Abstract
Background
Minimally invasive surgery (MIS) has profoundly changed standards of care and lowered perioperative morbidity, but its temporal implementation and factors favoring MIS access remain elusive. We aimed to comprehensibly investigate MIS adoption across different surgical procedures over 20 years, identify predictors for MIS amenability and compare propensity score-matched outcomes among MIS and open surgery.
Methods
Nationwide retrospective analysis of all hospitalizations in Switzerland between 1998 and 2017. Appendectomies (n = 186,929), cholecystectomies (n = 57,788), oncological right (n = 9138) and left hemicolectomies (n = 21,580), rectal resections (n = 13,989) and gastrectomies for carcinoma (n = 6606) were included. Endpoints were assessment of temporal MIS implementation, identification of predictors for MIS access and comparison of propensity score-matched outcomes among MIS and open surgery.
Results
The rates of MIS increased for all procedures during the study period (p ≤ 0.001). While half of all appendectomies were performed laparoscopically by 2005, minimally invasive oncological colorectal resections reached 50% only by 2016. Multivariate analyses identified older age (p ≤ 0.02, except gastrectomy), higher comorbidities (p ≤ 0.001, except rectal resections), lack of private insurance (p ≤ 0.01) as well as rural residence (p ≤ 0.01) with impaired access to MIS. Rural residence correlated with low income regions (p ≤ 0.001), which themselves were associated with decreased MIS access. Geographical mapping confirmed strong disparities for rural and low-income areas in MIS access. Matched outcome analyses revealed benefits of MIS for length of stay, decreased surgical site infection rates for MIS appendectomies and cholecystectomies and higher mortality for open cholecystectomies. No consistent morbidity or mortality benefit for MIS compared to open colorectal resections was observed.
Conclusion
Unequal access to MIS exists in disfavor of older and more comorbid patients and those lacking private insurance, living in rural areas, and having lower income. Efforts should be made to ensure equal MIS access regardless of socioeconomic or geographical factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Implementation of minimally invasive surgery (MIS) has marked a major step forward in the surgical treatment of various diseases over the last decades [1]. Initially used in less demanding operations such as appendectomies or cholecystectomies, MIS has swiftly been adopted to increasingly complex procedures such as oncological colectomies [2], pulmonary lobectomies [3] or gastrectomies [4], providing benefits with respect to return of bowel function, pain, cosmetic results, length of hospital stay (LOS), rates of complications [5] and cost-effectiveness [6].
Regarding oncological outcomes, multiple randomized trials [7,8,9,10,11] and observational studies have shown that laparoscopic approaches for resections of colorectal cancer (CRC) provide equal oncological quality and long-term survival as conventional open surgery (OS). Similar level 1 evidence of equal outcomes were reported for gastrectomies [12,13,14,15], lobectomies [16], distal pancreatectomies [17] and resection of colorectal liver metastases [18]. However, recent studies have also shown shortcomings of MIS in operations such as hysterectomies [19, 20] or pancreaticoduodenectomies [21] with regard to complications and long-term oncological results, although multiple earlier meta-analyses have suggested similar outcomes [22].
While the use of MIS increases steadily [23], United States (US)-based observational studies objectified that major hurdles and inequalities in access to MIS remain. Disparities in choice of surgical access exist based on patient related factors such as ethnicity [24] or insurance status [25, 26] as well as patient-independent factors such as the treating hospital, experience of the surgeon and geographical residential area [27]. In contrast, comprehensive analyses of factors influencing the choice for or against MIS in Europe are currently missing. Furthermore, it remains elusive at which pace MIS approaches were implemented following the published evidence of non-inferior outcomes. While multiple studies reporting on institutional developments of MIS techniques exist, long-term nationwide analyses remain scarce.
Using a national surgical quality control database, we have previously reported that patients in Europe with private insurance have a higher likelihood to receive a MIS colorectal resection [28]. Here, we aimed to investigate the nationwide use and implementation of MIS over a 20-year period across different general surgical procedures. We hypothesized that individual patient access to MIS techniques varies depending on demographic, socioeconomic and geographical factors.
Methods
Study design and data source
The current study is a retrospective observational, nationwide analysis of patients undergoing appendectomies, cholecystectomies and oncological colorectal and gastric resections over 20 years. The Swiss federal statistical office’s (BFS, Neuchatel, Switzerland) databases covering the mandatory, nationwide reporting of all stationary hospitalizations (≥ 24 h) in Swiss hospitals starting from 1998 to 2017 were queried. These databases contain anonymized patient-level data including the main diagnosis responsible for hospitalization and up to 49 secondary diagnoses for comorbidities and complications coded via International Classification of Diseases (ICD-10 German modification) definitions. Procedures are coded by national Swiss surgical classification codes (CHOP), issued annually by the BFS classifying all medical interventions [29].
Data on age (5-year categories), gender, nationality, insurance status are provided as categorial variables. The databases provide place of residence of patients with concomitant anonymity of single cases in 706 subdistrict geographical clusters (MedStat regions) containing one or several official political municipalities [30], with exact information on place of residence (e.g. ZIP codes), location, caseload or case-mix of the treating hospital not available due to anonymization. Each Swiss municipality is classified as urban, suburban or rural [31] and MedStat regions and the included cases were classified accordingly by merging to corresponding municipalities (majority vote in case of differences). Similarly, mean taxable income per municipality in 2015 was queried of the Swiss federal tax administration [32] and averaged on overlapping MedStat regions. For population-adjusted rates of operations, we obtained the total number of inhabitants in Switzerland per year by the BFS [33].
