Abstract
Background
An estimated 8–15% of patients undergoing cholecystectomy have concomitant common bile duct stones. In this 14-year study, we utilize data of patients at a high-volume tertiary care academic center and compare the clinical outcomes of patients undergoing intraoperative cholangiography (IOC) and endoscopic retrograde pancreatography (ERCP).
Methods
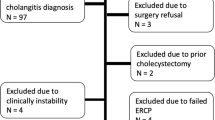
The charts of 1715 patients in the institutional NSQIP database who underwent cholecystectomy between October 1st, 2005 and September 30th, 2019 were retrospectively reviewed. Patients who underwent cholecystectomy in relation to a malignancy diagnosis or who underwent an ERCP in a different index hospitalization were excluded. Main outcomes included hospital length of stay (LOS), post-operative morbidity, and rate of readmissions.
Results
Of the 1409 patients included in the final analysis, 185 patients underwent ERCP, while 95 patients underwent IOC. Use of IOC compared to preoperative ERCP resulted in a shorter LOS (2.6 vs. 5.3 days, p < 0.001), lower rate of readmission (1.1% vs. 6.5%, p = 0.040), and similar rates of post-operative complications. Mean operative time increased by only 15 min in the IOC compared to the ERCP group (129 vs.114 min, p = 0.047). Additional variables that increased LOS on multivariable logistic regression included age, ASA classification, post-operative complications, and increased number of preoperative tests.
Conclusions
This study demonstrates that use of IOC during cholecystectomy results in shorter LOS and fewer readmissions compared to ERCP. Future studies comparing these two approaches should focus on patient randomization, a cost-effectiveness analysis, and identifying barriers to implementation of a one-stage approach in the management of suspected choledocholithiasis.

Similar content being viewed by others
References
Stinton LM, Shaffer EA (2012) Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver 6:172–187
Abboud PA, Malet PF, Berlin JA, Staroscik R, Cabana MD, Clarke JR, Shea JA, Schwartz JS, Williams SV (1996) Predictors of common bile duct stones prior to cholecystectomy: a meta-analysis. Gastrointest Endosc 44:450–455
Nickkholgh A, Soltaniyekta S, Kalbasi H (2006) Routine versus selective intraoperative cholangiography during laparoscopic cholecystectomy: a survey of 2,130 patients undergoing laparoscopic cholecystectomy. Surg Endosc 20:868–874
Guan G, Sun C, Ren Y, Zhao Z, Ning S (2018) Comparing a single-staged laparoscopic cholecystectomy with common bile duct exploration versus a two-staged endoscopic sphincterotomy followed by laparoscopic cholecystectomy. Surgery 164:1030–1034
Zang J, Yuan Y, Zhang C, Gao J (2016) Elective laparoscopic cholecystectomy without intraoperative cholangiography: role of preoperative magnetic resonance cholangiopancreatography - a retrospective cohort study. BMC Surg 16:45
Deytrikh A, Stewart S, Malone N, McTaggart E, Leeder P, Bhatti I, Awan A (2019) Index admission emergency laparoscopic cholecystectomy and common bile duct exploration: results from a specialist center in the United Kingdom. Surg Laparosc Endosc Percutan Tech 29:113–116
Dasari BV, Tan CJ, Gurusamy KS, Martin DJ, Kirk G, McKie L, Diamond T, Taylor MA (2013) Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev CD003327
Gurusamy KS, Giljaca V, Takwoingi Y, Higgie D, Poropat G, Stimac D, Davidson BR (2015) Endoscopic retrograde cholangiopancreatography versus intraoperative cholangiography for diagnosis of common bile duct stones. Cochrane Database Syst Rev CD010339
Sirinek KR, Schwesinger WH (2015) Has intraoperative cholangiography during laparoscopic cholecystectomy become obsolete in the era of preoperative endoscopic retrograde and magnetic resonance cholangiopancreatography? J Am Coll Surg 220:522–528
Program ACoSNSQI (2017) User guide for the 2016 ACS NSQIP procedure targeted participant use data file. ACS
