Abstract
Background
Primary palmar hyperhidrosis is a severely debilitating condition that can affect patients of any age. We report our experience with thoracoscopic sympathicolysis in a large cohort of children less than 14 years of age.
Methods
All children who underwent thoracoscopic sympathicolysis from April 2005 through January 2017 were evaluated retrospectively. The procedure entailed bilateral bipolar fulguration of the second and third thoracic ganglia with transverse disruption of collateral nerve fibers along the third and fourth rib. Demographic information, as well as postoperative outcome, complications, and satisfaction were analyzed.
Results
Over the 12 year study interval, a total of 102 children underwent thoracoscopic sympathicolysis for palmar hyperhidrosis. Complete follow-up was available for 98 patients (median age 12 [range 5–14] years; 38 boys [39%]). Median follow-up was 4 [range 2–12] years. Complete palmar dryness was achieved in 93 (95%) cases. One patient suffered postoperative unilateral ptosis, 6 reported gustatory sweating, and 65 experienced compensatory sweating. Average postoperative rating on a 1 (lowest) to 10 (highest) rating scale was 9, with 97 (99%) patients saying that they would undergo the procedure again.
Conclusion
Our technique of thoracoscopic sympathicolysis in children was associated with very high postoperative satisfaction, despite a high rate of compensatory sweating and occasional autonomic gustatory sweating. Other more severe complications in this age group were rare.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Primary palmar hyperhidrosis is a disease of the autonomous nervous system characterized by excessive sweating over 6 months in duration that impairs daily activities [1]. In children, this can lead to handwriting difficulties in school, since the paper becomes soaked, causing the ink to run, compromising neatness and legibility. It also can cause social isolation and difficulty playing sports because a ball or other equipment may slip when gripped with a wet hand. The impact of palmar hyperhidrosis in children is often underappreciated. Patients are often ridiculed and become frustrated with their condition. As in adults, constantly having wet hands can stigmatize children and lead to introversion and low self-esteem.
Treatment options include topical therapy with aluminum salts (deodorant), oral anticholinergics such as glycopyrrolate or oxybutinin, calcium-channel blockers, clonidine, as well as iontophoresis, or botulinum injections [2]. Iontophoresis can improve palmar hyperhidrosis in up to 80% of cases but requires a series of treatments [3]. Oxybutinin has been reported to improve symptoms in 90% of cases, but requires long-term medication causing oropharyngeal dryness [4]. Finally, botulinum injections last only on average 7 months before symptoms return [5]. The only long-term therapy for severe palmar hyperhidrosis is operative sympathectomy or sympathicolysis, which is most often performed thoracoscopically.
We report our experience over more than a decade with thoracoscopic sympathicolysis using a special technique that entails bipolar fulguration of the second and third thoracic ganglia and interruption of the collateral fibers along the third and fourth ribs, and compare our outcome to that of other published series.
Methods
Study design
Approval was granted by the Ethics committee of the Institution (Y0941622T). The study was registered at www.researchregistry.com (researchregistry3903). All patients and their parents consented to participation of the study.
A retrospective review was performed on all patients 14 years of age and younger who underwent thoracoscopic sympathicolysis in the described technique from April 2005 through January 2017 at the University Hospital Las Palmas de Gran Canaria, Spain. Data were collected through paper and electronic medical records. A standardized schedule for follow-up for at least 2 years after the procedure was shared with the patients postoperatively and followed through by telephone or mail follow-up. Phone numbers were made available for any questions or complications, should they arise in the interim. All patients underwent a detailed preoperative and postoperative physical exam, and were asked to answer a postoperative questionnaire that included a satisfaction scale from 1 (least) to 10 (highest) satisfaction, along with a query of postoperative symptoms and complications.