Data processing
The databases were searched for cases of hospitalisations based on the respective main diagnoses acute appendicitis, cholecystitis, colorectal and gastric carcinoma according to the corresponding annual ICD-10 definitions and consequently filtered for the surgical procedures of interest by respective year-matched CHOP codes (Supplementary Tables 1, 2). All codes were specified at study start by consensus of 3 investigators (MS, DG, MT). Minimally invasive or conventional open procedures were distinguished based on codes specifying the surgical approach or codes indicating a laparoscopic access or use of robotic surgical system. Cases were grouped as open, laparoscopic and robotic to assess trends over time. For further analyses, laparoscopic and robotic approaches were combined into MIS cases and compared to OS. For oncological resections, cases were restricted to patients undergoing elective procedures. Readmissions and cases, in which the main reason for surgery was due to a complication, were excluded. Comorbidities & complications were assessed via 49 reported ICD side codes (Supplementary Table 3) and used to assess the extent of comorbidities via the modified version [34] of the Elixhauser score [35].
Outcomes of interest
Primary endpoint was the assessment of implementation of minimally invasive approaches (laparoscopic and robotic) over a 20-year period and identification of predictors for MIS approach. Secondary endpoint was comparison of short-term surgical outcomes of matched OS and MIS cases, including LOS, complications, and in-hospital mortality.
Ethics approval and written consent
As all information in the database are provided completely anonymized by the BFS, no institutional ethics approval or individual patient written consent was required according to the current Swiss Human Research Act.
Statistical analysis
Statistical significance was defined as p < 0.05. Continuous data are given as mean ± standard deviation (SD) or median ± interquartile range (IQR) as appropriate and categorical as number (n) and percentage (%). Students t-test, Wilcoxon’s rank sum test or Fisher’s exact test was used to compare means, medians and proportions or odds among groups. Mann–Kendall Trend Test served to test changes in frequency over time. Correlation between numerical variables was assessed with Pearson’s correlation coefficient. Logistic regression with binary outcome “open” vs. “minimally invasive” procedure served to identify factors influencing the choice of the surgical approach and respective odds with 95% confidence intervals (CI). Propensity score matching was performed using the nearest neighbor method (logistic regression distance, caliper: 0.1) based on year of the operation and identified factors influencing the choice of surgical approach. A 1:1 ratio for interventions with high MIS frequency was used, while allowing up to 5:1 matching for procedures with low MIS frequencies with possible discarding of extreme cases in both groups. Geographical mapping was based on respective MedStat regions of patients by displaying frequencies of MIS approached on publicly available shapefile maps. R version 3.5.1 was used for all database processing, statistical analyses, and graphical representations.
Results
Identification of surgical procedures and developments over time
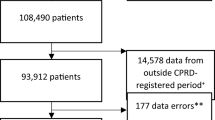
The combined databases comprised 27,121,637 hospitalizations from 1st of January 1998 to 31st of December 2017. Based on respective yearly ICD-10 and surgical codes, 186,929 appendectomies, 57,788 cholecystectomies, 9138 oncological right and 21,580 left hemicolectomies, 13,989 rectal resections and 6606 gastrectomies for carcinoma were identified (Fig. 1). Table 1 summarizes the demographic baseline data of patients per procedure stratified according to OS or MIS, while Table 2 provides data on hospitalization parameters.
Flowchart of patient identification per surgical procedure, depicting the complete dataset, total numbers of identified patients per surgical procedure with stratification of OS and MIS procedures and respective numbers after propensity score matching. OS open surgery, MIS minimally invasive surgery
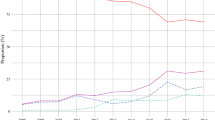
The number of total procedures as well as population-adjusted procedure rates per year increased during 2008–2017 for appendectomies, cholecystectomies, right hemicolectomies, and rectal resections (p < 0.01), while those for left hemicolectomies and gastrectomies remained stable (Fig. 2A). We found different proportions of MIS procedures over the whole 20-year period, ranging from 7.8% for gastrectomies, 19.4% to 26.7% for colorectal resections, 68.5% for appendectomies and 88.1% for cholecystectomies. The rates of MIS increased across all procedures during the study period (p < 0.001), with incremental amounts of robotic procedures observed for all 4 oncological operations. Cholecystectomy was already routinely (> 75%) performed laparoscopically in 1998. While half of all appendectomies were performed laparoscopically by 2005, minimally invasive oncological colorectal resections reached 50% by 2016 and stayed below 20% for gastrectomies in 2017 (Fig. 2B). Next, Elixhauser scores were calculated to assess comorbidities of patients undergoing OS and MIS and compared over groups of 5-year intervals. The degrees of comorbidities increased across all procedures studied, with OS being preferably used in patients with higher Elixhauser scores in all 6 procedures. For cholecystectomies, rates of OS were significantly higher during the entire 20 years in patients with increased comorbidities (Fig. 2C).
