Abstract
Background
The role of minimally invasive surgery in trauma has continued to evolve over the past 20 years. Diagnostic laparoscopy (DL) has become increasingly utilized for the diagnosis and management of both blunt and penetrating injuries.
Objective
While the safety and feasibility of laparoscopy has been established for penetrating thoracoabdominal trauma, it remains a controversial tool for other injury patterns due to the concern for complications and missed injuries. We sought to examine the role of laparoscopy for the initial management of traumatic injuries at our urban Level 1 trauma center.
Methods
All trauma patients who underwent DL for blunt or penetrating trauma between 2009 and 2018 were retrospectively reviewed. Demographic data, indications for DL, injuries identified, rate of conversion to open surgery, and outcomes were evaluated.
Results
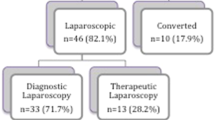
A total of 316 patients were included in the cohort. The mean age was 34.9 years old (± 13.7), mean GCS 14 (± 3), and median ISS 10 (4–18). A total of 110/316 patients (35%) sustained blunt injury and 206/316 patients (65%) sustained penetrating injury. Indications for DL included evaluation for peritoneal violation (152/316, 48%), free fluid without evidence of solid organ injury (52/316, 16%), evaluation of bowel injury (42/316, 13%), and evaluation for diaphragmatic injury (35/316, 11%). Of all DLs, 178/316 (56%) were negative for injury requiring intervention, which was 58% of blunt cases and 55% of penetrating cases. There were no missed injuries noted. Average hospital length of stay was significantly shorter for patients that underwent DL vs conversion to open exploration (2.2 days vs. 4.5 days, p < 0.05).
Conclusion
In this single institution, retrospective study, the high volume of cases appears to show that DL is a reliable tool for detecting injury and avoiding potential negative or non-therapeutic laparotomies. However, when injuries were present, the high rate of conversion to open exploration suggests that its utility for therapeutic intervention warrants further study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The role of diagnostic laparoscopy (DL) after significant traumatic injury has continued to evolve over the past decade. DL, as a diagnostic modality, was initially viewed with skepticism due to concern about missed injuries and the lack of consensus on its indications [1]. Historically, DL has only been used for hemodynamically stable blunt trauma patients. However, traumatologists are now increasingly implementing DL in the evaluation of penetrating injuries given the growing body of literature demonstrating its efficacy and accuracy, with several studies documenting improved clinical outcomes [1,2,3].
The purpose of this study was to explore the utility of DL in both blunt and penetrating trauma patients in an urban Level I trauma center. We hypothesized that the use of DL in blunt and penetrating trauma patients would decrease the rate of non-therapeutic exploratory laparotomies and hospital length of stay (LOS).
Methods
Patient population and clinical data
We performed a retrospective review of all trauma patients who underwent diagnostic or therapeutic laparoscopy between 2009 and 2018 at Grady Memorial Hospital, a busy urban, Level I trauma center in Atlanta, Georgia. After IRB approval was obtained, patients were identified from the institution’s trauma database. Data on patient demographics (age, GCS, ISS), vital signs on presentation (systolic blood pressure, shock index), injury mechanism (penetrating vs. blunt), indications for DL, injuries identified, and outcomes were collected from review of the electronic medical records. Data were extracted and entered into a database by two of the authors. Coding of penetrating vs. blunt injury was based on the ICD-10 Primary External Cause Code. Indications for DL were determined by documentation in operative and clinical notes.
Primary outcomes included rate of conversion to laparotomy and rates of missed injury. Rate of conversion to exploratory laparotomy and missed injuries were determined by review of operative notes in the medical record. Secondary outcomes included intensive care unit and hospital LOS, ventilator days, deep venous thrombosis (DVT), pneumonia, superficial site infection (SSI), and mortality rates.
Definitions
Cases were defined as “negative” if no injury was identified or “non-therapeutic” if no injury was identified that required intervention. “Missed injuries” were defined as intraperitoneal injuries diagnosed after conversion to open laparotomy if the injury was not suspected at time of laparoscopy, as well as any injury diagnosed post-operatively.