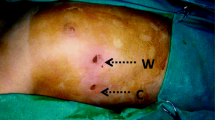
Surgical technique (Fig. 1)
Technique of thoracoscopic sympathicolysis. The sympathetic chain (between arrows) is identified over the head of the second rib (2) as seen in (A). It is fulgurated using bipolar diathermy through the intact pleura (B, arrow). Using electrocautery hook, the pleura and periosteum is opened laterally for 3 cm on top of the rib (C), and the procedure is repeated along the 3rd rib (D, 3)
Thoracoscopic sympathicolysis is performed under general anesthesia with conventional single-lumen intubation using low-pressure carbon dioxide insufflation (between 5 and a maximum of 10 mmHg). A one-time bilateral procedure is performed during the same anesthesia. All patients are placed in semi-sitting position with 90° abduction of the arms and the elbows slightly flexed. Two 5 mm incisions are made after the skin is injected with local anesthetic: the first in the mid axillary line in the third intercostal space, the second slightly anterior in the fifth intercostal space. The first trocar was placed using an open technique in apnea ventilation mode to minimize the risk of lung injury. Standard tidal volume ventilation is used by anesthesia during the procedure. The ipsilateral lung is collapsed by using valved trocars and insufflating carbon dioxide at a pressure of 1 mm Mercury over positive end expiratory pressure (PEEP). After identifying the sympathetic chain by vision and palpation, bipolar electrofulguration of the chain is performed through the intact pleura, starting just below the second rib (T2) and continuing down to the head of the fourth rib (T3). In doing so, the sympathetic chain “tenses and draws” itself below the intact parietal pleura, making the chain identification easier. Short single impulses are used, avoiding the dispersion of heat to adjacent structures. We use a 12 W energy setting in all cases, which is comparably low but proved adequate for effective fulguration of the sympathetic chain. Subsequently, a monopolar hook is used to make 3 cm long transverse incisions of the parietal pleura and periosteum along the third and fourth rib from medial to lateral, transecting the sympathetic chain and any collateral nerve fibers. After evacuation of the capnothorax, the trocars are removed and the wounds closed. No chest drains were left in place. All patients were operated by two board-certified pediatric surgeons.
Results
Demographics
During the study interval, a total of 102 patients were operated in the described fashion. Of those, complete follow-up was available from 98 patients. The median age of these at the time of the intervention was 12 years (Quartile 1: 11 years, Quartile 3: 14 years, range 5–14 years) and most were girls (60 girls vs 38 boys). Symptoms started at a mean age of 4.8 years, and parents of 23 patients said that the palmar hyperhidrosis was perceptible from infancy. The median follow-up was 4 years (range 2–12 years) after the procedure.
Intraoperative and postoperative complications
Mean operative time was 90 min (95% confidence interval 85–95 min). Complete dryness of the hands was achieved in 93 (95%) patients, one hand in one patient stayed humid after an unsuccessful redo procedure, partial moistness was observed in 4 (4.1%) cases. A redo procedure was performed in 3 (3%) cases, 2 of which were successful. There were no intraoperative complications. Postoperatively, one patient presented with unilateral mild ptosis, which was not functionally impairing.
Postoperative compensatory and gustatory sweating
Compensatory sweating (CS) appeared in 65 (66%) patients, 6 of which were transient and resolved spontaneously, another 12 reported decreasing CS with time. Long-term CS was therefore found in 59 (60%). Of those with any CS, 26 (44%) were not bothered by it at all, while only 3 saw it as a major impairment. The vast majority (64%) of those with CS reported CS within the first 3 months with a peak in the second month after the procedure. The location of CS were the feet in about half of patients 33), the back in 27, the trunk in 21, the axilla in 10, and the entire body in 5 patients. Autonomic gustatory sweating (upon tasting or smelling food) was reported in 6 patients.
Satisfaction
Postoperative patient-rated satisfaction on a scale of 1–10, stratified by gender and compensatory sweating, is presented in Table 1. Overall, patients were very satisfied at a median of 9 (range 5–10). Boys with compensatory sweating were less satisfied than others (p = 0.03), while there was no difference in girls. Upon questioning, 97 patients said they would have the procedure performed again, only 1 patient did not (an adolescent with compensatory sweating).