Number of operations, implementation of minimally invasive procedures and comorbidities. A Total (brown) and population adjusted (blue) numbers of procedures performed per year from 1998 to 2017. B Representation of percent changes of open (red), laparoscopic (turquois) and robotic (green) surgeries over the 20-year period. C Comorbidities as assessed with Elixhauser score for open (dark red) and minimally invasive (blue) surgeries per procedure in 5-year strata. Single points depict yearly means, diamond & error bars show mean and SD of 5 years. *p < 0.05, **p < 0.01, ***p ≤ 0.001
Predictors of MIS access
Using logistic regression, we explored socioeconomic and demographic factors influencing the choice of surgical access (Fig. 3). The likelihood of receiving a MIS procedure increased greatly over time for all procedures. Patients were 9 × more likely to have a MIS appendectomy during 2008–2012 and 41 × more likely during 2013–2017 compared to 1998–2002. Similarly, odds increased 26 × for right hemicolectomy, 11 × for left hemicolectomy, 16 × for rectal resection and 7 × for gastrectomy between the first and last 5-year strata. For cholecystectomy, the increase was only 4 ×, as already a large proportion of procedures was conducted MIS by the beginning of the study period. Older age predisposed to open surgical procedures across all interventions studied. Indeed, patients in the highest group aged 80–99 years were half as likely to receive a MIS appendectomy and had 4 × lower odds for MIS cholecystectomy (both p ≤ 0.001). Similarly, odds to receive MIS for the oldest group were decreased by 23% for right hemicolectomy (p = 0.02), 48% for left hemicolectomy and 32% for rectal resection (both p ≤ 0.001). Similarly, higher comorbidities predisposed to OS with 28% to > 50% lower odds of receiving MIS (all p ≤ 0.001), except for patients with rectal resections (p = 0.32). For non-oncological operations, female patients were considerably more likely to receive a MIS procedure than their male counterparts. However, this phenomenon was not observed for oncological operations. Patients without Swiss citizenship were more likely to have a MIS appendectomy (p ≤ 0.001), right hemicolectomy (p = 0.003) and rectal resection (p = 0.029), otherwise no clear influence of patients’ nationality was observed. However, patients with private insurance were 22–34% more likely to undergo MIS procedures compared to patients with statutory insurance only (all p ≤ 0.001). Patients living in rural areas had impaired access to MIS for all 6 procedures with a 17% to 40% decreased likelihood compared to patients living in urban and suburban areas.
Odds of factors predicting minimally invasive access per surgical procedure. Graphical representation of logistic regression results regarding choice of MIS vs. OS for all 6 procedures. Blue diamonds indicate logistic odds compared to reference levels with error bars showing 95% CI. *Reference levels. OS open surgery, MIS minimally invasive surgery
Next, we attempted to understand the underlying reason for the consistent impaired MIS access in rural patients. Speculating that differences in prosperity and income of regions contribute to the observed differences, we compared mean taxable incomes per regions of different residential areas. Indeed, 48% of rural areas, but only 13% and 11% of suburban and urban areas respectively, grouped in the lowest quintile of incomes. In contrast, the middle quantile of incomes was made up of 15% of rural, 13% suburban and 31% of urban areas, while the top quintile quantile consisted of 8% rural, 22% suburban and 28% of urban areas (p ≤ 0.001). Geographical mapping according to urban–rural stratification of regions compared with mapping of mean taxable income per region visually confirmed correlation of urban/suburban areas with higher income across most areas of the country (Fig. 4A, B). Additionally, we found that income itself correlated with frequency of MIS in regions (R 0.11–0.13, p ≤ 0.001) for appendectomies, cholecystectomies and colectomies, but not for rectal resection and gastrectomies. Furthermore, for all 6 operations, higher mean income per region correlated strongly with increased frequencies of privately insured patients undergoing the procedure (R 0.22–0.61, all p ≤ 0.001) and all urban and suburban areas had higher frequencies of privately insured patients than rural ones (all p ≤ 0.001).
Geographical mapping of MedStat regions based on urban–rural classification of municipalities, income and frequency of minimally invasive interventions. A Map of Switzerland showing MedStat regions (black boarders) with underlying municipalities (grey boarders) colored according to classification into urban (red), suburban (orange) and rural (green). B Map of Switzerland depicting mean taxable income per MedStat region with color scale of 10%-deciles. C Maps of Switzerland depicting frequencies of minimally invasive interventions for all 6 procedures from 2008 to 2017. Note the visual correlation of areas with higher frequencies with urban and high-income areas and vice versa
Geographical differences of MIS implementation
Based on the observed differences among urban and rural regions in MIS access, frequency of MIS per region was calculated from 2008 to 2017 and consequent geographical mapping performed. Compared with maps displaying urban–rural stratification and mean income per regions, we indeed found strong visual correlation of decreased implementation of MIS procedures in rural and low-income areas (Fig. 4C).
Short-term outcomes of MIS compared to OS
Next, we aimed to identify hospitalisation-related differences among patients undergoing OS vs. MIS. To reliably identify differences owed due to the surgical approach only and not influenced by biasing factors, we propensity score-matched patients undergoing OS or MIS based on the year of operation and identified factors influencing the choice of surgical technique including age, insurance status, comorbidities, urban or rural area and income of region. Matching resulted in groups with attenuated baseline demographic and hospitalization parameters compared to unmatched patients (Supplementary Tables 4, 5) for subsequent analyses of outcomes and complications.
LOS was consistently shorter for all MIS compared to open procedures. With a general short LOS, the observed differences for appendectomies were marginal. In contrast, the effect was most pronounced for patients undergoing cholecystectomy with median LOS of 9–10 days in OS twice the 3–4 days for MIS across the entire 20 years. Patients undergoing MIS hemicolectomies and rectal resections benefitted of a 1–3 days shorter LOS, while MIS gastrectomies reported shortened LOS only in the last period examined (Fig. 5A).
Surgical outcomes of propensity score matched patients. A Boxplots showing length of hospital stay of patients operated open (darkred) and minimally invasive (blue) over 5-year strata for all 6 procedures. Rates of selected complication (B) and in-hospital mortality (C) per intervention for open and minimally invasive procedures. Single points depict yearly means, diamond and error bars show mean and SD of 5 years. *p < 0.05, **p < 0.01, ***p ≤ 0.001
Wound infections were more common in patients undergoing open appendectomy and cholecystectomy, while no clear benefit in this regard was observed for colorectal and gastric resections. Postoperative bleeding was reported more frequently after open cholecystectomy, while inconsistent higher rates were found for MIS colorectal resections. No steady difference was observed for gastrointestinal leakage between MIS and OS for any procedure (Fig. 5B). Readmission rates (recorded in the databases since 2012) were lower following MI appendectomies (2.22 vs. 3.36%, p = 0.001) and cholecystectomies (3.19 vs. 6.25%, p ≤ 0.001). In contrast, slightly higher readmission rates for MI rectal resections were observed (6.18 vs. 4.58%, p = 0.017). No difference was found for right (5.67 vs 4.46%, p = 0.203) and left hemicolectomies (4.24 vs. 3.74%, p = 0.348) or gastrectomies (6.46 vs. 4.42%, p = 0.208). Adjusted in-hospital mortality rates were invariably lower after MIS cholecystectomies, while no relevant differences were observed for appendectomies and all 4 oncological procedures (Fig. 5C).
