
Wade R, Jones-Diette J, Wright K, Layton AM, Woolacott N (2019) Hyperhidrosis quality of life measures: review and patient perspective. J Dermatol Treat 30:303–308. https://doi.org/10.1080/09546634.2018.1506080
Leiderman DBD, de Campos JRM, Kauffman P, Tedde ML, Yazbek G, Teivelis MP et al (2018) The relation between age and outcomes of thoracic sympathicotomy for hyperhidrosis: The older the better. J Thorac Cardiovasc Surg 156:1748–56. https://doi.org/10.1016/j.jtcvs.2018.05.084
Vasconcelos-Castro S, Soares-Oliveira M, Tuna T, Borges-Dias M (2020) Thoracoscopic sympathotomy for palmar hyperhidrosis: How young is too young? J Pediatr Surg 55:2362–2365. https://doi.org/10.1016/j.jpedsurg.2019.11.024
Chiou TSM (2005) Chronological changes of postsympathicotomy compensatory hyperhidrosis and recurrent sweating in patients with palmar hyperhidrosis. J Neurosurg Spine 2:151–154. https://doi.org/10.3171/spi.2005.2.2.0151
Lin TS, Fang HY, Wu CY (2000) Repeat transthoracic endoscopic sympathectomy for palmar and axillary hyperhidrosis. Surg Endosc 14:134–136. https://doi.org/10.1007/s004649900084
Lin TS (2001) Video-assisted thoracoscopic “resympathicotomy” for palmar hyperhidrosis: analysis of 42 cases. Ann Thorac Surg 72:895–898. https://doi.org/10.1016/s0003-4975(01)02852-1
Kim DH, Paik HC, Lee DY (2005) Video assisted thoracoscopic re-sympathetic surgery in the treatment of re-sweating hyperhidrosis. Eur J Cardiothorac Surg 27:741–744. https://doi.org/10.1016/j.ejcts.2005.01.054
Freeman RK, Van Woerkom JM, Vyverberg A, Ascioti AJ (2009) Reoperative endoscopic sympathectomy for persistent or recurrent palmar hyperhidrosis. Ann Thorac Surg 88:412–417. https://doi.org/10.1016/j.athoracsur.2009.03.101
de Campos JRM, Lembrança L, Fukuda JM, Kauffman P, Teivelis MP, Puech-Leão P, Wolosker N (2017) Evaluation of patients who underwent resympathectomy for treatment of primary hyperhidrosis. Interact Cardiovasc Thorac Surg 25:716–719. https://doi.org/10.1093/icvts/ivx235
Licht PB, Clausen A, Ladegaard L (2010) Resympathicotomy. Ann Thorac Surg 89:1087–1090. https://doi.org/10.1016/j.athoracsur.2010.01.005
Gossot D, Galetta D, Pascal A, Debrosse D, Caliandro R, Girard P, Stern J-B, Grunenwald D (2003) Long-term results of endoscopic thoracic sympathectomy for upper limb hyperhidrosis. Ann Thorac Surg 75:1075–1079. https://doi.org/10.1016/s0003-4975(02)04657-x
Southwick FS, Cranley NM, Hallisy JA (2015) A patient-initiated voluntary online survey of adverse medical events: the perspective of 696 injured patients and families. BMJ Qual Saf 24:620. https://doi.org/10.1136/bmjqs-2015-003980
Choung RS, Locke GR, Schleck CD, Ziegenfuss JY, Beebe TJ, Zinsmeister AR et al (2013) A low response rate does not necessarily indicate non-response bias in gastroenterology survey research: a population-based study. J Public Health 21:87–95. https://doi.org/10.1007/s10389-012-0513-z
Holle R, Hochadel M, Reitmeir P, Meisinger C, Wichmann HE, KORA Group (2006) Prolonged recruitment efforts in health surveys: effects on response, costs, and potential bias. Epidemiology 17:639–43. https://doi.org/10.1097/01.ede.0000239731.86975.7f
Keeter S, Miller C, Kohut A, Groves RM, Presser S (2000) Consequences of reducing nonresponse in a national telephone survey. Public Opin Q 64:125–148. https://doi.org/10.1086/317759
Acknowledgements
There is no acknowledgements.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Wongi Woo MD, Bong Jun Kim MD, Du-Young Kang MD, Duk Hwan Moon MD, Sungsoo Lee MD, PhD and Ms. Jongeun Won, BBA have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Woo, W., Kim, B.J., Kang, DY. et al. Patient experience and prognostic factors of compensatory hyperhidrosis and recurrence after endoscopic thoracic sympathicotomy. Surg Endosc 36, 8340–8348 (2022). https://doi.org/10.1007/s00464-022-09284-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09284-w