Discussion
Primary palmar hyperhidrosis (PPH) is a poorly understood derangement of the sympathetic system that leads to uncontrollable sweating of the hands. The overall incidence has been reported at around 5–15% of the population [6,7,8]. While PPH is well recognized in adults as a debilitating condition for social interaction, it has only received attention in children in the last two decades. Around 1.6% of adolescents and 0.6% of prepubertal children reportedly affected [9].
A literature search was performed using the subject terms syntax 〈thoracoscopic 〉 , 〈sympathectomy〉 OR 〈sympathicolytic〉 , 〈palmar hyperhidrosis〉, 〈children〉 in PubMed. The results were screened for relevance and the references in those respective studies were snowballed for a comprehensive overview of the subject. The results of all relevant studies were combined in a table to compare reported demographics and outcome. Table 2 shows the results of our systematic review. A total of 17 reviews were found, published from 1994 until 2019, all of them case series that included between 12 and 350 patients. There were no controlled trials or comparative studies. The techniques employed showed broad heterogeneity, as did the age ranges. Compensatory sweating was reported in 0–90%, patients stated that they would have the procedure performed again in 87–100%, while satisfaction rate in the published studies ranged from 57–100%.
Compared to the other published series, the cohort evaluated in this study is, on average, the youngest and one of the largest. Therefore, the findings are particularly useful to shed insight into the particularities of treating primary palmar hyperhidrosis by thoracoscopic sympathicolysis in young children. Despite the high rate of postoperative compensatory sweating, children are very satisfied with the procedure and would retrospectively choose to have the intervention performed again. These findings corroborate the findings of other published reports and support the notion that early operative intervention is justified and that there is no rationale to delay treatment for primary palmar hyperhidrosis until adolescence or adulthood.
Our study found that symptoms usually started before school start, and that hyperhidrosis was noticeable by the parents as early as infancy in about a quarter of patients. This implies that primary hyperhidrosis may be a congenital problem, at least in a substantial portion of patients, and that primary care physicians and pediatricians should specifically ask for signs and symptoms during well-child checks and routine care visits. Thereby, early intervention is possible and the associated problems with handwriting and sports participation can be proactively identified and avoided. This supports the recommendations by Steiner et al. [10] who compared children (ages 6–12 years), adolescents (ages 13–18 years), and adults (ages 19–29 years and found that postoperative satisfaction rates were similar, but that the willingness to have undergone the procedure again was significantly higher in the first two groups. Only one report contradicts these findings, arguing that older patients have a greater reduction in sweating compared to younger ones [11]. However, the authors base their conclusions solely on subjective findings.
Sweating patterns are indeed an interesting topic in this context. Normal sweating of the palms and soles is appreciable after birth, while axillary sweating does not begin until puberty [12]. In our series, axillary sweating was never part of the initial complaint, nor a frequent location for compensatory sweating. Therefore, continuing the sympathicolysis as far caudal as thoracic levels T4 or T5 does not seem reasonable in children under 14 years of age. Since there is no universal definition for compensatory sweating, this entity is based on subjective reports by the patients. In our series, it was noted in about two thirds of cases, and only in 6 of these (roughly 10%) had longterm spontaenous resolution. In our patients, the most common areas affected by compensatory sweating were the trunk (36%), back (46%), and soles of the feet (56%). Overall in our patients, we noted that over half had a combination of palmar and plantar hyperhydrosis, even before the procedure. While typically the entity is described as primary palmar hyperhidrosis (PPH), we would argue that children especially may have what should be called primary palmar-plantar hyperhidrosis (PPPH).
Another unexpected finding in our series is the postoperative gustatory sweating that appeared in 6 patients. This is something not previously reported, but was part of our routine follow-up questions since one of our early patients had complained of profuse sweating upon smelling or tasting food. Gustatory sweating is a focal hyperhidrosis that can appear in the context of Frey syndrome [13] after parotid gland surgery or injury. The exact autonomous mechanisms remain unclear [14]. We believe that postoperative gustatory sweating after sympathicolysis or sympathectomy is underreported, since it requires a high level of suspicion by the physician performing the follow-up.
