Abstract
Background
Endoluminal functional lumen imaging probe (EndoFLIP) provides an objective measure of the distensibility index (DI) during different parts of hiatal hernia repair. However, the absolute DI measure above a cut-off after creating a barrier alone has not shown a relationship to dysphagia after surgery. We wanted to determine if the change in DI with volume change is associated with dysphagia.
Methods
We included patients who had hiatal hernia repair with EndoFLIP values, including two values taken at the end of the surgical case with different volumes of fluid in the balloon (30 mL and 40 mL). We compared the absolute and change in DI during hiatal hernia repair and performed an analysis to determine if there was a correlation with short-term clinical outcomes.
Results
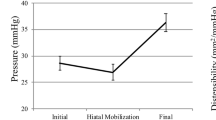
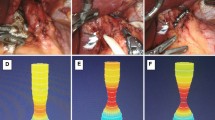
A total of 103 patients met the inclusion and exclusion criteria. Most of the patients underwent Toupet fundoplication (n = 56, 54%), followed by magnetic sphincter augmentation (LINX, n = 28, 27%) and Nissen fundoplication (n = 19, 18%). There was a significant reduction in the DI from the initial DI taken after mobilization of the hiatus (3 mm2/mmHg) and after the creation of the barrier (1.4 mm2/mmHg, p < 0.001). A minority of patients had a decrease or no change in the DI with an increase in balloon volume increased from 30 to 40 mL (n = 37, 36%). Overall, after 1 month, there was a significant decrease in the GERD-HRQL score from 23 to 4 (p < 0.001) and bloat score from 3 to 2 (p = 0.003) with a non-significant decrease in the dysphagia score from 1 to 0 (p = 0.11). Patients who had a decreased or unchanged DI with an increase in the balloon volume from 30 to 40 mL had a significant decrease in their dysphagia score by 2 points (p = 0.04).
Conclusion
The decreased or unchanged DI with an increase in the balloon volume on EndoFLIP is associated with a significant reduction in dysphagia after surgery. The decrease in DI denotes the esophagus’s ability to create higher pressure relative to the change in the cross-sectional area with a larger bolus across the gastroesophageal junction. This measure may be a new marker that can predict short-term outcomes in patients undergoing hiatal hernia repair.



Similar content being viewed by others
References
Jarral OA, Athanasiou T, Hanna GB, Zacharakis E (2012) Is an intra-oesophageal bougie of use during Nissen fundoplication? Interact Cardiovasc Thorac Surg 14:828–833
Huttl TP, Hohle M, Wichmann MW, Jauch KW, Meyer G (2005) Techniques and results of laparoscopic antireflux surgery in Germany. Surg Endosc 19:1579–1587
Kim MP, Meisenbach LM, Chan EY (2018) Tailored fundoplication with endoluminal functional lumen imaging probe allows for successful minimally invasive hiatal hernia repair. Surg Laparosc Endosc Percutan Tech 28:178–182
Tucker E, Sweis R, Anggiansah A, Wong T, Telakis E, Knowles K, Wright J, Fox M (2013) Measurement of esophago-gastric junction cross-sectional area and distensibility by an endolumenal functional lumen imaging probe for the diagnosis of gastro-esophageal reflux disease. Neurogastroenterol Motil 25:904–910
Turner B, Helm M, Hetzel E, Gould JC (2020) Is that “floppy” fundoplication tight enough? Surg Endosc 34:1823–1828
Su B, Dunst C, Gould J, Jobe B, Severson P, Newhams K, Sachs A, Ujiki M (2020) Experience-based expert consensus on the intra-operative usage of the Endoflip impedance planimetry system. Surg Endosc 35:2731–2742
Su B, Callahan ZM, Kuchta K, Linn JG, Haggerty SP, Denham W, Ujiki MB (2020) Use of impedance planimetry (endoflip) in foregut surgery practice: experience of more than 400 cases. J Am Coll Surg 231:160–171
Nwokedi U, Nguyen DT, Meisenbach LM, Chihara R, Chan EY, Graviss EA, Kim MP (2020) Short-term outcome of routine use of EndoFLIP during hiatal hernia repair. Surg Endosc 35(7):3840–3849
Carlson DA (2016) Functional lumen imaging probe: the FLIP side of esophageal disease. Curr Opin Gastroenterol 32:310–318
Lottrup C, Gregersen H, Liao D, Fynne L, Frokjaer JB, Krogh K, Regan J, Kunwald P, McMahon BP (2015) Functional lumen imaging of the gastrointestinal tract. J Gastroenterol 50:1005–1016
Ilczyszyn A, Botha AJ (2014) Feasibility of esophagogastric junction distensibility measurement during Nissen fundoplication. Dis Esophagus 27:637–644
Su B, Attaar M, Wong H, Callahan ZM, Kuchta K, Stearns S, Linn JG, Denham W, Haggerty SP, Ujiki MB (2020) Using a standardized intra-operative endoflip protocol during fundoplication to identify factors that affect distensibility. Surg Endosc 35(10):5717–5723
DeHaan RK, Davila D, Frelich MJ, Gould JC (2017) Esophagogastric junction distensibility is greater following Toupet compared to Nissen fundoplication. Surg Endosc 31:193–198
Turner B, Helm M, Hetzel E, Gould JC (2019) Is that “floppy” fundoplication tight enough? Surg Endosc 34(4):1823–1828
Nathanson LK, Brunott N, Cavallucci D (2012) Adult esophagogastric junction distensibility during general anesthesia assessed with an endoscopic functional luminal imaging probe (EndoFLIP(R)). Surg Endosc 26:1051–1055
Valiati W, Fuchs KH, Valiati L, Freys SM, Fein M, Maroske J, Tigges H, Thiede A (2000) Laparoscopic fundoplication–short- and long-term outcome. Langenbecks Arch Surg 385:324–328
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Min P Kim is a consultant for Veran, Intuitive Surgical, and Medtronic. Edward Chan is a consultant for Veran. Anuj Shah, Duc T. Nguyen, Leonora M. Meisenbach, Ray Chihara, and Edward A. Graviss do not have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shah, A., Nguyen, D.T., Meisenbach, L.M. et al. A novel EndoFLIP marker during hiatal hernia repair is associated with short-term postoperative dysphagia. Surg Endosc 36, 4764–4770 (2022). https://doi.org/10.1007/s00464-021-08817-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08817-z