Abstract
Background
Although early series focused on benign disease, minimally invasive pancreatoduodenectomy (MIPD) might be particularly suited for malignancy. Unlike their predecessors, fellowship-trained (FT) Hepatic-Pancreatic and Biliary (HPB) surgeons usually have equal skills in approaching peri-ampullary tumors (PT) either openly or via minimally invasive (MI) techniques.
Method
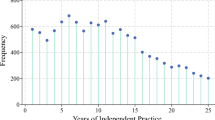
We retrospectively reviewed a MI-HPB-FT surgeon’s 10-year experience with PD. A sub-analysis of malignant PT was also done (MIPD-PT vs. OPD-PT). The primary endpoint was to assess postoperative mortality and morbidity. Secondary endpoints included operative parameters, length of hospital stay, and survival analysis. Moreover, we addressed practice pattern changes for a surgeon straight out of training with no previous experience of independent surgery.
Results
From December 2007-February 2018, one MI-HPB-FT performed a total of 100 PDs, including 57 MIPDs and 43 open PDs (OPDs). In both groups, over 70% of PDs were undertaken for malignancy. Eight patients with borderline resectable pancreatic ductal cancer (PDC) were in the OPD-PT group (as compared to only 2 in the MIPD-PT group) (p = 0.07). Estimated mean blood loss and length of stay were less in the MIPD-PT group (345 mL and 12 days) as compared to the OPD-PT group (971 mL and 16 days), p < 0.001 and p = 0.007, respectively. However, the mean operative time was longer for the MIPD-PT (456 min) as compared to the OPD-PT (371 min), p < 0.001. Thirty and 90-day mortality was 2.6%/5.1% after MIPD-PT compared to 0%/3.2% after OPD-PT, respectively, p = 1. Overall 30-/90-day morbidity rates were similar at 41.0%/43.6% after MIPD-PT and 35.5%/41.9% after OPD-PT, respectively, p = 0.8 and 1. Complete resection (R0) rates were not statistically different, 97.4% after MIPD-PT compared to 87.0% after OPD-PT (p = 0.2). After MIPD and OPD for malignant PT, overall 1, 3 and 5-year survival rates, and median survival were 82.5%, 59.6% and 46.3% and 38 months as compared to 52.5%, 15.7% and 10.5% and 13 months, respectively (p = 0.01). In the MIDP-PT group, recurrence free survival (RFS) at 1, 3 and 5 years and median RFS were 69.1%, 41.9% and 33.5% and 26 months as compared to 50.4%, 6.3% and 6.3% and 13 months, in the OPD-PT group, respectively (p = 0.03).
Conclusion
FT HPB Surgeons who begin their practice with the ability to do both MI and OPD may preferentially approach resectable peri-ampullary tumors minimally invasively. This may result in decreased blood loss decreased length of hospital stays. Despite longer operative time, the improved visualization of MI techniques may enable superior R0 rates when compared to historical open controls. Moreover, combined with quicker initiation of adjuvant chemotherapeutic treatments, this may eventually result in improved survival.



