Abstract
Background
Minimal access surgery has fast become the standard of care for many operative procedures, but is associated with lot of ergonomic stress to the surgeons performing these procedures, which may result in reduction in surgeon’s performance and work capacity. In this study, we evaluated the impact of structured training program in improving the ergonomic stress in trainee laparoscopic surgeons.
Methods
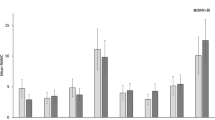
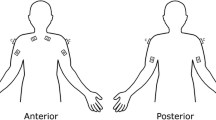
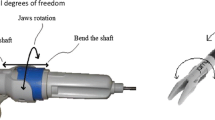
Laparoscopic surgeons were divided in 2 groups: trainee surgeons (ten) and expert surgeons (three). Baseline surface electromyography (sEMG) data were collected from bilateral deltoid, biceps brachii, forearm extensors, and pronator teres during a predefined suturing task on Tuebingen trainer with integrated porcine organs in both the groups. Trainee surgeons underwent 20 h of laparoscopic intra-corporeal suturing training and surface electromyography data were recorded at the end of training again and compared with baseline.
Results
Experts were found to have lower muscle activation (p < 0.05) and muscle work (p < 0.05) and better bimanual dexterity than the trainee surgeons at baseline. After training, the trainee surgeons showed significant improvement (p = 0.01), but still did not reach the values of the expert surgeons (p = 0.01). Right deltoid and pronator teres muscles were found to have maximal activity while performing intra-corporeal suturing.
Conclusion
Structured and focused training outside operation theater can significantly reduce unnecessary muscle activation of trainee laparoscopic surgeons and better dexterity leading on to lesser ergonomic stress and thus possibly may reduce the risk of development of future musculo-skeletal disorders.



Similar content being viewed by others
References
Zhang F-W, Zhou Z-Y, Wang H-L, Zhang J-X, Di B-S, Huang W-H, Yang K-H (2014) Laparoscopic versus open surgery for rectal cancer: a systematic review and meta-analysis of randomized controlled trials. Asian Pac J Cancer Prev 15:9985–9996
Gui L, Liu Y, Qin J, Zheng L, Huang Y-J, He Y, Deng W-S, Qian B-B, Luo M (2016) Laparoscopic common bile duct exploration versus open approach in cirrhotic patients with choledocholithiasis: a retrospective study. J Laparoendosc Adv Surg Tech A 26:972–977
Korman JE, Ho T, Hiatt JR, Phillips EH (1997) Comparison of laparoscopic and open adrenalectomy. Am Surg 63:908–912
Alleblas CCJ, de Man AM, van den Haak L, Vierhout ME, Jansen FW, Nieboer TE (2017) Prevalence of musculoskeletal disorders among surgeons performing minimally invasive surgery: a systematic review. Ann Surg 266:905–920
Esposito C, Najmaldin A, Schier F, Yamataka A, Ferro M, Riccipetitoni G, Czauderna P, Ponsky T, Till H, Escolino M, Iaquinto M, Marte A, Saxena A, Settimi A, Rothenberg S (2014) Work-related upper limb musculoskeletal disorders in pediatric minimally invasive surgery: a multicentric survey comparing laparoscopic and sils ergonomy. Pediatr Surg Int 30:395–399
Bansal VK, Tamang T, Misra MC, Prakash P, Rajan K, Bhattacharjee HK, Kumar S, Goswami A (2012) Laparoscopic suturing skills acquisition: a comparison between laparoscopy-exposed and laparoscopy-naive surgeons. JSLS 16:623–631
Bansal VK, Raveendran R, Misra MC, Bhattacharjee H, Rajan K, Krishna A, Kumar P, Kumar S (2014) A prospective randomized controlled blinded study to evaluate the effect of short-term focused training program in laparoscopy on operating room performance of surgery residents (CTRI /2012/11/003113). J Surg Educ 71:52–60
