Abstract
Background
Laparoscopic surgery with natural orifice specimen extraction (La-NOSE) is being performed more frequently for the minimally invasive management of sigmoid and rectal cancer. The objective of this meta-analysis was to compare the clinical and oncological safety and efficacy of La-NOSE versus conventional laparoscopy (CL).
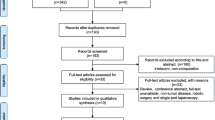
Methods
A search of the PubMed, Web of Science, and Cochrane databases was performed for studies that compared clinical or oncological outcomes of conventional laparoscopic resection using NOSE with conventional laparoscopic resection for sigmoid and rectal cancer.
Results
Compared with CL group, the length of hospital stay and the pain score on the first day were shorter in the La-Nose group. The La-NOSE group had a lower incidence of total perioperative complications (OR 0.46; 95% CI [0.32 to 0.66]; I2 = 0%; P < 0.0001) and a lower incidence of surgical site infections (SSIs) (OR 0.11; 95% CI [0.04 to 0.29]; I2 = 0%; P < 0.0001) than the CL group, while the anastomotic leakage showed no significant difference between the La-Nose group and the CL group (P = 0.19). 5-year disease-free survival (DFS) and 5-year overall survival (OS) were no significant difference between the La-Nose group and the CL group (P = 0.43, P = 0.40, respectively).
Conclusions
La-NOSE can achieve oncological and surgical safety comparable to that of CL for patients with sigmoid and rectal cancer. La-NOSE in patients was associated with a shorter hospital stay, shorter time to first flatus or defecation, less postoperative pain, and fewer surgical site infections (SSIs) and total perioperative complications. In general, the operative time in La-NOSE was longer than that in CL. The long-term oncological efficacy of La-NOSE seems to be equivalent to that of CL.












Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- LA:
-
Conventional laparoscopic surgery
- NOS:
-
Newcastle–Ottawa Scale
- NOSE:
-
Natural orifice specimen extraction
- OR:
-
Odds ratio
- PNT:
-
Prospective non-randomized trial
- RCT:
-
Randomized controlled trial
- RT:
-
Retrospective trial
- SD:
-
Standard deviation
- SSI:
-
Surgery section infection
- MD:
-
Mean difference
References
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics, 2017. CA Cancer J Clin 67:7–30. https://doi.org/10.3322/caac.21387
Jacobs M, Verdeja JC, Goldstein HS (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1:144–150
Simorov A, Shaligram A, Shostrom V et al (2012) Laparoscopic colon resection trends in utilization and rate of conversion to open procedure: a national database review of academic medical centers. Ann Surg 256:462–468. https://doi.org/10.1097/SLA.0b013e3182657ec5
Parker JM, Feldmann TF, Cologne KG (2017) Advances in laparoscopic colorectal surgery. Surg Clin North Am 97:547–560. https://doi.org/10.1016/j.suc.2017.01.005
Martinez-Perez A, Carra MC, Brunetti F et al (2017) Pathologic outcomes of laparoscopic vs open mesorectal excision for rectal cancer: a systematic review and meta-analysis. Jama Surg 152:e165665. https://doi.org/10.1001/jamasurg.2016.5665
Bertelsen CA (2017) Complete mesocolic excision an assessment of feasibility and outcome. Dan Med J 64:B5334
Feinberg AE, Chesney TR, Acuna SA et al (2017) Oncologic outcomes following laparoscopic versus open resection of pT4 colon cancer: a systematic review and meta-analysis. Dis Colon Rectum 60:116–125. https://doi.org/10.1097/DCR.0000000000000641
Winslow ER, Fleshman JW, Birnbaum EH et al (2002) Wound complications of laparoscopic vs open colectomy. Surg Endosc 16:1420–1425. https://doi.org/10.1007/s00464-002-8837-3
Ihedioha U, Mackay G, Leung E et al (2008) Laparoscopic colorectal resection does not reduce incisional hernia rates when compared with open colorectal resection. Surg Endosc 22:689–692. https://doi.org/10.1007/s00464-007-9462-y
Hackert T, Uhl W, Buchler MW (2002) Specimen retrieval in laparoscopic colon surgery. Dig Surg 19:502–506. https://doi.org/10.1159/000067605
Rolanda C, Lima E, Pego JM et al (2007) Third-generation cholecystectomy by natural orifices: transgastric and transvesical combined approach (with video). Gastrointest Endosc 65:111–117. https://doi.org/10.1016/j.gie.2006.07.050
Zorron R, Filgueiras M, Maggioni LC et al (2007) NOTES. Transvaginal cholecystectomy: report of the first case. Surg Innov 14:279–283. https://doi.org/10.1177/1553350607311090
Leroy J, Costantino F, Cahill RA et al (2011) Laparoscopic resection with transanal specimen extraction for sigmoid diverticulitis. Br J Surg 98:1327–1334. https://doi.org/10.1002/bjs.7517