Statistical analyses
Means (standard deviations, SD) and medians (interquartile ranges, IQR) were calculated for normally distributed and skewed continuous variables, respectively. Frequencies and percentages were used to describe distributions of categorical variables.
Chi-square test was used for comparison of hospital LOS while Fischer’s exact test was used for comparison of SSI, pneumonia, DVT, and death between DL and laparotomy groups. Mann–Whitney U test was used for ventilator days and ICU LOS to compare the two groups. A two-sided p-value of ≤ 0.05 was used as a cutoff for statistically significance.
Results
Patient demographics
A total of 316 trauma patients were included in the cohort. The mean age was 34.9 years (± 13.7), mean GCS 14 (± 2.6) and median ISS 10 (4–18). Most injuries were penetrating 206/316 (65%) vs 110/316 (35%) blunt. Mean systolic blood pressure on arrival was 130 mmHg (± 22) and mean shock index was 0.76 (± 0.23).
Indications
The most common indications for DL included evaluation for peritoneal violation (152/316, 48%), free fluid without evidence of solid organ injury (52/316, 16%), evaluation of potential bowel injury (42/316, 13%), and evaluation for diaphragmatic injury (35/316, 11%).
Outcomes
Of the 316 cases, 178 (56%) DLs were negative or non-therapeutic. Of the 110 patients with blunt traumatic injuries, 64 (58%) had negative or non-therapeutic DLs. Of the 206 patients presenting after penetrating trauma, 114 (55%) had negative or non-therapeutic DLs. 112/316 (35%) cases were converted to open (34% of penetrating cases and 39% of blunt cases). There were 21 (6.6%) cases converted from DL to non-therapeutic exploratory laparotomy, representing 18% of all laparotomies. Indications for conversion included hemoperitoneum (n = 6), fascial violation (n = 5), mesenteric laceration (n = 4), retroperitoneal or solid organ hematoma (n = 3), need for better visualization (n = 2), and iatrogenic injury to the gallbladder (n = 1). Of note, there were no missed injuries reported in the entire cohort.
After stratifying by organs injured and conversion to open exploration, there were 34 diaphragm injuries, 30 (88%) of which required open repair. The stomach, small bowel, and colon were injured 9, 34, and 42 times, respectively, of which 8 (89%), 32 (94%), and 39 (93%) were converted to exploratory laparotomy. Of the 36 liver injuries and 17 splenic injuries, 21 (58%) and 16 (94%), respectively, were converted to open, while 1/2 (50%) kidney and 1/1 (100%) bladder injuries were repaired through exploratory laparotomy (Table 1). A secondary analysis of liver injuries was then performed. Of the 36 liver injuries, 28 (78%) were caused by penetrating injury and 8 (22%) were due to blunt trauma. A lower percentage of the penetrating injuries 16/28 (57%) were converted to open while 5/8 (62%) of the blunt injuries required open exploration (p = 1).
Regarding secondary outcomes, the number of SSIs was 1 in both the laparoscopy (1/204, 0.5%) and laparotomy (1/112, 0.9%) group (p = 1). DVT rate was 0% for the laparoscopy group (0/204) and 1.8% in the laparotomy group (2/112) (p = 0.12). Pneumonia occurred in 3.9% of the laparoscopy group (8/204) and 6.3% of the laparotomy group (7/112) (p = 0.5). Ventilator days and ICU LOS were similar between groups (median 0 vs 0, IQR 0, p = 0.68 and median 0 vs 0, IQR 3, p = 0.53, respectively). Hospital LOS was significantly shorter for patients that underwent DL vs. DL converted to open laparotomy (2.2 days vs 4.5 days; p < 0.05). Overall mortality was 1.5% (3/204) for laparoscopy group and 1.8% (2/112) for laparotomy group (p = 1) (Table 2).