Berguer R, Chen J, Smith WD (2003) A comparison of the physical effort required for laparoscopic and open surgical techniques. Arch Surg 138:967–970
Berguer R (1998) Surgical technology and the ergonomics of laparoscopic instruments. Surg Endosc 12:458–462
Waseda M, Inaki N, Mailaender L, Buess GF (2005) An innovative trainer for surgical procedures using animal organs. Minim Invasive Ther Allied Technol 14:262–266
Bansal VK, Panwar R, Misra MC, Bhattacharjee HK, Jindal V, Loli A, Goswami A, Krishna A, Tamang T (2012) Are short-term focused training courses on a phantom model using porcine gall bladder useful for trainees in acquiring basic laparoscopic skills? Surg Laparosc Endosc Percutan Tech 22:154–160
Uhrich ML, Underwood RA, Standeven JW, Soper NJ, Engsberg JR (2002) Assessment of fatigue, monitor placement, and surgical experience during simulated laparoscopic surgery. Surg Endosc 16:635–639
Hägg GM, Luttmann A, Jäger M (2000) Methodologies for evaluating electromyographic field data in ergonomics. J Electromyogr Kinesiol 10:301–312
Berguer R, Rab GT, Abu-Ghaida H, Alarcon A, Chung J (1997) A comparison of surgeons’ posture during laparoscopic and open surgical procedures. Surg Endosc 11:139–142
Stucky C-CH, Cromwell KD, Voss RK, Chiang Y-J, Woodman K, Lee JE, Cormier JN (2018) Surgeon symptoms, strain, and selections: systematic review and meta-analysis of surgical ergonomics. Ann Med Surg (Lond) 27:1–8
Stylopoulos N, Rattner D (2003) Robotics and ergonomics. Surg Clin North Am 83:1321–1337
Supe AN, Kulkarni GV, Supe PA (2010) Ergonomics in laparoscopic surgery. J Minim Access Surg 6:31–36
Nguyen NT, Ho HS, Smith WD, Philipps C, Lewis C, De Vera RM, Berguer R (2001) An ergonomic evaluation of surgeons’ axial skeletal and upper extremity movements during laparoscopic and open surgery. Am J Surg 182:720–724
Pérez-Duarte FJ, Sánchez-Margallo FM, Martín-Portugués ID-G, Sánchez-Hurtado MA, Lucas-Hernández M, Sánchez-Margallo JA, Usón-Gargallo J (2013) Ergonomic analysis of muscle activity in the forearm and back muscles during laparoscopic surgery: influence of previous experience and performed task. Surg Laparosc Endosc Percutan Tech 23:203–207
Dalager T, Søgaard K, Bech KT, Mogensen O, Jensen PT (2017) Musculoskeletal pain among surgeons performing minimally invasive surgery: a systematic review. Surg Endosc 31:516–526
Lawson EH, Curet MJ, Sanchez BR, Schuster R, Berguer R (2007) Postural ergonomics during robotic and laparoscopic gastric bypass surgery: a pilot project. J Robot Surg 1:61–67
McAtamney L, Nigel Corlett E (1993) RULA: a survey method for the investigation of work-related upper limb disorders. Appl Ergon 24:91–99
Lee GI, Lee MR, Clanton T, Clanton T, Sutton E, Park AE, Marohn MR (2014) Comparative assessment of physical and cognitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc 28:456–465
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Washim Firoz Khan, Asuri Krishna, Atanu Roy, Om Prakash, Ashok Kumar Jaryal, Kishore K Deepak, Hemanga Bhattacharjee, Vishnubhatla Sreenivas, Virinder Kumar Bansal have declared that they have no conflicts of interest or financial ties to disclose.
Ethical approval
A formal ethical clearance was taken for this study.
Informed consent
An informed consent was taken at the time of procedure from each participant.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khan, W.F., Krishna, A., Roy, A. et al. Effect of structured training in improving the ergonomic stress in laparoscopic surgery among general surgery residents. Surg Endosc 35, 4825–4833 (2021). https://doi.org/10.1007/s00464-020-07945-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07945-2