Discussion
This nationwide study across 6 different surgical procedures revealed 5 consistent key factors decreasing the likelihood to receive MIS: elderly age, increased comorbidities, lack of private insurance, rural residence, and lower income. We found a strong interdependence among rural residence, low income, and decreased rate of private insurance coverage, suggesting that lower socio-economic status hindered MIS access.
Inequalities in access to modern surgical practice like MIS based on socioeconomic and demographic factors should not occur in an ideal healthcare system. However, multiple previous studies have shown higher rates of perioperative complications, decreased MIS amenability and, in case of oncological diseases, impaired long-term survival outcomes for members of certain ethnic groups [36, 37] and under-insured patients [25, 38, 39]. In contrast, the role of residential area and geographical location has just recently come into focus. Recent studies reported impaired access to laparoscopic surgery for diverticular disease and colorectal cancer [40,41,42] as well as modern surgical oncological care for patients living in rural areas in the US [43]. However, little is known how differences in residential areas within other countries influence surgical practice. Our findings of decreased MIS access of patients in rural areas in Switzerland are in accordance with previous reports, point towards a global phenomenon and probably reflect subpar training in oncologic MIS of less-specialized surgeons in remote areas.
The current report provides a comprehensive nationwide temporal analysis of the implementation of MIS over 20 years across different operations, ranging from simple procedures like appendectomy to complex oncological procedures like rectal resections or gastrectomies. As expected, rates of MIS increased across time for all procedures investigated. The data at hand pinpoint several interesting facts. Laparoscopic appendectomy was the first MIS visceral operation performed after the technique was adapted from gynecology [44]. However, laparoscopic cholecystectomy was the first MIS procedure to swiftly gain wide acceptance [45]. Indeed, by 1998, the start of our records, already three quarter of all cholecystectomies were performed laparoscopically. In contrast, implementation of laparoscopic appendectomy was slower, ranging below 25% in 1998 and reaching > 50% only by 2005. MIS implementation in more complex oncological procedures like hemicolectomy or rectal resections was considerably slower, although several large-scale randomized trials started reporting similar oncological short- and later long-term outcomes since 2002 [2, 7,8,9, 11, 45, 46]. Reasons for slow implementation likely include the learning curve for more complex procedures, which might be accentuated in the Swiss decentralized health care system. Switzerland has one of the highest numbers of physicians and hospitals per inhabitants [47], which results in limited caseloads of certain surgical conditions such as resections for colorectal cancer per surgeon and institution. Given that the learning curve for laparoscopic colorectal resections is 30–60 cases [48,49,50], the potential to learn MIS techniques adequately may be limited in rural, low volume hospitals. Furthermore, surgical training in Switzerland includes abdominal general surgery as well as musculoskeletal trauma and many general surgeons in smaller, peripheral Swiss hospitals still perform a broad spectrum of surgical procedures, preventing adequate specialization. Additionally, the implementation of working hour directives and the increased number of surgical residents have resulted in a decreased exposure to colorectal surgery during surgical training, which might furthermore impact on learning of complex MIS techniques [51]. However, centralization with resulting increased caseloads at specialized centers may result in increased MIS amenability for rural and low-income populations in the future. Further reasons might be owed to lack of specific instruments as well as a reluctance of older surgeons to learn new techniques [27], which necessitates the coming in charge of younger surgeons eager to promote modern techniques. Even so, rates observed in our analyses are not vastly different from countries with more pronounced specialization and higher hospital caseloads. In 2004, rates of MIS hemicolectomies for cancer were 4.3% [42], rising to 30–50% in 2009 [41, 52, 53] and 53.5% in 2012 [40] in the US. A recent report has shown US hospitals to be low MIS utilizers for cancer surgery [54] with rates similar to the percentages reported in our present study. Lastly, the lack of implementation of MIS gastrectomy is probably related to the small caseload in Europe, preventing an acceptable learning curve within a meaningful period [55].
We observed that overall degrees of comorbidities increased across all procedures studied, an effect probably dually owed to increased reporting of concomitant diseases in the databases and increasing patient age and comorbidities. Decreased MIS access of older and sicker patients is no novel finding and probably owed to multiple factors like e.g. hesitance to use pneumoperitoneum in patients with severe cardiopulmonary comorbidities or morbid obesity [56]. These results illustrate the paradox associated with MIS: Patients with advanced age and more comorbidities, who would likely benefit the most from the early postoperative advantages of MIS such as reduced pain, facilitated mobilization, faster bowel recovery and reduced hospital stay are more frequently denied MIS for reasons that remain elusive today. Positively, no discrimination in access to MIS based on gender or nationality was found; indeed, rates of MIS in women were higher in appendectomy and cholecystectomy. Furthermore, patients with foreign citizenship benefitted of increased rates of minimally invasive approaches in appendectomy, right hemicolectomies and rectal resections, a finding which might be related to the area of residence. Compared to Swiss citizens, a higher percentage of foreign individuals lives in urban (33.3 ± 1.28% foreign vs. 25.2 ± 1.08%, Swiss) and suburban (46.71 ± 1.94% foreign vs. 43.65 ± 1.18% Swiss) as opposed to rural residential areas (19.96 ± 1.36% foreign vs. 31.26 ± 1.64% Swiss) for all 6 procedures (all p ≤ 0.001). Residence in urban areas might have translated into improved access to specialized centers offering MIS access earlier and more frequently.