Similar content being viewed by others
References
Abu Hilal M, Takhar AS (2013) Laparoscopic left pancreatectomy: current concepts. Pancreatology 13(4):443–8
van Hilst J et al (2017) Worldwide survey on opinions and use of minimally invasive pancreatic resection. HPB (Oxford) 19(3):190–204
Klompmaker S, et al (2019) International validation of reduced major morbidity after minimally invasive distal pancreatectomy compared with open pancreatectomy. Ann Surg
de Rooij T et al (2019a) Minimally invasive versus open distal pancreatectomy (LEOPARD): a multicenter patient-blinded Randomized Controlled Trial. Ann Surg 269(1):2–9
van Hilst J et al (2019a) Costs and quality of life in a randomized trial comparing minimally invasive and open distal pancreatectomy (LEOPARD trial). Br J Surg 106(7):910–921
de Rooij T et al (2015) Technical aspects of laparoscopic distal pancreatectomy for benign and malignant disease: review of the literature. Gastroenterol Res Pract 2015:472906
Palanivelu C et al (2017) Randomized clinical trial of laparoscopic versus open pancreatoduodenectomy for periampullary tumours. Br J Surg 104(11):1443–1450
Poves I et al (2018) Comparison of perioperative outcomes between laparoscopic and open approach for pancreatoduodenectomy: the PADULAP Randomized Controlled Trial. Ann Surg 268(5):731–739
van Hilst J et al (2019b) Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol 4(3):199–207
Gagner M, Pomp A (1994) Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 8(5):408–410
Palanivelu C et al (2007) Laparoscopic pancreaticoduodenectomy: technique and outcomes. J Am Coll Surg 205(2):222–230
Gumbs AA, Gayet B (2008) The laparoscopic duodenopancreatectomy: the posterior approach. Surg Endosc 22(2):539–540
Asbun HJ, Stauffer JA (2012) Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the Accordion Severity Grading System. J Am Coll Surg 215(6):810–819
Gumbs AA et al (2013) 200 consecutive laparoscopic pancreatic resections performed with a robotically controlled laparoscope holder. Surg Endosc 27(10):3781–3791
Croome, K.P., et al., Total laparoscopic pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: oncologic advantages over open approaches? Ann Surg, 2014. 260(4): p. 633–8; discussion 638–40.
Kendrick ML et al (2017) Minimally invasive pancreatoduodenectomy. HPB (Oxford) 19(3):215–224
Pedziwiatr M et al (2017) Minimally invasive versus open pancreatoduodenectomy-systematic review and meta-analysis. Langenbecks Arch Surg 402(5):841–851
de Rooij T et al (2018) Minimally invasive versus open pancreatoduodenectomy (LEOPARD-2): study protocol for a randomized controlled trial. Trials 19(1):1
McCulloch P et al (2009) No surgical innovation without evaluation: the IDEAL recommendations. Lancet 374(9695):1105–1112
Halls MC et al (2019) A comparison of the learning curves of laparoscopic liver surgeons in differing stages of the IDEAL paradigm of surgical innovation: standing on the shoulders of pioneers. Ann Surg 269(2):221–228
Gumbs AA, Gayet B (2007) The medical and surgical department of digestive diseases and minimally invasive HPB Fellowship at IMM. HPB (Oxford) 9(6):470–471
Callery MP et al (2009) Pretreatment assessment of resectable and borderline resectable pancreatic cancer: expert consensus statement. Ann Surg Oncol 16(7):1727–1733
Gumbs AA, Daskalaki D, Milone L (2018) Laparoscopic total pancreatectomy for chronic pancreatitis. Surg Laparosc Endosc Percutan Tech 28(2):e62
Palanivelu C et al (2018) International Summit on laparoscopic pancreatic resection (ISLPR) “Coimbatore Summit Statements.” Surg Oncol 27(1):A10–A15
Trudeau MT et al (2020) Pancreatic head resection following Roux-en-Y Gastric bypass: operative considerations and outcomes. J Gastrointest Surg 24(1):76–87
Gumbs AA, Gayet B, Hoffman JP (2011) Video: laparoscopic Whipple procedure with a two-layered pancreatojejunostomy. Surg Endosc 25(10):3446–3447
Gumbs AA, Rodriguez-Rivera AM, Hoffman JP (2011) Minimally invasive pancreatic surgery of the entire gland: initial experience. Minerva Chir 66(4):269–280