Besides compensatory sweating, complications are exceedingly rare after thoracoscopic sympathicolysis. Although mostly transient Horner syndrome has been described in up to 18% of cases [15], we only encountered one case of mild, but permanent ptosis. There were no intraoperative complications or unusual findings in this particular case. The ptosis was appreciated immediately after the operation. The procedure itself was performed in 2014, so in the latter half of the series, well beyond an expected learning curve. One could speculate that the patient had a variant of a low-lying stellate ganglion. Heat conduction may have played a role, although the technique was performed in exactly the same manner as in the other patients. Over a two year follow-up, by 2016, the ptosis was still appreciable on physical examination, but had improved to the point where her visual axis was not impaired and the patient had no subjective complaints about the ptosis. Other complications such as inadequate resolution or recurrence of hyperhydrosis have been reported in up to 10% of cases [15]. In our series, redo procedures were rarely required (3%).
One of the problems of comparability of studies is that a multitude of different techniques have been used. Not only do different surgeons treat different levels of the sympathetic chain (an overview of the levels is given in Table 2), but different modalities of sympathicolysis or sympathectomy are being employed, ranging from transection, resection, clipping, as well as chemical or CO2-laser ablation [16]. In our center, the described technique has produced exceedingly good results, is reproducible and easy to perform. In 2011, an expert consensus was published [17], noting that interruption of the sympathetic chain should be achieved either by electrocautery (as performed in our center) or clipping. Also, disruption just cranial to the third rib produces the highest success rate in treating primary palmar and craniofacial hyperhidrosis. In another systematic review, the authors found that T2-free interventions lowered the risk of Horner's syndrome without compromising efficacy [18]. However, these conclusions are all based on retrospective reports, mainly in the adult population, and should be validated in prospective controlled trials.
Besides its retrospective data acquisition, the main limitation of our study is the non-validated assessment of postoperative satisfaction. Unfortunately, this is common among the other referenced studies listed in our systematic review (Table 2). It makes comparability difficult, although the numbers reported are surprisingly congruent. Overall, the satisfaction rates after the procedure seem to be almost universally high, irrespective of the technique employed or the target levels on the sympathetic chain. Unfortunately, we lost 4 of the 102 patients to follow-up. Several attempts were made to contact these respective patients and families by telephone, mail, and by a search through the social security system. Unfortunately, they had moved away without any follow-up information. The relatively high follow-up quota of 96% (98 of 102 patients) is most likely associated with the geographic circumstances of the Canary islands, in which the population tends to be confined to one island and remains relatively stable and accessible.
In the meantime, a validated quality of life scale, the so-called hidroQOL© tool has been published [19]. Unfortunately, it is currently only available for adults and includes such items as impact on sex life, which is obviously not appropriate for children 14 years and under. We have thus adapted the questionnaire for our pediatric patient population and are currently enrolling patients in a prospective fashion to objectify the impact of the procedure on postoperative quality of life. In one study in adults, quality of life and self-esteem improved significantly after thoracoscopic sympathectomy, despite a high rate (78%) of compensatory sweating [20].
In summary, our technique of thoracoscopic sympathicolysis produced a high degree of patient satisfaction despite a substantial rate of compensatory sweating comparable to other series. More serious complications were exceedingly rare. Considering the excellent outcome, we advocate that hyperhidrosis be treated early in life as soon as it is identified as a problem that impacts on age-appropriate psychosocial development.