Finally, comparison of short-term outcomes using matched patients revealed striking differences in LOS related to the use of MIS. Population-wide benefits with respect to LOS appear larger than expected by results of RCTs, which normally report 1–2 days differences in LOS between open and MIS approaches in colectomy [5]. In our analysis, we found differences in LOS of up to 5 days for cholecystectomies and 3 days for colectomies, rectal resections and gastrectomies. With over 75% of cholecystectomies already being performed MI at the beginning of the study period, the striking difference in LOS of cholecystectomies is probably related to the higher level of comorbidities in patients undergoing open cholecystectomy, reserving OS for difficult cases. Furthermore, the larger than expected differences in LOS in colectomy may reflect disparities typically observed between RCT patient care maps and real-world data derived from observational studies. While some authors suggest that the benefits observed in clinical trials might be even more pronounced if biases are accounted for [57], multiple studies and statistical calculations show that results implied by small scale randomized or observations trials might fail to provide an accurate picture of nationwide developments [58]. Furthermore, LOS observed in our study were longer then reported from large-scale retrospective series from other countries. Switzerland has traditionally longer LOS than other countries in Europe or in the US [28], an aspect which is attributed to regional and cultural traditions rather than medical necessities. Lastly, the observed decrease in LOS across 20 years was modest at best despite major advances in surgical care, changes in hospital reward policies and advent of enhanced recovery after surgery programs [59]. Similarly, rates of readmissions, morbidities and mortality were higher than reported in selected populations of RCTs [5]. The strongly elevated rate of mortality after open cholecystectomy are probably owed to the extent of comorbidities in patients selected for open surgery. Mortality rates of colectomies were several years above 5%, similar to reports published around the change of the millennium [60], and have stagnated around 2% in the last years for left colectomy and rectal resection. Mortality rates after right hemicolectomy were elevated at 3.4%, similar to rates observed for open right hemicolectomy in a recent meta-analysis [61]. It is concerning, that no consistent morbidity and mortality benefits are observed for any colorectal MIS intervention on a national level. All these phenomena might depict a “real-life” effect, representing a median of all patients and not just well-selected patients for participation in a RCT [62].
The databases of all hospitalizations in Switzerland are primarily intended for administrative statistical evaluations by the responsible federal offices and the present study, therefore, has inherent limitations. As it is not a surgical quality control database, no specific information on the interventions itself (duration of surgery, experience of the operating surgeon, R- and N-status) are provided. Similarly, not intended as a cancer-registry, no conclusion on oncological outcomes can be drawn. Furthermore, the database in its current form does not provide information on the influence of center size, caseload, or conversion rates. While we provide absolute numbers for completely performed MIS procedures, we can only speculate how rates of conversion developed over time. However, other groups and we have reported conversion rates e.g. for colectomy [28, 40] and associated risk factors [63]. Lastly, national data of Switzerland might just be partly generalizable to other countries, especially with different healthcare systems. However, despite these limitations, the population-based nature of the databases and its large caseload provides a high level of generalizability and mirrors the actual adoption of MIS over 20 years.
Conclusion
Strong socio-economic, geographic and demographic disparities exist in access to MIS techniques. Considering the observed benefits, efforts should be made to ensure equal MIS availability for patients with elderly age, increased comorbidities, lack of private insurance as well as residence in rural and low-income areas.
Data availability
The national databases covering all stationary hospitalizations is available from the BFS upon signature of a research & data protection agreement for a fee of 712 Swiss francs. All other data used in this study are freely available under the given links. All codes used for filtering, analyses and graphics are available from the first author upon reasonable request.
Abbreviations
- CI:
-
95% Confidence intervals
- IQR:
-
Interquartile range
- LOS:
-
Length of hospital stay
- MIS:
-
Minimally invasive surgery
- OS:
-
Open surgery
- SD:
-
Standard deviation
- CRC:
-
Colorectal cancer
- ICD-10:
-
International Classification of Diseases, German modification
- BFS:
-
Swiss federal statistical office
- CHOP:
-
Swiss surgical classification codes
- MedStat regions:
-
Place of residence with concomitant anonymity of single cases in 706 subdistrict geographical clusters
- n :
-
Number
- %:
-
Percentage
- US:
-
United States
References
Wickham JE (1994) Minimally invasive surgery Future developments. BMJ 308:193–196