Ogiso S et al (2013) Posterior approach for laparoscopic pancreaticoduodenectomy to prevent replaced hepatic artery injury. Ann Surg Oncol 20(9):3120
Gumbs AA et al (2007) Modified robotic lightweight endoscope (ViKY) validation in vivo in a porcine model. Surg Innov 14(4):261–264
Chun YS, Pawlik TM, Vauthey JN (2018) 8th Edition of the AJCC cancer staging manual: pancreas and hepatobiliary cancers. Ann Surg Oncol 25(4):845–847
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Bassi C et al (2004) Pancreatic fistula rate after pancreatic resection. The importance of definitions. Dig Surg 21(1):54–59
Klaiber U et al (2018) Meta-analysis of delayed gastric emptying after pylorus-preserving versus pylorus-resecting pancreatoduodenectomy. Br J Surg 105(4):339–349
Maggino L et al (2018) Impact of operative time on outcomes after pancreatic resection: a risk-adjusted analysis using the American College of Surgeons NSQIP Database. J Am Coll Surg 226(5):844–857
Dokmak S (2019) Comment on “comparison of perioperative outcomes between the laparoscopic and open approach for pancreaticoduodenectomy: can we compare the results of the laparoscopic approach with bad results of the open approach?” Ann Surg 270(6):e91–e92
Poves I (2019) Response to comment on “comparison of perioperative outcomes between the laparoscopic and open approach for pancreaticoduodenectomy. Can we compare the results of the laparoscopic approach with bad results of the open approach?” Ann Surg 270(6):e92
Cameron JL et al (2006) One thousand consecutive pancreaticoduodenectomies. Ann Surg 244(1):10–15
Cameron JL, He J (2015) Two thousand consecutive pancreaticoduodenectomies. J Am Coll Surg 220(4):530–536
Adam MA et al (2015) Minimally invasive versus open pancreaticoduodenectomy for cancer: practice patterns and short-term outcomes among 7061 patients. Ann Surg 262(2):372–377
Kantor O et al (2017) Laparoscopic pancreaticoduodenectomy for adenocarcinoma provides short-term oncologic outcomes and long-term overall survival rates similar to those for open pancreaticoduodenectomy. Am J Surg 213(3):512–515
Dokmak S et al (2015) Laparoscopic pancreaticoduodenectomy should not be routine for resection of periampullary tumors. J Am Coll Surg 220(5):831–838
Crist DW, Cameron JL (1989) Current status of pancreaticoduodenectomy for periampullary carcinoma. Hepatogastroenterology 36(6):478–485
Yeo CJ et al (1997) Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: pathology, complications, and outcomes. Ann Surg 226(3):248–57 (discussion 257–60)
Balzano G et al (2008) Effect of hospital volume on outcome of pancreaticoduodenectomy in Italy. Br J Surg 95(3):357–362
Gooiker GA et al (2014) Impact of centralization of pancreatic cancer surgery on resection rates and survival. Br J Surg 101(8):1000–1005
Sanchez-Velazquez P et al (2019) Benchmarks in pancreatic surgery: a novel tool for unbiased outcome comparisons. Ann Surg 270(2):211–218
Farges O et al (2017) The theory and practice of pancreatic surgery in France. Ann Surg 266(5):797–804
de Rooij T et al (2019b) Outcomes of a multicenter training program in laparoscopic pancreatoduodenectomy (LAELAPS-2). Ann Surg 269(2):344–350
Chapman BC et al (2018) Comparison of laparoscopic to open pancreaticoduodenectomy in elderly patients with pancreatic adenocarcinoma. Surg Endosc 32(5):2239–2248
Seiler CA et al (2005) Randomized clinical trial of pylorus-preserving duodenopancreatectomy versus classical Whipple resection-long term results. Br J Surg 92(5):547–556
Jang JY et al (2014) A prospective randomized controlled study comparing outcomes of standard resection and extended resection, including dissection of the nerve plexus and various lymph nodes, in patients with pancreatic head cancer. Ann Surg 259(4):656–664
Kunstman JW et al (2019) Outcomes after pancreatectomy with routine pasireotide use. J Am Coll Surg 228(2):161–170
Matsumoto I et al (2014) A prospective randomized comparison between pylorus- and subtotal stomach-preserving pancreatoduodenectomy on postoperative delayed gastric emptying occurrence and long-term nutritional status. J Surg Oncol 109(7):690–696