Discussion
Despite the advances in diagnostic modalities over the past few decades, accurate diagnosis of clinically significant intraperitoneal injuries in blunt and penetrating trauma remains challenging. A continuum from non-invasive tests such as hemodynamic monitoring and physical exam, to imaging with X-ray, computed tomography (CT) scan and ultrasound, to invasive procedures such as diagnostic peritoneal lavage (DPL), DL, and exploratory laparotomy can be used to aid in identification and treatment of injury [1,2,3].
In 1995, a retrospective review by Sosa et al. of abdominal gunshot wounds found that DL resulted in lower negative exploratory laparotomy rates along with shorter hospital stays and decreased morbidity when compared to negative exploratory laparotomy [4, 5]. Since then, there is a growing body of literature suggesting DL is both safe and accurate in the diagnosis of intraperitoneal injury. A systematic review of 2569 patients undergoing DL for penetrating injuries demonstrated that 60% were spared a non-therapeutic laparotomy [2]. Furthermore, Liu et al. conducted a prospective trial to compare sensitivity and specificity of DPL, CT scan, and Focused Assessment with Sonography in Trauma (FAST) in the diagnosis of injury requiring operative intervention after blunt abdominal trauma in hemodynamically stable patients. They observed DPL had the highest sensitivity but lowest specificity when compared to CT and FAST [3]. CT scan sensitivity (94%) and specificity (95%) improved with penetrating abdominal trauma according to a 2009 meta-analysis [4]. However, these values significantly decrease for diagnosis of bowel injury in blunt trauma with sensitivity reported as low as 64%, with an accuracy of 82% [6]. Interestingly, a 2017 study found CT more accurately diagnosed location of small bowel injury compared to large bowel although concordance rates were still only 83.7% and 46.2%, respectively [7]. In contrast, a 2013 meta-analysis found that 23 of 50 studies reported a sensitivity, specificity, and accuracy of 100% for DL in abdominal trauma patients [2].
One of the most significant advantages to DL is the avoidance of non-therapeutic laparotomy. Ahmad et al. demonstrated that DL helped avoid 77% of unnecessary laparotomies in hemodynamically stable patients with penetrating abdominal trauma [8]. Similarly, Fabian et al. found 53% of laparotomies were avoided without a single complication or missed injury [9]. Cherry and colleagues found DL had a sensitivity of 100%, specificity of 76%, positive predictive value of 53%, and negative predictive value of 100%, meaning that a negative laparoscopy excludes the need for laparotomy [10]. Unnecessary laparotomies decreased from 60.7 to 0% with blunt injuries and 78.9 to 16.9% with penetrating trauma in a study conducted by Taner et al. [11]. A study specifically analyzing anterior abdominal stab wounds found that 26% of laparotomies were non-therapeutic when DL was not utilized [12]. Laparotomies can result in significant morbidity for the patient as well as longer hospital stay and increased healthcare costs. Between 10 and 40% of patients who undergo negative laparotomy will experience a complication [13,14,15]. Laparoscopy is not as widely accepted in trauma as it is for elective general surgery, likely due to the urgent nature of trauma surgery and concern for incomplete visibility resulting in missed injuries [16].
Our study demonstrates the benefit of DL for the initial evaluation of intra-abdominal injury among hemodynamically stable trauma patients. We found that it reduced the number of negative and non-therapeutic laparotomies without an increased risk of missed injuries. The hospital LOS for patients undergoing DL was 50% lower than for those who underwent laparotomy. In terms of infectious or thrombotic complications including SSI, pneumonia, and DVT, there was no significant difference found between DL versus conversion to laparotomy. There was also no difference found in ventilator days, ICU LOS, or mortality between the two groups.
We found that conversion to open was more common in the setting of injury to any solid organ or hollow viscus except the liver. The high conversion rate could be explained by the urgency of trauma surgery and inability to fully visualize the surgical field with subsequent concern for missed injury. However, as surgeons become more comfortable with laparoscopy, especially in their residency training, there may be a shift towards using laparoscopy for definitive management of traumatic injuries [17].
Limitations of our study include its retrospective design and single institution data. Data were collected from a very busy civilian trauma center, and therefore, our findings may not be generalizable to other trauma centers. The use of laparoscopy is also surgeon dependent and its use will vary according to the skill set of the operating surgeon.