Group TLAvOCTS (2007) Laparoscopically assisted vs open colectomy for colon cancer: a meta-analysis. Arch Surg 142:298–303
Cheng X, Onaitis MW, D’Amico TA, Chen H (2018) Minimally invasive thoracic surgery 3.0: lessons learned from the history of lung cancer surgery. Ann Surg 267:37–38
Brenkman HJF, Gisbertz SS, Slaman AE, Goense L, Ruurda JP, van Berge Henegouwen MI, van Hillegersberg R (2017) Postoperative outcomes of minimally invasive gastrectomy versus open gastrectomy during the early introduction of minimally invasive gastrectomy in the netherlands: a population-based cohort study. Ann Surg 266:831–838
Lai JH, Law WL (2012) Laparoscopic surgery for colorectal cancer. Br Med Bull 104:61–89
Gehrman J, Angenete E, Björholt I, Lesén E, Haglind E (2019) Cost-effectiveness analysis of laparoscopic and open surgery in routine Swedish care for colorectal cancer. Surg Endosc 34(10):4403–4412
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy AM (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
Colon Cancer Laparoscopic or Open Resection Study Group (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MHGM, de Lange-de Klerk ESM, Lacy AM, Bemelman WA, Andersson J, Angenete E, Rosenberg J, Fuerst A, Haglind E (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol 25:3061–3068
Best LM, Mughal M, Gurusamy KS (2016) Laparoscopic versus open gastrectomy for gastric cancer. Cochrane Database Syst Rev 3:CD011389
Katai H, Mizusawa J, Katayama H, Morita S, Yamada T, Bando E, Ito S, Takagi M, Takagane A, Teshima S, Koeda K, Nunobe S, Yoshikawa T, Terashima M, Sasako M (2020) Survival outcomes after laparoscopy-assisted distal gastrectomy versus open distal gastrectomy with nodal dissection for clinical stage IA or IB gastric cancer (JCOG0912): a multicentre, non-inferiority, phase 3 randomised controlled trial. Lancet Gastroenterol Hepatol 5:142–151
Huscher CG, Mingoli A, Sgarzini G, Sansonetti A, Di Paola M, Recher A, Ponzano C (2005) Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: five-year results of a randomized prospective trial. Ann Surg 241:232–237
Lee H-J, Kim H-H, Han SU, Kim M-C, Hyung WJ, Ryu SW, Cho GS, Kim CY, Yang H-K, Park DJ, Song KY, Lee SI, Ryu SY, Lee J-H, Kim W (2015) Morbidity and mortality after laparoscopy-assisted and open distal gastrectomy for stage I gastric cancer: Results from a multicenter randomized controlled trial (KLASS-01). J Clin Oncol 33:4–4
Yang CJ, Kumar A, Deng JZ, Raman V, Lui NS, D’Amico TA, Berry MF (2019) A national analysis of short-term outcomes and long-term survival following thoracoscopic versus open lobectomy for clinical stage II non-small-cell lung cancer. Ann Surg. https://doi.org/10.1097/SLA.0000000000003231
de Rooij T, van Hilst J, van Santvoort H, Boerma D, van den Boezem P, Daams F, van Dam R, Dejong C, van Duyn E, Dijkgraaf M, van Eijck C, Festen S, Gerhards M, Groot Koerkamp B, de Hingh I, Kazemier G, Klaase J, de Kleine R, van Laarhoven C, Luyer M, Patijn G, Steenvoorde P, Suker M, Abu Hilal M, Busch O, Besselink M (2019) Minimally invasive versus open distal pancreatectomy (LEOPARD): a multicenter patient-blinded randomized controlled trial. Ann Surg 269:2–9
Fretland AA, Dagenborg VJ, Bjornelv GMW, Kazaryan AM, Kristiansen R, Fagerland MW, Hausken J, Tonnessen TI, Abildgaard A, Barkhatov L, Yaqub S, Rosok BI, Bjornbeth BA, Andersen MH, Flatmark K, Aas E, Edwin B (2018) Laparoscopic versus open resection for colorectal liver metastases: The OSLO-COMET Randomized Controlled Trial. Ann Surg 267:199–207
Melamed A, Margul DJ, Chen L, Keating NL, del Carmen MG, Yang J, Seagle B-LL, Alexander A, Barber EL, Rice LW, Wright JD, Kocherginsky M, Shahabi S, Rauh-Hain JA (2018) Survival after minimally invasive radical hysterectomy for early-stage cervical cancer. N Engl J Med 379:1905–1914
Ramirez PT, Frumovitz M, Pareja R, Lopez A, Vieira M, Ribeiro R, Buda A, Yan X, Shuzhong Y, Chetty N, Isla D, Tamura M, Zhu T, Robledo KP, Gebski V, Asher R, Behan V, Nicklin JL, Coleman RL, Obermair A (2018) Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med 379:1895–1904
van Hilst J, de Rooij T, Bosscha K, Brinkman DJ, van Dieren S, Dijkgraaf MG, Gerhards MF, de Hingh IH, Karsten TM, Lips DJ, Luyer MD, Busch OR, Festen S, Besselink MG, Van Hilst J, De Rooij T, Bosscha K, Brinkman DJ, Van Dieren S, Dijkgraaf MG, Gerhards MF, De Hingh IH, Karsten TM, Lips DJ, Luyer MD, Busch OR, Festen S, Besselink MG, Marsman HA, Van Gulik TM, Wicherts DA, Eshuis WJ, Stibbe LA, Nieveen van Dijkum EJM, Van Hooft JE, Fockens P, Van Laarhoven HW, Wilmink JW, Van de Vijver MJ, Bijlsma MF, Verheij J, Nio CY, Van Lienden KP, Van Tienhoven G, Schoorlemmer A, Creemers G-J, Van Eijck CHJ, Groot Koerkamp B, Bruno MJ, Eskens F, Nuyttens JJ, Pek C, Van der Schelling GP, Seerden TC, Patijn GA, Nieuwenhuijs VB, De Groot JW, Bonsing BA, Vahrmeijer A, Swijnenburg RJ, Mieog JSD, Van der Harst E, Den Dulk M, Olde Damink S, Dejong CHC, Van Dam R, De Vos JM, Liem MSL, Van Laarhoven CJHM, Van Goor H, Van den Boezem PB, Van der Kolk BM, Stommel MWJ, Hermans JJ, Van Geenen EJM, Radema SA, Brosens LA, Scheepers JJG, Roos D, Boerma D, Te Riele W, Van Santvoort HC, Bollen TL, Wit F, Molenaar IQ, Haj Mohammad N, Van Leeuwen MS, Roele A, De Jong KP, De Meijer VE, Klaase JM, Kazemier G, Zonderhuis B, Daams F, Meijerink MR, Latenstein A, Van Rijssen LB, Nota C, Van Halsema E, Van Veldhuisen E, Vogel J, Janssen K, Scholten L, Daamen L, Walma M, Strijker M, Prins M, Zwart M, Suker M, Rombouts S, Mungroop T, Vissers F, Korrel M (2019) Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol 4:199–207