Pan L, Chen M, Ji L, Zheng L, Yan P, Fang J, Zhang B, Cai X (2018) The safety and efficacy of laparoscopic common bile duct exploration combined with cholecystectomy for the management of cholecysto-choledocholithiasis: an up-to-date meta-analysis. Ann Surg 268:247–253
Ricci C, Pagano N, Taffurelli G, Pacilio CA, Migliori M, Bazzoli F, Casadei R, Minni F (2018) Comparison of efficacy and safety of 4 combinations of laparoscopic and intraoperative techniques for management of gallstone disease with biliary duct calculi: a systematic review and network meta-analysis. JAMA Surg 153:e81167
Rojas-Ortega S, Arizpe-Bravo D, Marín López ER, Cesin-Sánchez R, Roman GR, Gómez C (2003) Transcystic common bile duct exploration in the management of patients with choledocholithiasis. J Gastrointest Surg 7:492–496
Lin C, Collins JN, Britt RC, Britt LD (2015) Initial cholecystectomy with cholangiography decreases length of stay compared to preoperative MRCP or ERCP in the management of choledocholithiasis. Am Surg 81:726–731
Chopra I, Wilkins TL, Sambamoorthi U (2016) Hospital length of stay and all-cause 30-day readmissions among high-risk Medicaid beneficiaries. J Hosp Med 11:283–288
Kaboli PJ, Go JT, Hockenberry J, Glasgow JM, Johnson SR, Rosenthal GE, Jones MP, Vaughan-Sarrazin M (2012) Associations between reduced hospital length of stay and 30-day readmission rate and mortality: 14-year experience in 129 Veterans Affairs hospitals. Ann Intern Med 157:837–845
Altieri MS, Yang J, Obeid N, Zhu C, Talamini M, Pryor A (2018) Increasing bile duct injury and decreasing utilization of intraoperative cholangiogram and common bile duct exploration over 14 years: an analysis of outcomes in New York State. Surg Endosc 32:667–674
Jones M, Johnson M, Samourjian E, Schlauch K, Ozobia N (2013) ERCP and laparoscopic cholecystectomy in a combined (one-step) procedure: a random comparison to the standard (two-step) procedure. Surg Endosc 27:1907–1912
Tabone LE, Conlon M, Fernando E, Yi S, Sarker S, Fisichella PM, Luchette FA (2013) A practical cost-effective management strategy for gallstone pancreatitis. Am J Surg 206:472–477
Overman RE Jr, Hsieh LB, Thomas TT, Gadepalli SK, Geiger J (2019) Pediatric laparoscopic common bile duct exploration: an opportunity to decrease ERCP complications. J Surg Res 242:318–322
Wu X, Huang ZJ, Zhong JY, Ran YH, Ma ML, Zhang HW (2019) Laparoscopic common bile duct exploration with primary closure is safe for management of choledocholithiasis in elderly patients. Hepatobiliary Pancreat Dis Int 18:557–561
Mohseni S, Ivarsson J, Ahl R, Dogan S, Saar S, Reinsoo A, Sepp T, Isand KG, Garder E, Kaur I, Ruus H, Talving P (2019) Simultaneous common bile duct clearance and laparoscopic cholecystectomy: experience of a one-stage approach. Eur J Trauma Emerg Surg 45:337–342
Lee HW, Park DH, Lee JH, Oh DW, Song TJ, Lee SS, Seo DW, Lee SK, Kim MH, Moon JE (2019) Prevalence and predictors of unnecessary endoscopic retrograde cholangiopancreatography in the two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy. J Gastrointest Surg 23:1578–1588
Livingston EH, Miller JA, Coan B, Rege RV (2007) Costs and utilization of intraoperative cholangiography. J Gastrointest Surg 11:1162–1167
Acknowledgements
The authors would like to acknowledge Mary Beth Cotter for her assistance in acquiring the data used in this study and whose diligent efforts made this study possible.
Funding
None received for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Savas Tsikis, Sophia H. Yin, Stephen R. Odom, and Nisha Narula have no disclosures or conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsikis, S., Yin, S.H., Odom, S.R. et al. Intraoperative cholangiography: a stepping stone to streamlining the treatment of choledocholithiasis. Surg Endosc 36, 4885–4892 (2022). https://doi.org/10.1007/s00464-021-08840-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08840-0