Abstract
Introduction
Common bile duct stones (CBDS) can spontaneously migrate through the duodenal papilla. In this case, ERCP could be unnecessary and a significant rate of complications could be avoided. In this study, we aim at retrospectively evaluating the rate of spontaneous stone passage in patients with an imaging diagnosis of CBDS and at analysing the factors associated to spontaneous stone migration.
Methods
We conducted a retrospective multi-centre analysis of patients undergoing ERCP for CBDS in a 12-month period. 1016 patients with CBDS were analysed. In all patients CBDS was diagnosed with adequate imaging methods performed prior to ERCP. ERCPs with failed biliary cannulation were excluded. Data regarding patients’ characteristics, imaging findings and ERCP procedure were analysed.
Results
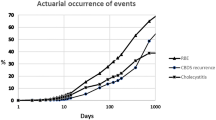
1016 patients with CBDS undergoing ERCP were analysed (male sex 43.3%; mean age 69.9 ± 16.5 years). Diagnosis of CBDS was obtained by EUS in 415 patients (40.8%), MR in 343 (33.8%), CT in 220 (21.7%), and US in 38 (3.7%). No stones were found at ERCP in 179 patients (17.6%), in 14 (6.2%) when ERCP was performed within 6 h from imaging study, in 114 (18.5%) between 7 h and 7 days, in 32 (24.6%) between 8 and 29 days, and in 19 (43.2%) after 30 days. The rate of unnecessary ERCP occurred significantly more frequently in patients in whom imaging methods demonstrated either sludge or ≤ 5 mm CBDS (29.9 vs. 8.3%; p < 0.001).
Discussion
Spontaneous migration of small CBDS is a frequent event, and ≤ 5 mm size and a delay in ERCP > 7 days represent predictive factors for it. We suggest that CBDS ≤ 5 mm should not undergo immediate removal and this fact would allow reducing the rate of unnecessary ERCP with their related complications. Prospective studies are needed to confirm these results and demonstrate the safety of a conservative management in this setting.


Similar content being viewed by others
References
Everhart JE, Khare M, Hill M, Maurer KR (1999) Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology 117:632–639
Shaffer EA (2006) Gallstone disease: epidemiology of gallbladder stone disease. Best Pract Res Clin Gastroenterol 20:981–996
Caddy GR, Tham TC (2006) Gallstone disease: symptoms, diagnosis and endoscopic management of common bile duct stones. Best Pract Res Clin Gastroenterol 20:1085–1101
Johnson KD, Perisetti A, Tharian B, Thandassery R, Jamidar P, Goyal H, Inamdar S (2020) Endoscopic retrograde cholangiopancreatography-related complications and their management strategies: a scoping literature review. Dig Dis Sci 65:361–375
Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P, Barthet M, Domagk D, Dumonceau JM, Gigot JF, Hritz I, Karamanolis G, Laghi A, Mariani A, Paraskeva K, Pohl J, Ponchon T, Swahn F, Ter Steege RWF, Tringali A, Vezakis A, Williams EJ, van Hooft JE (2019) Endoscopic management of common bile duct stones: European society of gastrointestinal endoscopy (ESGE) guideline. Endoscopy 51:472–491
Moller M, Gustafsson U, Rasmussen F, Persson G, Thorell A (2014) Natural course vs interventions to clear common bile duct stones: data from the swedish registry for gallstone surgery and endoscopic retrograde cholangiopancreatography (GallRiks). JAMA Surg 149:1008–1013
Collins C, Maguire D, Ireland A, Fitzgerald E, O’Sullivan GC (2004) A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy: natural history of choledocholithiasis revisited. Ann Surg 239:28–33
Frossard JL, Hadengue A, Amouyal G, Choury A, Marty O, Giostra E, Sivignon F, Sosa L, Amouyal P (2000) Choledocholithiasis: a prospective study of spontaneous common bile duct stone migration. Gastrointest Endosc 51:175–179
Cotton PB (2015) Adverse events: definitions, avoidance, and management ERCP: The Fundamentals. Wiley-Blackwell, New York, pp 369–396
Dumonceau JM, Kapral C, Aabakken L, Papanikolaou IS, Tringali A, Vanbiervliet G, Beyna T, Dinis-Ribeiro M, Hritz I, Mariani A, Paspatis G, Radaelli F, Lakhtakia S, Veitch AM, van Hooft JE (2020) ERCP-related adverse events: European society of gastrointestinal endoscopy (ESGE) guideline. Endoscopy 52:127–149
Chathadi KV, Chandrasekhara V, Acosta RD, Decker GA, Early DS, Eloubeidi MA, Evans JA, Faulx AL, Fanelli RD, Fisher DA, Foley K, Fonkalsrud L, Hwang JH, Jue TL, Khashab MA, Lightdale JR, Muthusamy VR, Pasha SF, Saltzman JR, Sharaf R, Shaukat A, Shergill AK, Wang A, Cash BD, DeWitt JM (2015) The role of ERCP in benign diseases of the biliary tract. Gastrointest Endosc 81:795–880
Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, Bjorkman DJ, Overby CS, Aas J, Ryan ME, Bochna GS, Shaw MJ, Snady HW, Erickson RV, Moore JP, Roel JP (2001) Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc 54:425–434
Ammori BJ, Birbas K, Davides D, Vezakis A, Larvin M, McMahon MJ (2000) Routine vs “on demand” postoperative ERCP for small bile duct calculi detected at intraoperative cholangiography. Clinical evaluation and cost analysis. Surg Endosc 14:1123–1126
Gurusamy KS, Giljaca V, Takwoingi Y, Higgie D, Poropat G, Stimac D, Davidson BR (2015) Ultrasound versus liver function tests for diagnosis of common bile duct stones. Cochrane Database System Rev. https://doi.org/10.1002/14651858.CD011548
Anderson SW, Rho E, Soto JA (2008) Detection of biliary duct narrowing and choledocholithiasis: accuracy of portal venous phase multidetector CT. Radiology 247:418–427
Acknowledgements
Guarantor of the article: Gianpiero Manes. Specific author contributions: Paolo Andreozzi and Gianpiero Manes: Statistical analysis and drafting of the manuscript; Germana de Nucci, Massimo Devani, Davide Redaelli, Mario Schettino, Donato Iuliano, Claudio Zulli, Attilio Maurano, Maria Erminia Bottiglieri, Gregorios Paspatis, Marco Dinelli: data collection. All authors approved the final draft of this manuscript for submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Paolo Andreozzi, Germana de Nucci, Massimo Devani, Davide Redaelli, Mario Schettino, Donato Iuliano, Claudio Zulli, Attilio Maurano, Maria Erminia Bottiglieri, Gregorios Paspatis, Marco Dinelli, Gianpiero Manes have no conflict of interest or fnancial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Andreozzi, P., de Nucci, G., Devani, M. et al. The high rate of spontaneous migration of small size common bile duct stones may allow a significant reduction in unnecessary ERCP and related complications: results of a retrospective, multicenter study. Surg Endosc 36, 3542–3548 (2022). https://doi.org/10.1007/s00464-021-08676-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08676-8