van Hilst J, de Rooij T, Klompmaker S, Rawashdeh M, Aleotti F, Al-Sarireh B, Alseidi A, Ateeb Z, Balzano G, Berrevoet F, Bjornsson B, Boggi U, Busch OR, Butturini G, Casadei R, Del Chiaro M, Chikhladze S, Cipriani F, van Dam R, Damoli I, van Dieren S, Dokmak S, Edwin B, van Eijck C, Fabre JM, Falconi M, Farges O, Fernandez-Cruz L, Forgione A, Frigerio I, Fuks D, Gavazzi F, Gayet B, Giardino A, Groot Koerkamp B, Hackert T, Hassenpflug M, Kabir I, Keck T, Khatkov I, Kusar M, Lombardo C, Marchegiani G, Marshall R, Menon KV, Montorsi M, Orville M, de Pastena M, Pietrabissa A, Poves I, Primrose J, Pugliese R, Ricci C, Roberts K, Rosok B, Sahakyan MA, Sanchez-Cabus S, Sandstrom P, Scovel L, Solaini L, Soonawalla Z, Souche FR, Sutcliffe RP, Tiberio GA, Tomazic A, Troisi R, Wellner U, White S, Wittel UA, Zerbi A, Bassi C, Besselink MG, Abu Hilal M (2019) Minimally invasive versus open distal pancreatectomy for ductal adenocarcinoma (DIPLOMA): a Pan-European Propensity Score Matched Study. Ann Surg 269:10–17
Davis CH, Shirkey BA, Moore LW, Gaglani T, Du XL, Bailey HR, Cusick MV (2018) Trends in laparoscopic colorectal surgery over time from 2005–2014 using the NSQIP database. J Surg Res 223:16–21
Guller U, Jain N, Curtis LH, Oertli D, Heberer M, Pietrobon R (2004) Insurance status and race represent independent predictors of undergoing laparoscopic surgery for appendicitis: secondary data analysis of 145,546 patients. J Am Coll Surg 199:567–575
Billmann F, Langan E (2018) Insurance status, not race, is associated with use of minimally invasive surgical approach for rectal cancer. Ann Surg 268:e49
Turner M, Adam MA, Sun Z, Kim J, Ezekian B, Yerokun B, Mantyh C, Migaly J (2017) Insurance status, not race, is associated with use of minimally invasive surgical approach for rectal cancer. Ann Surg 265:774–781
Aquina CT, Becerra AZ, Justiniano CF, Xu Z, Boscoe FP, Schymura MJ, Noyes K, Monson JRT, Temple LK, Fleming FJ (2019) Surgeon, hospital, and geographic variation in minimally invasive colectomy. Ann Surg 269:1109–1116
Schneider MA, Rickenbacher A, Frick L, Cabalzar-Wondberg D, Käser S, Clavien P-A, Turina M (2018) Insurance status does not affect short-term outcomes after oncological colorectal surgery in Europe, but influences the use of minimally invasive techniques: a propensity score-matched analysis. Langenbecks Arch Surg 403:863–872
Statistik Bf (2020) Swiss surgical classification codes (CHOP).https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/nomenklaturen/medkk.html
Statistik Bf (2020) MedStat Regionen. https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/nomenklaturen/medsreg.html
Statistik Bf (2020) Raumgliederung der Schweiz. https://www.bfs.admin.ch/bfs/de/home/grundlagen/raumgliederungen.html
Steuerverwaltung E (2015) Äquivalenzeinkommen natürliche Personen 2015. https://www.estv.admin.ch/estv/de/home/allgemein/steuerstatistiken/fachinformationen/steuerstatistiken/direkte-bundessteuer.html
Statistik Bf (2020) Ständige Wohnbevölkerung. https://www.bfs.admin.ch/bfs/de/home/statistiken/bevoelkerung/stand-entwicklung/bevoelkerung.html
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ (2009) A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care 47:626–633
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36:8–27
Lidor AO, Gearhart SL, Wu AW, Chang DC (2008) Effect of race and insurance status on presentation, treatment, and mortality in patients undergoing surgery for diverticulitis. Arch Surg 143:1160–1165
Chu DI, Moreira DM, Gerber L, Presti JC, Aronson WJ, Terris MK, Kane CJ, Amling CL, Freedland SJ (2012) Effect of race and socioeconomic status on surgical margins and biochemical outcomes in an equal-access health care setting: results from the Shared Equal Access Regional Cancer Hospital (SEARCH) database. Cancer 118:4999–5007
LaPar DJ, Bhamidipati CM, Mery CM, Stukenborg GJ, Jones DR, Schirmer BD, Kron IL, Ailawadi G (2010) Primary payer status affects mortality for major surgical operations. Ann Surg 252:544–550
Kelz RR, Gimotty PA, Polsky D, Norman S, Fraker D, DeMichele A (2004) Morbidity and mortality of colorectal carcinoma surgery differs by insurance status. Cancer 101:2187–2194
Moghadamyeghaneh Z, Carmichael JC, Mills S, Pigazzi A, Nguyen NT, Stamos MJ (2015) Variations in laparoscopic colectomy utilization in the United States. Dis Colon Rectum 58:950–956
Fox J, Gross CP, Longo W, Reddy V (2012) Laparoscopic colectomy for the treatment of cancer has been widely adopted in the United States. Dis Colon Rectum 55:501–508
Kemp JA, Finlayson SRG (2008) Nationwide trends in laparoscopic colectomy from 2000 to 2004. Surg Endosc 22:1181–1187
Hung P, Deng S, Zahnd WE, Adams SA, Olatosi B, Crouch EL, Eberth JM (2020) Geographic disparities in residential proximity to colorectal and cervical cancer care providers. Cancer 126:1068–1076
Litynski GS (1998) Kurt Semm and the fight against skepticism: endoscopic hemostasis, laparoscopic appendectomy, and Semm’s impact on the “laparoscopic revolution.” JSLS 2:309–313
Darzi SA, Munz Y (2004) The impact of minimally invasive surgical techniques. Annu Rev Med 55:223–237
Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359:2224–2229
Organization WH (2020) World Health Statistics 2019: Monitoring health for the SDGs. 2019.