Conclusion
DL appears to be a reliable method to initially identify injuries in trauma patients whether they sustain blunt or penetrating trauma. Initial evaluation with laparoscopy may also decrease hospital LOS in these patients. While DL seems to be an accurate diagnostic tool, its utility for therapeutic intervention continues to be surgeon dependent.
References
Ivatury R, Simon RJ, Stahl WM (1993) A critical evaluation of laparoscopy in penetrating abdominal trauma. J Trauma 34(6):822–827
O’Malley E, Boyle E, O’Callaghan A et al (2013) Role of laparoscopy in penetrating trauma: a systematic review. World J Surg 37(1):113–122
Liu M, Lee CH, P’eng FK (1993) Prospective comparison of diagnostic peritoneal lavage, computed tomographic scanning, and ultrasonography for the diagnosis of blunt abdominal trauma. J Trauma 35(2):267–270
Sosa JL, Baker M, Puente I et al (1995) Negative laparotomy in abdominal gunshot wounds: potential impact of laparoscopy. J Trauma 38(2):194–197
Goodman CS, Hur JY, Adajar MA, Coulam CH (2009) How well does CT predict the need for laparotomy in hemodynamically stable patients with penetrating abdominal injury? A review and meta-analysis. AJR Am J Roentgenol 193(2):432–437
Butela ST, Federle MP, Chang PJ et al (2001) Performance of CT in detection of bowel injury. Am J Roentgenol 176(1):129–135
Panda A, Kumar A, Gamanagatti S et al (2017) Can multidetector CT detect the site of gastrointestinal tract injury in trauma? A retrospective study. Diagn Interv Radiol 23(1):29–36
Ahmad N, Whelan J, Brownlee J et al (2005) The contribution of laparoscopy in evaluation of penetrating abdominal wounds. J Am Coll Surg 201(2):213–216
Fabian TC, Croce MA, Stewart RM et al (1993) A prospective analysis of diagnostic laparoscopy in trauma. Ann Surg 217(5):557–564
Cherry RA, Eachempti SR, Hydo LJ, Barie PS (2005) The role of laparoscopy in penetrating abdominal stab wounds. Surg Laparosc Endosc Percutan Tech 15(1):14–17
Taner AS, Topgul K, Kucukel F et al (2001) Diagnostic laparoscopy decreases the rate of unnecessary laparotomies and reduces hospital costs in trauma patients. J Laparoendosc Adv Surg Tech A 11(4):207–211
Biffl WL, Kaups KL, Cothren CC et al (2009) Management of patients with anterior abdominal stab wounds: a Western Trauma Association multicenter trial. J Trauma 66(5):1294–1301
Morrison JE, Wisner DH, Bodai BI (1996) Complications after negative laparotomy for trauma: long-term follow-up in a health maintenance organization. J Trauma 41(3):509–513
Schnuriger B, Lam L, Inaba K et al (2012) Negative laparotomy in trauma: are we getting better? Am Surg 78(11):1219–1223
Ertekin C, Yanar H, Taviloglu K et al (2005) Unnecessary laparotomy by using physical examination and different diagnostic modalities for penetrating abdominal stab wound. Emerg Med J 22(11):790–794
Rozycki GS, Root HD (2010) The diagnosis of intraabdominal visceral injury. J Trauma 68(5):1019–1023
Matsevych OY, Koto MZ, Aldous C (2018) trauma laparoscopy: a prospect of skills training (cohort study). Int J Surg 55:117–123
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Jonathan Nguyen reports personal fees and non-financial support from Z-Medica, Prytime Medical, and Zimmer Biomet, outside the submitted work. Drs. Deepika Koganti, Benjamin Hazen, Christopher Dente, and Rondi Gelbard have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Koganti, D., Hazen, B.J., Dente, C.J. et al. The role of diagnostic laparoscopy for trauma at a high-volume level one center. Surg Endosc 35, 2667–2670 (2021). https://doi.org/10.1007/s00464-020-07687-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07687-1