Abstract
Background
Our group has previously demonstrated that low socioeconomic status (SES) independently predicts ≤ 25th percentile weight-loss following bariatric surgery (BS). Given that sociodemographic metrics can be separated into income, education, and race, we sought to investigate how each metric independently impacted weight loss following BS.
Methods
Patients from a single academic institution who underwent bariatric surgery from 2014 to 2016 were retrospectively reviewed. Patients were stratified by income (low/high), education (≤ high school/ ≥ college), and race (black/white) then compared using univariate analysis. Variables significant on univariate analyses were subsequently used for a greedy 1:3 propensity score match with a caliper of 0.2. After matching, groups were balanced on demographics, social/medical/psychological history, and surgery type. Percent excess body weight loss for each post-operative time point was compared using appropriate univariate analyses. A p-value ≤ 0.05 was considered statistically significant.
Results
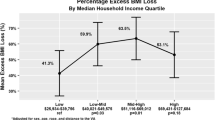
571 patients were included. Unmatched race analysis demonstrated black patients were significantly younger (p = 0.05), single (p < 0.0001), in a lower income bracket (p < 0.0001), and experienced less weight loss at 2- (p = 0.01), 6- (p = 0.007), 12- (p = 0.008) and 24- (p = 0.007) months post-op. After matching, black patients continued to experience less weight loss at 2- (p = 0.01) and 6- (p = 0.03) months, which trended at 1 year (p = 0.06). Initial income analysis demonstrated patients in the low-income group (LIG) were more likely to be black (p < 0.0001), have ≤ high school education (p = 0.004), a higher preoperative BMI (p = 0.008), and lower postoperative weight loss at 2- (p = 0.001), 6- (p = 0.01), and 12- (p = 0.04) months after surgery. After matching, no differences were observed up to 3-years post-op. Analysis of education demonstrated no effect on weight loss in both unmatched and matched analyses.
Conclusion
Unmatched analysis demonstrated that low income and race impact short-term weight loss after BS. After matching, however, race, not socioeconomic status, predicted weight loss outcomes up to 1-year.
Similar content being viewed by others
References
Dalstra JA, Kunst AE, Borrell C et al (2005) Socioeconomic differences in the prevalence of common chronic diseases: an overview of eight European countries. Int J Epidemiol 34:316–326
Stringhini S, Carmeli C, Jokela M et al (2017) Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1·7 million men and women. Lancet 389:1229–1237
Lewer D, Jayatunga W, Aldridge RW et al (2020) Premature mortality attributable to socioeconomic inequality in England between 2003 and 2018: an observational study. Lancet Public Health 5:e33–e41
Muennig P, Franks P, Jia H et al (2005) The income-associated burden of disease in the United States. Soc Sci Med 61:2018–2026
Chetty R, Stepner M, Abraham S et al (2016) The association between income and life expectancy in the United States, 2001–2014. JAMA 315:1750–1766
Mohammed SH, Habtewold TD, Birhanu MM et al (2019) Neighbourhood socioeconomic status and overweight/obesity: a systematic review and meta-analysis of epidemiological studies. BMJ Open 9:e028238
Adler NE, Newman K (2002) Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood) 21:60–76
Singh GK, Siahpush M, Hiatt RA et al (2011) Dramatic increases in obesity and overweight prevalence and body mass index among ethnic-immigrant and social class groups in the United States, 1976–2008. J Community Health 36:94–110
Wang Y, Beydoun MA (2007) The obesity epidemic in the United States–gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev 29:6–28
Fan JX, Wen M, Li K (2020) Associations between obesity and neighborhood socioeconomic status: variations by gender and family income status. SSM Popul Health 10:100529
Livingston EH, Ko CY (2004) Socioeconomic characteristics of the population eligible for obesity surgery. Surgery 135:288–296
Martin M, Beekley A, Kjorstad R et al (2010) Socioeconomic disparities in eligibility and access to bariatric surgery: a national population-based analysis. Surg Obes Relat Dis 6:8–15