Young S et al (2018) Pasireotide is not effective in reducing the development of postoperative pancreatic fistula. HPB (Oxford) 20(9):834–840
Allen PJ et al (2014) Pasireotide for postoperative pancreatic fistula. N Engl J Med 370(21):2014–2022
Cai Y, et al (2020) Laparoscopic duodenum-preserving total pancreatic head resection using real-time indocyanine green fluorescence imaging. Surg Endosc
Machado MA et al (2016) Laparoscopic pancreatoduodenectomy in 50 consecutive patients with no mortality: a single-center experience. J Laparoendosc Adv Surg Tech A 26(8):630–634
Conrad C et al (2017) Comparable long-term oncologic outcomes of laparoscopic versus open pancreaticoduodenectomy for adenocarcinoma: a propensity score weighting analysis. Surg Endosc 31(10):3970–3978
Chen XM, Sun DL, Zhang Y (2018) Laparoscopic versus open pancreaticoduodenectomy combined with uncinated process approach: a comparative study evaluating perioperative outcomes (Retrospective cohort study). Int J Surg 51:170–173
Chikhladze S et al (2019) Adjuvant chemotherapy after surgery for pancreatic ductal adenocarcinoma: retrospective real-life data. World J Surg Oncol 17(1):185
Ma SJ et al (2019) Association of timing of adjuvant therapy with survival in patients with resected stage I to II pancreatic cancer. JAMA Netw Open 2(8):e199126
Croome KP et al (2015) Pancreaticoduodenectomy with major vascular resection: a comparison of laparoscopic versus open approaches. J Gastrointest Surg 19(1):189–94 (discussion 194)
Sohn TA et al (2000) Resected adenocarcinoma of the pancreas-616 patients: results, outcomes, and prognostic indicators. J Gastrointest Surg 4(6):567–579
Andrianello S et al (2015) Pancreaticoduodenectomy for distal cholangiocarcinoma: surgical results, prognostic factors, and long-term follow-up. Langenbecks Arch Surg 400(5):623–628
Hsu CP et al (2018) Three-year and five-year outcomes of surgical resection for pancreatic ductal adenocarcinoma: Long-term experiences in one medical center. Asian J Surg 41(2):115–123
He C et al (2018) Nomograms predict long-term survival for patients with periampullary adenocarcinoma after pancreatoduodenectomy. BMC Cancer 18(1):327
Yeo CJ et al (1998) Periampullary adenocarcinoma: analysis of 5-year survivors. Ann Surg 227(6):821–831
van Geenen RC et al (2001) Survival after pancreaticoduodenectomy for periampullary adenocarcinoma: an update. Eur J Surg Oncol 27(6):549–557
Speicher PJ et al (2014) Defining the learning curve for team-based laparoscopic pancreaticoduodenectomy. Ann Surg Oncol 21(12):4014–4019
Wang M et al (2016) Learning curve for laparoscopic pancreaticoduodenectomy: a CUSUM analysis. J Gastrointest Surg 20(5):924–935
Fretland AA et al (2018) Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET Randomized Controlled Trial. Ann Surg 267(2):199–207
Tanaka S et al (2017) Validation of a difficulty scoring system for laparoscopic liver resection: a multicenter analysis by the endoscopic liver surgery study group in Japan. J Am Coll Surg 225(2):249–258
Mogal H et al (2017) Modified Frailty Index predicts morbidity and mortality after pancreaticoduodenectomy. Ann Surg Oncol 24(6):1714–1721
Ohtsuka T et al (2020) A multicenter prospective registration study on laparoscopic pancreatectomy in Japan: report on the assessment of 1,429 patients. J Hepatobiliary Pancreat Sci 27(2):47–55
Asbun HJ et al (2020) The Miami International evidence-based guidelines on minimally invasive pancreas resection. Ann Surg 271(1):1–14
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gumbs, A.A., Chouillard, E., Abu Hilal, M. et al. The experience of the minimally invasive (MI) fellowship-trained (FT) hepatic-pancreatic and biliary (HPB) surgeon: could the outcome of MI pancreatoduodenectomy for peri-ampullary tumors be better than open?. Surg Endosc 35, 5256–5267 (2021). https://doi.org/10.1007/s00464-020-08118-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08118-x