Wolthuis AM, Fieuws S, Van Den Bosch A et al (2015) Randomized clinical trial of laparoscopic colectomy with or without natural-orifice specimen extraction. Br J Surg 102:630–637. https://doi.org/10.1002/bjs.9757
Park JS, Choi GS, Lim KH et al (2010) Clinical outcome of laparoscopic right hemicolectomy with transvaginal resection, anastomosis, and retrieval of specimen. Dis Colon Rectum 53:1473–1479. https://doi.org/10.1007/DCR.0b013e3181f1cc17
Awad Z (2014) Laparoscopic total colectomy with transvaginal extraction of the colon and ileorectal anastomosis. Ann Surg Oncol 21:3029. https://doi.org/10.1245/s10434-014-3678-6
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100. https://doi.org/10.1371/journal.pmed.1000100
Higgins JP, Altman DG, Gotzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605. https://doi.org/10.1007/s10654-010-9491-z
Tierney JF, Stewart LA, Ghersi D et al (2007) Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8:16. https://doi.org/10.1186/1745-6215-8-16
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Kim HJ, Choi G, Park JS et al (2014) Transvaginal specimen extraction versus conventional minilaparotomy after laparoscopic anterior resection for colorectal cancer: mid-term results of a case-matched study. Surg Endosc 28:2342–2348. https://doi.org/10.1007/s00464-014-3466-1
Park JS, Kang H, Park SY et al (2018) Long-term outcomes after Natural Orifice Specimen Extraction versus conventional laparoscopy-assisted surgery for rectal cancer: a matched case-control study. Ann Surg Treat Res 94:26. https://doi.org/10.4174/astr.2018.94.1.26
Hisada M (2014) Complete laparoscopic resection of the rectum using natural orifice specimen extraction. World J Gastroenterol 20:16707. https://doi.org/10.3748/wjg.v20.i44.16707
Ng H, Sun W, Zhao X et al (2018) Outcomes of trans-anal natural orifice specimen extraction combined with laparoscopic anterior resection for sigmoid and rectal carcinoma. Medicine 97:e12347. https://doi.org/10.1097/MD.0000000000012347
Denost Q, Adam J, Pontallier A et al (2015) Laparoscopic total mesorectal excision with coloanal anastomosis for rectal cancer. Ann Surg 261:138–143. https://doi.org/10.1097/SLA.0000000000000855
Xingmao Z, Haitao Z, Jianwei L et al (2014) Totally laparoscopic resection with natural orifice specimen extraction (NOSE) has more advantages comparing with laparoscopic-assisted resection for selected patients with sigmoid colon or rectal cancer. Int J Colorectal Dis 29:1119–1124. https://doi.org/10.1007/s00384-014-1950-7
Liu Z, Efetov S, Guan X et al (2019) A multicenter study evaluating natural orifice specimen extraction surgery for rectal cancer. J Surg Res 243:236–241. https://doi.org/10.1016/j.jss.2019.05.034
Zhou Z, Wang K, Du T et al (2020) Transrectal natural orifice specimen extraction (NOSE) with oncological safety: a prospective and randomized trial. J Surg Res 254:16–22. https://doi.org/10.1016/j.jss.2020.03.064
Zhu Z, Wang K, Orangio GR et al (2020) Clinical efficacy and quality of life after transrectal natural orifice specimen extraction for the treatment of middle and upper rectal cancer. J Gastrointest Oncol 11:260–268. https://doi.org/10.21037/jgo.2020.03.05
Ding Y, Li Z, Gao H et al (2019) Comparison of efficacy between natural orifice specimen extraction without abdominal incision and conventional laparoscopic surgery in the treatment of sigmoid colon cancer and upper rectal cancer. J BUON 24:1817
Hu JH, Li XW, Wang CY et al (2019) Short-term efficacy of natural orifice specimen extraction surgery for low rectal cancer. World J Clin Cases 7:122–129. https://doi.org/10.12998/wjcc.v7.i2.122
Zhou S, Wang X, Zhao C et al (2019) Comparison of short-term and survival outcomes for transanal natural orifice specimen extraction with conventional mini-laparotomy after laparoscopic anterior resection for colorectal cancer. Cancer Manag Res 11:5939–5948. https://doi.org/10.2147/CMAR.S209194
Franklin MJ, Ramos R, Rosenthal D et al (1993) Laparoscopic colonic procedures. World J Surg 17:51–56. https://doi.org/10.1007/BF01655705
Akiyoshi T, Kuroyanagi H, Oya M et al (2009) Short-term outcomes of laparoscopic rectal surgery for primary rectal cancer in elderly patients: is it safe and beneficial? J Gastrointest Surg 13:1614–1618. https://doi.org/10.1007/s11605-009-0961-0
Park JS, Choi GS, Kim HJ et al (2011) Natural orifice specimen extraction versus conventional laparoscopically assisted right hemicolectomy. Br J Surg 98:710–715. https://doi.org/10.1002/bjs.7419