References
Hornberger J, Grimes K, Naumann M, Glaser DA, Lowe NJ, Naver H, Ahn S, Stolman LP, Multi-Specialty Working Group on the Recognition, Diagnosis, and Treatment of Primary Focal Hyperhidrosis (2004) Recognition, diagnosis, and treatment of primary focal hyperhidrosis. J Am Acad Dermatol 51:274–286
Gelbard CM, Epstein H, Hebert A (2008) Primary pediatric hyperhidrosis: a review of current treatment options. Pediatr Dermatol 25:591–598
Dagash H, McCaffrey S, Mellor K, Roycroft A, Helbling I (2017) Tap water iontophoresis in the treatment of pediatric hyperhidrosis. J Pediatr Surg 52:309–312
Wolosker N, Teivelis MP, Krutman M, de Paula RP, Kauffman P, de Campos JRM, Puech-Leao P (2015) Long-term efficacy of oxybutynin for palmar and plantar hyperhidrosis in children younger than 14 years. Pediatr Dermatol 32:663–667
Coutinho dos Santos LH, Gomes AM, Giraldi S, Abagge KT, Marinoni LP (2009) Palmar hyperhidrosis: long-term follow-up of nine children and adolescents treated with botulinum toxin type A. Pediatr Dermatol 26:439–444
Liu Y, Bahar R, Kalia S, Huang RY, Phillips A, Su M, Yang S, Zhang X, Zhou P, Zhou Y (2016) Hyperhidrosis prevalence and demographical characteristics in dermatology outpatients in shanghai and vancouver. PLoS ONE 11:e0153719
Shayesteh A, Janlert U, Brulin C, Boman J, Nylander E (2016) Prevalence and characteristics of hyperhidrosis in Sweden: a cross-sectional study in the general population. Dermatology 232:586–591
Doolittle J, Walker P, Mills T, Thurston J (2016) Hyperhidrosis: an update on prevalence and severity in the United States. Arch Dermatol Res 308:743–749
Bohaty BR, Hebert AA (2014) Special considerations for children with hyperhidrosis. Pediatr Dermatol 32:477–484
Steiner Z, Kleiner O, Hershkovitz Y, Mogilner J, Cohen Z (2007) Compensatory sweating after thoracoscopic sympathectomy: an acceptable trade-off. J Pediatr Surg 42:1238–1242
Leiderman DBD, Milanez de Campos JR, Kauffman P, Tedde ML, Yazbek G, Passos Teivelis M, Wolosker N (2018) The relation between age and outcomes of thoracic sympathectomy for hyperhidrosis: the older the better. J Thorac Cardiovasc Surg 156:1748–1756
Bellet JS (2010) Diagnosis and treatment of primary focal hyperhidrosis in children and adolescents. Semin Cutan Med Surg 29:121–126
Grzybowski A, Sak J (2016) Łucja Frey (1889–1942). J Neurol 263:2358–2359
Ohshima Y, Tamada Y (2016) Classification of systemic and localized sweating disorders. Curr Probl Dermatol 51:7–10
Sinha CK, Kiely E (2013) Thoracoscopic sympathectomy for palmar hyperhidrosis in children: 21 years of experience at a tertiary care center. Eur J Pediatr Surg 23:486–489
Kao MC, Lee WY, Yip KM, Hsiao YY, Lee YS, Tsai JC (1994) Palmar hyperhidrosis in children: treatment with video endoscopic laser sympathectomy. J Pediatr Surg 29:387–391
Cerfolio RJ, De Campos JR, Bryant AS, Connery CP, Miller DL, DeCamp MM, McKenna RJ, Krasna MJ (2011) The society of thoracic surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg 91:1642–1649
Sang H, Li G, Xiong P, Zhu M, Zhu M (2017) Optimal targeting of sympathetic chain levels for treatment of palmar hyperhidrosis: an updated systematic review. Surg Endosc 31:4357–4369
Kamudoni P, Mueller B, Salek MS (2015) The development and validation of a disease-specific quality of life measure in hyperhidrosis: The Hyperhidrosis Quality of LIfe Index (HidroQOL©). Qual Life Res 24:1017–1027
Dharmaraj B, Kosai NR, Gendeh H, Ramzisham AR, Das S (2016) A Prospective cohort study on quality of life after endoscopic thoracic sympathectomy for primary hyperhidrosis. Clin Ter 167:67–71