Kayano H, Okuda J, Tanaka K, Kondo K, Tanigawa N (2011) Evaluation of the learning curve in laparoscopic low anterior resection for rectal cancer. Surg Endosc 25:2972–2979
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242:83–91
Wishner JD, Baker JW Jr, Hoffman GC, Hubbard GW 2nd, Gould RJ, Wohlgemuth SD, Ruffin WK, Melick CF (1995) Laparoscopic-assisted colectomy. The learning curve. Surg Endosc 9:1179–1183
Käser SA, Rickenbacher A, Cabalzar-Wondberg D, Schneider M, Dietrich D, Misselwitz B, Clavien P-A, Turina M (2019) The growing discrepancy between resident training in colonic surgery and the rising number of general surgery graduates. Int J Colorectal Dis 34:423–429
Alnasser M, Schneider EB, Gearhart SL, Wick EC, Fang SH, Haider AH, Efron JE (2014) National disparities in laparoscopic colorectal procedures for colon cancer. Surg Endosc 28:49–57
Simorov A, Shaligram A, Shostrom V, Boilesen E, Thompson J, Oleynikov D (2012) Laparoscopic colon resection trends in utilization and rate of conversion to open procedure: a national database review of academic medical centers. Ann Surg 256:462–468
Mason MC, Tran Cao HS, Awad SS, Farjah F, Chang GJ, Massarweh NN (2018) Hospital minimally invasive surgery utilization for gastrointestinal cancer. Ann Surg 268:303–310
Jung DH, Son SY, Park YS, Shin DJ, Ahn HS, Ahn SH, Park DJ, Kim HH (2016) The learning curve associated with laparoscopic total gastrectomy. Gastric Cancer 19:264–272
Lascano CA, Kaidar-Person O, Szomstein S, Rosenthal R, Wexner SD (2006) Challenges of laparoscopic colectomy in the obese patient: a review. Am J Surg 192:357–365
Faucheron JL, Sage PY, Trilling B (2018) Open, laparoscopic, or robotic rectal cancer surgery: adjustments for biases may increase the differences. Ann Surg 268:e50–e51
Dickerman BA, García-Albéniz X, Logan RW, Denaxas S, Hernán MA (2019) Avoidable flaws in observational analyses: an application to statins and cancer. Nat Med 25:1601–1606
Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, Francis N, McNaught CE, Macfie J, Liberman AS, Soop M, Hill A, Kennedy RH, Lobo DN, Fearon K, Ljungqvist O, Enhanced Recovery After Surgery Society fPC, Nutrition ESfC, Metabolism, Metabolism IAfS, Nutrition (2013) Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations. World J Surg 37:259–284
Longo WE, Virgo KS, Johnson FE, Oprian CA, Vernava AM, Wade TP, Phelan MA, Henderson WG, Daley J, Khuri SF (2000) Risk factors for morbidity and mortality after colectomy for colon cancer. Dis Colon Rectum 43:83–91
Arezzo A, Passera R, Ferri V, Gonella F, Cirocchi R, Morino M (2015) Laparoscopic right colectomy reduces short-term mortality and morbidity. Results of a systematic review and meta-analysis. Int J Colorectal Dis 30:1457–1472
Allaix ME, Rebecchi F, Fichera A (2020) The landmark series: minimally invasive (laparoscopic and robotic) colorectal cancer surgery. Ann Surg Oncol 27:3704–3715
Crippa J, Grass F, Achilli P, Mathis KL, Kelley SR, Merchea A, Colibaseanu DT, Larson DW (2020) Risk factors for conversion in laparoscopic and robotic rectal cancer surgery. Br J Surg 107:560–566
Funding
Open access funding provided by University of Zurich.
Author information
Authors and Affiliations
Contributions
MT served as the primary investigator of the study. MAS, DG, KH, AR & MT made substantial contributions to the study conception and design. MAS, DG, AR & MT contributed to the acquisition of data. MAS, DG, MM performed statistics, calculations & graphical illustrations. All authors analysed and interpreted the data. MAS & MT wrote the manuscript. All authors contributed to revision of the manuscript and final approval for publication.
Corresponding author
Ethics declarations
Disclosures
This research did not receive any specific grant or funding from agencies in the public, commercial, or non-profit sectors. Marcel Schneider, Daniel Gero, Matteo Müller, Karoline Horisberger, Andreas Rickenbacher and Matthias Turina have no conflicts of interest of financial ties to disclose.
Ethical approval
No institutional ethical approval was required for this study according to the current Swiss Human Research Act.
Informed consent
No individual patient written consent was required as all information in the database are completely anonymized. No trial registration was required for this retrospective series.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schneider, M.A., Gero, D., Müller, M. et al. Inequalities in access to minimally invasive general surgery: a comprehensive nationwide analysis across 20 years. Surg Endosc 35, 6227–6243 (2021). https://doi.org/10.1007/s00464-020-08123-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08123-0