Keating C, Backholer K, Moodie M et al (2015) Differences in the rates of treatment of severe obesity using bariatric surgery across socioeconomic groups. JAMA Surg 150:367–368
Wallace AE, Young-Xu Y, Hartley D et al (2010) Racial, socioeconomic, and rural-urban disparities in obesity-related bariatric surgery. Obes Surg 20:1354–1360
Bhogal SK, Reddigan JI, Rotstein OD et al (2015) Inequity to the utilization of bariatric surgery: a systematic review and meta-analysis. Obes Surg 25:888–899
Hecht LM, Pester B, Braciszewski JM et al (2020) Socioeconomic and racial disparities in bariatric surgery. Obes Surg 11:1–5
Keith CJ, Gullick AA, Feng K et al (2018) Predictive factors of weight regain following laparoscopic Roux-en-Y gastric bypass. Surg Endosc 32:2232–2238
Winkleby MA, Jatulis DE, Frank E et al (1992) Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health 82:816–820
Dilektasli E, Erol MF, Cayci HM et al (2017) Low educational status and childhood obesity associated with insufficient Mid-term weight loss after sleeve gastrectomy: a retrospective observational cohort study. Obes Surg 27:162–168
Mahoney ST, Strassle PD, Farrell TM et al (2019) Does lower level of education and health literacy affect successful outcomes in bariatric surgery? J Laparoendosc Adv Surg Tech A 29:1011–1015
Akkary E, Nerlinger A, Yu S et al (2009) Socioeconomic predictors of weight loss after laparoscopic Roux-Y gastric bypass. Surg Endosc 23:1246–1251
Jalilvand A, Blaszczak A, Dewire J et al (2019) Laparoscopic sleeve gastrectomy is an independent predictor of poor follow-up and reaching ≤ 40% excess body weight loss at 1, 2, and 3 years after bariatric surgery. Surg Endosc 34:2572–2584
Advameg, Inc. “Columbus, OH.” City-Data.com. (2020). http://www.city-data.com/city/Columbus-Ohio.html
U.S. General Services Administration TTS. IMPACT (2020). http://www.data.gov/impact/
Pew Research Center. Social & Demographic Trends (2016). http://www.pewresearch.org/
Doumouras AG, Lee Y, Babe G et al (2020) The hidden cost of an extensive preoperative work-up: predictors of attrition after referral for bariatric surgery in a universal healthcare system. Surg Endosc 34:988–995
Smith ED, Layden BT, Hassan C et al (2018) Surgical treatment of obesity in Latinos and African Americans: future directions and recommendations to reduce disparities in bariatric surgery. Bariatr Surg Pract Patient Care 13:2–11
Mainous AG, Johnson SP, Saxena SK et al (2013) Inpatient bariatric surgery among eligible black and white men and women in the United States, 1999–2010. Am J Gastroenterol 108:1218–1223
Palli SR, Rizzo JA, Heidrich N (2018) Bariatric surgery coverage: a comprehensive budget impact analysis from a payer perspective. Obes Surg 28:1711–1723
Altieri MS, Yang J, Yin D et al (2019) Patients insured by Medicare and Medicaid undergo lower rates of bariatric surgery. Surg Obes Relat Dis 15:2109–2114
Gould KM, Zeymo A, Chan KS et al (2019) Bariatric surgery among vulnerable populations: the effect of the affordable care act's Medicaid expansion. Surgery 166:820–828
Halloran K, Padwal RS, Johnson-Stoklossa C et al (2011) Income status and approval for bariatric surgery in a publicly funded regional obesity program. Obes Surg 21:373–378
Gullick AA, Graham LA, Richman J et al (2015) Association of race and socioeconomic status with outcomes following laparoscopic Roux-en-Y gastric bypass. Obes Surg 25:705–711
Admiraal WM, Celik F, Gerdes VE et al (2012) Ethnic differences in weight loss and diabetes remission after bariatric surgery: a meta-analysis. Diabetes Care 35:1951–1958
Kitamura R, Chen R, Trickey A et al (2020) Positive and negative independent predictive factors of weight loss after bariatric surgery in a veteran population. Obes Surg 3:1–7
Turner M, Vigneswaran Y, Dewey E et al (2019) Weight loss and co-morbidity resolution between different races and ethnicities after gastric bypass. Surg Obes Relat Dis 15:1943–1948
King RA, Patel KC, Mark VM et al (2019) Role of ethnicity on weight loss and attrition after bariatric surgery. Obes Surg 29:3577–3580
Jambhekar A, Maselli A, Robinson S et al (2018) Demographics and socioeconomic status as predictors of weight loss after laparoscopic sleeve gastrectomy: a prospective cohort study. Int J Surg 54:163–169
Wood MH, Carlin AM, Ghaferi AA et al (2019) Association of race with bariatric surgery outcomes. JAMA Surg 154:e190029
