Abstract
Background
Manometry is the gold standard diagnostic test for achalasia. However, there are incidences where manometry cannot be obtained preoperatively, or the results of manometry is inconsistent with the patient's symptomatology. We aim to determine if intraoperative use of EndoFLIP can provide a diagnosis of achalasia and provide objective information during Heller myotomy and Dor fundoplication.
Methods
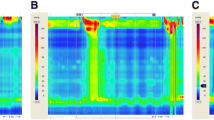
To determine the intraoperative diagnostic EndoFLIP values for patients with achalasia, we determined the optimal cut-off points of the distensibility index (DI) between patients with a diagnosis of achalasia and patients with a diagnosis of hiatal hernia. To evaluate the usefulness of EndoFLIP values during Heller myotomy and Dor fundoplication, we obtained a cohort of patients with EndoFLIP values obtained after Heller myotomy and after Dor fundoplication as well as Eckardt score before and after surgery.
Results
Our analysis of 169 patients (133 hiatal hernia and 36 achalasia) showed that patients with DI < 0.8 have a >99% probability of having achalasia, while DI > 2.3 have a >99% probability of having hiatal hernia. Patients with a DI 0.8–1.3 have a 95% probability of having achalasia, and patients with a DI of 1.4–2.2 have a 94% probability of having a hiatal hernia. There were 40 patients in the cohort to determine objective data during Heller myotomy and Dor fundoplication. The DI increased from a median of 0.7 to 3.2 after myotomy and decreased to 2.2 after Dor fundoplication (p < 0.001). The median Eckardt score went down from a median of 4.5 to 0 (p < 0.001).
Conclusions
Our study shows that intraoperative use of EndoFLIP can facilitate the diagnosis of achalasia and is used as an adjunct to diagnose achalasia when symptoms are inconsistent. The routine use of EndoFLIP during Heller myotomy and Dor fundoplication provides objective data during the operation in a group of patients with excellent short-term outcomes.





Similar content being viewed by others
References
Boeckxstaens GE, Zaninotto G, Richter JE (2014) Achalasia Lancet 383:83–93
Beck WC, Sharp KW (2011) Achalasia. Surg Clin North Am 91:1031–1037
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE, International High Resolution Manometry Working G (2015) The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27:160–174
Muller M (2015) Impact of high-resolution manometry on achalasia diagnosis and treatment. Ann Gastroenterol 28:3–9
Roman S, Kahrilas PJ, Kia L, Luger D, Soper N, Pandolfino JE (2012) Effects of large hiatal hernias on esophageal peristalsis. Arch Surg 147:352–357
Pandolfino JE, Kwiatek MA, Ho K, Scherer JR, Kahrilas PJ (2010) Unique features of esophagogastric junction pressure topography in hiatus hernia patients with dysphagia. Surgery 147:57–64
Desprez C, Roman S, Leroi AM, Gourcerol G (2020) The use of impedance planimetry (Endoscopic Functional Lumen Imaging Probe, EndoFLIP((R)) ) in the gastrointestinal tract: a systematic review. Neurogastroenterol Motil 32:e13980
Su B, Callahan ZM, Novak S, Kuchta K, Ujiki MB (2020) Using impedance planimetry (EndoFLIP) to evaluate myotomy and predict outcomes after surgery for achalasia. J Gastrointest Surg 24:964–971
Carlson DA, Gyawali CP, Kahrilas PJ, Triggs JR, Falmagne S, Prescott J, Dorian E, Kou W, Lin Z, Pandolfino JE (2019) Esophageal motility classification can be established at the time of endoscopy: a study evaluating real-time functional luminal imaging probe panometry. Gastrointest Endosc 90(915–923):e911
Kim MP, Meisenbach LM, Chan EY (2018) Tailored fundoplication with endoluminal functional lumen imaging probe allows for successful minimally invasive hiatal hernia repair. Surg Laparosc Endosc Percutan Tech 28:178–182
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3:32–35
Carlson DA, Pandolfino JE (2013) High-resolution manometry and esophageal pressure topography: filling the gaps of convention manometry. Gastroenterol Clin North Am 42:1–15
Roman S, Kahrilas PJ, Boris L, Bidari K, Luger D, Pandolfino JE (2011) High-resolution manometry studies are frequently imperfect but usually still interpretable. Clin Gastroenterol Hepatol 9:1050–1055
Pandolfino JE, de Ruigh A, Nicodeme F, Xiao Y, Boris L, Kahrilas PJ (2013) Distensibility of the esophagogastric junction assessed with the functional lumen imaging probe (FLIP) in achalasia patients. Neurogastroenterol Motil 25:496–501
Carlson DA, Lin Z, Kahrilas PJ, Sternbach J, Donnan EN, Friesen L, Listernick Z, Mogni B, Pandolfino JE (2015) The functional lumen imaging probe detects esophageal contractility not observed with manometry in patients with achalasia. Gastroenterology 149:1742–1751
Ata-Lawenko RM, Lee YY (2017) Emerging Roles of the endolumenal functional lumen imaging probe in gastrointestinal motility disorders. J Neurogastroenterol Motil 23:164–170
Nwokedi U, Nguyen DT, Meisenbach LM, Chihara R, Chan EY, Graviss EA, Kim MP (2020) Short-term outcome of routine use of EndoFLIP during hiatal hernia repair. Surg Endosc. https://doi.org/10.1007/s00464-020-07788-x
Rohof WO, Hirsch DP, Kessing BF, Boeckxstaens GE (2012) Efficacy of treatment for patients with achalasia depends on the distensibility of the esophagogastric junction. Gastroenterology 143:328–335
Swanstrom LL, Kurian A, Dunst CM, Sharata A, Bhayani N, Rieder E (2012) Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg 256:659–667
Khajanchee YS, Kanneganti S, Leatherwood AE, Hansen PD, Swanstrom LL (2005) Laparoscopic Heller myotomy with Toupet fundoplication: outcomes predictors in 121 consecutive patients. Arch Surg 140:827–833 (discussion 833–824)
Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Hirano I, Boris L, Nicodeme F, Lin Z, Hungness ES (2015) Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc 29:522–528
Smeets FG, Masclee AA, Keszthelyi D, Tjwa ET, Conchillo JM (2015) Esophagogastric junction distensibility in the management of achalasia patients: relation to treatment outcome. Neurogastroenterol Motil 27:1495–1503
Teitelbaum EN, Boris L, Arafat FO, Nicodeme F, Lin Z, Kahrilas PJ, Pandolfino JE, Soper NJ, Hungness ES (2013) Comparison of esophagogastric junction distensibility changes during POEM and Heller myotomy using intraoperative FLIP. Surg Endosc 27:4547–4555
Rohof WO, Salvador R, Annese V, des Varannes BS, Chaussade S, Costantini M, Elizalde JI, Gaudric M, Smout AJ, Tack J, Busch OR, Zaninotto G, Boeckxstaens GE (2013) Outcomes of treatment for achalasia depend on manometric subtype. Gastroenterology 144:718–725 (quiz e713–714)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Min P Kim is a consultant for Veran, Intuitive Surgical, and Medtronic. Edward Chan is a consultant for Veran. Yi Ying Law, Duc T. Nguyen, Leonora M. Meisenbach, Ray Chihara, and Edward A. Graviss do not have any conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Law, Y.Y., Nguyen, D.T., Meisenbach, L.M. et al. Intraoperative diagnosis and treatment of Achalasia using EndoFLIP during Heller Myotomy and Dor fundoplication. Surg Endosc 36, 2365–2372 (2022). https://doi.org/10.1007/s00464-021-08517-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08517-8