Frye J, Bokey EL, Chapuis PH et al (2009) Anastomotic leakage after resection of colorectal cancer generates prodigious use of hospital resources. Colorectal Dis 11:917–920. https://doi.org/10.1111/j.1463-1318.2008.01728.x
Boccola MA, Lin J, Rozen WM et al (2010) Reducing anastomotic leakage in oncologic colorectal surgery: an evidence-based review. Anticancer Res 30:601–607
Frasson M, Granero-Castro P, Ramos RJ et al (2016) Risk factors for anastomotic leak and postoperative morbidity and mortality after elective right colectomy for cancer: results from a prospective, multicentric study of 1102 patients. Int J Colorectal Dis 31:105–114. https://doi.org/10.1007/s00384-015-2376-6
Nikolian VC, Kamdar NS, Regenbogen SE et al (2017) Anastomotic leak after colorectal resection: a population-based study of risk factors and hospital variation. Surgery 161:1619–1627. https://doi.org/10.1016/j.surg.2016.12.033
Costantino FA, Diana M, Wall J et al (2012) Prospective evaluation of peritoneal fluid contamination following transabdominal vs. transanal specimen extraction in laparoscopic left-sided colorectal resections. Surg Endosc 26:1495–1500. https://doi.org/10.1007/s00464-011-2066-6
Yamamoto S, Inomata M, Katayama H et al (2014) Short-term surgical outcomes from a randomized controlled trial to evaluate laparoscopic and open D3 dissection for stage II/III colon cancer: Japan Clinical Oncology Group Study JCOG 0404. Ann Surg 260:23–30. https://doi.org/10.1097/SLA.0000000000000499
McKenzie S, Baek JH, Wakabayashi M et al (2010) Totally laparoscopic right colectomy with transvaginal specimen extraction: the authors’ initial institutional experience. Surg Endosc 24:2048–2052. https://doi.org/10.1007/s00464-009-0870-z
Asari SA, Cho MS, Kim NK (2015) Safe anastomosis in laparoscopic and robotic low anterior resection for rectal cancer: a narrative review and outcomes study from an expert tertiary center. Eur J Surg Oncol 41:175–185. https://doi.org/10.1016/j.ejso.2014.10.060
Baek SJ, Kim J, Kwak J et al (2013) Can trans-anal reinforcing sutures after double stapling in lower anterior resection reduce the need for a temporary diverting ostomy? World J Gastroenterol 19:5309–5313. https://doi.org/10.3748/wjg.v19.i32.5309
Lamm SH, Zerz A, Efeoglou A et al (2015) Transrectal rigid-hybrid natural orifice translumenal endoscopic sigmoidectomy for diverticular disease: a prospective cohort study. J Am Coll Surg 221:789–797. https://doi.org/10.1016/j.jamcollsurg.2015.07.012
Jayne D, Pigazzi A, Marshall H et al (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318:1569–1580. https://doi.org/10.1001/jama.2017.7219
Kim MJ, Park SC, Park JW et al (2018) Robot-assisted versus laparoscopic surgery for rectal cancer: a phase II open label prospective randomized controlled trial. Ann Surg 267:243–251. https://doi.org/10.1097/SLA.0000000000002321
Baik SH, Ko YT, Kang CM et al (2008) Robotic tumor-specific mesorectal excision of rectal cancer: short-term outcome of a pilot randomized trial. Surg Endosc 22:1601–1608. https://doi.org/10.1007/s00464-008-9752-z
Kuang Y, Lei S, Zhao H et al (2020) Totally robotic distal gastrectomy: a safe and feasible minimally invasive technique for gastric cancer patients who undergo distal gastrectomy. Dig Surg 37:360–367. https://doi.org/10.1159/000507809
Simillis C, Lal N, Thoukididou SN et al (2019) Open versus laparoscopic versus robotic versus transanal mesorectal excision for rectal cancer: a systematic review and network meta-analysis. Ann Surg 270:59–68. https://doi.org/10.1097/SLA.0000000000003227
Vennix S, Pelzers L, Bouvy N et al (2014) Laparoscopic versus open total mesorectal excision for rectal cancer. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD005200.pub3
Liang X, Hou S, Liu H et al (2011) Effectiveness and safety of laparoscopic resection versus open surgery in patients with rectal cancer: a randomized, controlled trial from China. J Laparoendosc Adv Surg Tech A 21:381–385. https://doi.org/10.1089/lap.2010.0059
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Shu Xu, Xi Chen, Kuijie Liu, and Hongliang Yao have no conflicts of interest and financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xu, S., Liu, K., Chen, X. et al. The safety and efficacy of laparoscopic surgery versus laparoscopic NOSE for sigmoid and rectal cancer. Surg Endosc 36, 222–235 (2022). https://doi.org/10.1007/s00464-020-08260-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08260-6