Ofori A, Keeton J, Booker Q et al (2020) Socioecological factors associated with ethnic disparities in metabolic and bariatric surgery utilization: a qualitative study. Surg Obes Relat Dis 16:786–795
Kim KH, Bursac Z, DiLillo V et al (2009) Stress, race, and body weight. Health Psychol 28:131–135
Weinsier RL, Hunter GR, Zuckerman PA et al (2000) Energy expenditure and free-living physical activity in black and white women: comparison before and after weight loss. Am J Clin Nutr 71:1138–1146
Carden A, Blum K, Arbaugh CJ et al (2019) Low socioeconomic status is associated with lower weight-loss outcomes 10-years after Roux-en-Y gastric bypass. Surg Endosc 33:454–459
Erdogdu UE, Cayci HM, Tardu A et al (2019) Health literacy and weight loss after bariatric surgery. Obes Surg 29:3948–3953
Marín-León L, Oliveira HB, Barros MB et al (2007) Social inequality and common mental disorders. Braz J Psychiatry 29:250–253
Kurspahić Mujčić A, Mujčić A (2019) The relationship between education and self-reported mental and physical health. Med Glas (Zenica) 16:102–107
Small L, Aplasca A (2016) Child obesity and mental health: a complex interaction. Child Adolesc Psychiatr Clin N Am 25:269–282
Testa G, Granero R, Siragusa C et al (2019) Psychological predictors of poor weight loss following LSG: relevance of general psychopathology and impulsivity. Eat Weight Disord. https://doi.org/10.1007/s40519-019-00800-x
Pinto-Bastos A, de Lourdes M, Brandão I et al (2019) Weight loss trajectories and psychobehavioral predictors of outcome of primary and reoperative bariatric surgery: a 2-year longitudinal study. Surg Obes Relat Dis 15:1104–1112
Pinto-Bastos A, Conceição EM, Machado PPP (2017) Reoperative bariatric surgery: a systematic review of the reasons for surgery, medical and weight loss outcomes, relevant behavioral factors. Obes Surg 27:2707–2715
Freese KE, Althouse AD, Ramanathan R et al (2017) Presurgery weight loss goals, depressive symptoms, and weight loss among women undergoing bariatric surgery. Bariatr Surg Pract Patient Care 12:67–71
Ahmed B, King WC, Gourash W et al (2018) Long-term weight change and health outcomes for sleeve gastrectomy (SG) and matched Roux-en-Y gastric bypass (RYGB) participants in the Longitudinal Assessment of Bariatric Surgery (LABS) study. Surgery 164:774–783
Semega J et al (2019) Income and poverty in the United States: 2018. http://www.census.gov/library/publications/2019/demo/p60-266.html
Manning S, Pucci A, Carter NC et al (2015) Early postoperative weight loss predicts maximal weight loss after sleeve gastrectomy and Roux-en-Y gastric bypass. Surg Endosc 29:1484–1491
Maciejewski ML, Arterburn DE, Van Scoyoc L et al (2016) Bariatric surgery and long-term durability of weight loss. JAMA Surg 151:1046–1055
Chu L, Howell B, Steinberg A et al (2019) Early weight loss in adolescents following bariatric surgery predicts weight loss at 12 and 24 months. Pediatr Obes 14:e12519
Ma Y, Pagoto SL, Olendzki BC et al (2006) Predictors of weight status following laparoscopic gastric bypass. Obes Surg 16:1227–1231
Toussi R, Fujioka K, Coleman KJ (2009) Pre- and postsurgery behavioral compliance, patient health, and postbariatric surgical weight loss. Obesity (Silver Spring) 17:996–1002
Vidal P, Ramón JM, Goday A et al (2014) Lack of adherence to follow-up visits after bariatric surgery: reasons and outcome. Obes Surg 24:179–183
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to data collection. SN was involved in database and study design. AG, RT and SN performed data analysis. SN, AG, RT and JC performed data interpretation. JC and SN prepared the manuscript. All authors participated in critical review and revision of the manuscript.
Corresponding author
Ethics declarations
Disclosures
Kayla Diaz, Anand Gupta, Robert Tamer, Muna Tamimi and Drs. J. C. Chen, Anahita Jalilvand, Vivian Wang, Jennwood Chen, Bradley Needleman, and Sabrena Noria have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, J.C., Jalilvand, A., Wang, V. et al. Influence of sociodemographic variables on weight loss outcomes up to 3-years following primary bariatric surgery. Surg Endosc 35, 5774–5786 (2021). https://doi.org/10.1007/s00464-020-08066-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08066-6