Cohen Z, Levi I, Pinsk I, Mares AJ (1998) Thoracoscopic upper thoracic sympathectomy for primary palmar hyperhidrosis–the combined paediatric, adolescents and adult experience. Eur J Surg Suppl 580:5–8
Imhof M, Zacherl J, Plas EG, Herbst F, Jakesz R, Függer R (1999) Long-term results of 45 thoracoscopic sympathicotomies for primary hyperhidrosis in children. J Pediatr Surg 34:1839–1842
Lin TS (1999) Transthoracic endoscopic sympathectomy for palmar hyperhidrosis in children and adolescents: analysis of 350 cases. J Laparoendosc Adv Surg Tech A 9:331–334
Lin TS (1999) Transthoracic endoscopic sympathectomy for palmar and axillary hyperhidrosis in children and adolescents. Pediatr Surg Int 15:475–478
Steiner Z, Cohen Z, Kleiner O, Matar I, Mogilner J (2008) Do children tolerate thoracoscopic sympathectomy better than adults? Pediatr Surg Int 24:343–347
Buraschi J (2008) Simpaticólisis videotoracoscópica para el tratamiento de la hiperhidrosis palmar primaria en niños y adolescentes [Videothoracoscopic sympathicolysis procedure for primary palmar hyperhidrosis in children and adolescents]. Arch Argent Pediatr 106:32–35
Wait SD, Killory BD, Lekovic GP, Dickman CA (2010) Biportal thoracoscopic sympathectomy for palmar hyperhidrosis in adolescents. J Neurosurg Pediatr 6:183–187
Kravarusic D, Freud E (2012) Thoracoscopic sympathectomy ganglia ablation in the management of palmer hyperhidrosis: a decade experience in a single institution. Afr J Paediatr Surg 9:143–147
Neves S, Uchoa PC, Wolosker N, Munia MA, Kauffman P, de Campos JRM, Puech-Leao P (2012) Long-term comparison of video-assisted thoracic sympathectomy and clinical observation for the treatment of palmar hyperhidrosis in children younger than 14. Pediatr Dermatol 29:575–579
Shalaby MS, El-Shafee E, Safoury H, El Hay SA (2012) Thoracoscopic excision of the sympathetic chain: an easy and effective treatment for hyperhidrosis in children. Pediatr Surg Int 28:245–248
Soto VV, Merayo EV, Poyato SB, Breña LR (2013) Videothorascopic sympathicotomy treatment through one port for idiopathic palmar and axillary hyperhidrosis in the child Revista Cubana de. Pediatría 85:28–35
Bell D, Jedynak J, Bell R (2014) Predictors of outcome following endoscopic thoracic sympathectomy. ANZ J Surg 84:68–72
Laje P, Rhodes K, Magee L, Klarich MK (2017) Thoracoscopic bilateral T3 sympathectomy for primary focal hyperhidrosis in children. J Pediatr Surg 52:313–316
López SLG, Juárez MD, Machado CAC, González MG, Orbe GMC, Delgado ZQ (2019) Tratamiento videotoracoscópico por dos puertos para la hiperhidrosis palmar y axilar idiopática en el niño [Video-assisted thoracoscopic treatment for two ports for idiopathic palmar and axillary hyperhidrosis in children]. Cir Pediatr 32:115–120
Acknowledgements
Open Access funding provided by Projekt DEAL.
Funding
This research was supported by internal departmental funds only.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Adam Mol and Oliver J. Muensterer have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work is part of a doctoral thesis of Adam Mol at the University Medical Center in Mainz, Germany (Chairman: Prof. Oliver Muensterer). Adam Mol previously worked in Gran Canaria, Spain, where this study was performed. Oliver Muensterer has performed operations in Gran Canaria, Spain.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mol, A., Muensterer, O.J. Over a decade of single-center experience with thoracoscopic sympathicolysis for primary palmar hyperhidrosis: a case series. Surg Endosc 35, 3313–3319 (2021). https://doi.org/10.1007/s00464-020-07769-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07769-0