Abstract
Background
Acquiring appropriate laparoscopic technique is necessary to safely perform laparoscopic surgery. The Endoscopic Surgical Skill Qualification System of the Japanese Society of Endoscopic Surgery, which was established to improve the quality of laparoscopic surgery in Japan, provides training to become an expert laparoscopic surgeon. In this study, we describe our educational system, in a Japanese highest volume cancer center, and evaluate the system according to the pass rate for the Endoscopic Surgical Skill Qualification System examination.
Methods
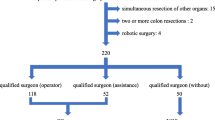
We assessed 14 residents who trained for more than 2 years from 2012 to 2018 in our department. All teaching surgeons, qualified by the Endoscopic Surgical Skill Qualification System, participated in all surgeries as supervisors. For the first 3 months, trainees learned as the scopist, then as the first assistant for 3 months, and then by performing laparoscopic surgery as an operator during ileocecal resection or sigmoidectomy. Trainees apply for this training in their second year of residency or later. All laparoscopic procedures in our department are standardized in detail.
Results
The cumulative pass rate was 75% (12/16), and 87% (12/14) of the trainees eventually passed, while the general pass rate was approximately 30%. On average, those who passed in their second or third year had experienced 94 procedures as the surgeon, 177 as the first assistant, and 199 as the scopist. The number of laparoscopic procedures and the learning curves did not differ between successful and failed applicants.
Conclusions
Through our educational system, residents successfully acquired laparoscopic skills with a much higher pass rate in the Endoscopic Surgical Skill Qualification System examination than the general standard. Laparoscopic practice under supervision by experienced surgeons with standardized procedures and accurate understanding of the relevant anatomy is very helpful to achieving appropriate laparoscopic technique.


Similar content being viewed by others
References
Colon Cancer Laparoscopic or Open Resection Study G, Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52
Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, Heath RM, Brown JM, Group UMCT (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol 25:3061–3068
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, Choi HS, Kim DW, Chang HJ, Kim DY, Jung KH, Kim TY, Kang GH, Chie EK, Kim SY, Sohn DK, Kim DH, Kim JS, Lee HS, Kim JH, Oh JH (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
van der Pas MH, Haglind E, Cuesta MA, Furst A, Lacy AM, Hop WC, Bonjer HJ, Group COcLoORIS (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14:210–218
Mori T, Kimura T, Kitajima M (2010) Skill accreditation system for laparoscopic gastroenterologic surgeons in Japan. Minim Invasive Ther Allied Technol 19:18–23
Aoyama S, Inoue Y, Ohki T, Itabashi M, Yamamoto M (2019) Usefulness of the endoscopic surgical skill qualification system in laparoscopic colorectal surgery: short-term outcomes: a single-center and retrospective analysis. BMC Surg 19:90
Ichikawa N, Homma S, Yoshida T, Ohno Y, Kawamura H, Kamiizumi Y, Iijima H, Taketomi A (2018) Supervision by a technically qualified surgeon affects the proficiency and safety of laparoscopic colectomy performed by novice surgeons. Surg Endosc 32:436–442
Ichikawa N, Homma S, Yoshida T, Ohno Y, Kawamura H, Wakizaka K, Nakanishi K, Kazui K, Iijima H, Shomura H, Funakoshi T, Nakano S, Taketomi A (2017) Mentor tutoring: an efficient method for teaching laparoscopic colorectal surgical skills in a general hospital. Surg Laparosc Endosc Percutan Tech 27:479–484
Japanese Society for Endoscopic surgery. https://www.jses.or.jp/member/gijutsuninteisinsakekka.html
Hospital intelligence agency. https://hospia.jp/dpc
Watanabe T, Muro K, Ajioka Y, Hashiguchi Y, Ito Y, Saito Y, Hamaguchi T, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kawano H, Kinugasa Y, Kokudo N, Murofushi K, Nakajima T, Oka S, Sakai Y, Tsuji A, Uehara K, Ueno H, Yamazaki K, Yoshida M, Yoshino T, Boku N, Fujimori T, Itabashi M, Koinuma N, Morita T, Nishimura G, Sakata Y, Shimada Y, Takahashi K, Tanaka S, Tsuruta O, Yamaguchi T, Yamaguchi N, Tanaka T, Kotake K, Sugihara K, Japanese Society for Cancer of the C, Rectum (2018) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol 23:1–34
Jacobs M, Verdeja JC, Goldstein HS (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1:144–150
Seto Y, Kakeji Y, Miyata H, Iwanaka T (2017) National clinical database (NCD) in Japan for gastroenterological surgery: brief introduction. Ann Gastroenterol Surg 1:80–81
Kapiteijn E, Kranenbarg EK, Steup WH, Taat CW, Rutten HJ, Wiggers T, van Krieken JH, Hermans J, Leer JW, van de Velde CJ (1999) Total mesorectal excision (TME) with or without preoperative radiotherapy in the treatment of primary rectal cancer. Prospective randomised trial with standard operative and histopathological techniques. Dutch ColoRectal Cancer Group. Eur J Surg 165:410–420
Wang C, Gao Z, Shen K, Shen Z, Jiang K, Liang B, Yin M, Yang X, Wang S, Ye Y (2017) Safety, quality and effect of complete mesocolic excision vs non-complete mesocolic excision in patients with colon cancer: a systemic review and meta-analysis. Colorectal Dis 19:962–972
Detering R, Karthaus EG, Borstlap WAA, Marijnen CAM, van de Velde CJH, Bemelman WA, Beets GL, Tanis PJ, Aalbers AGJ, Dutch Snapshot Research G (2019) Treatment and survival of locally recurrent rectal cancer: a cross-sectional population study 15 years after the Dutch TME trial. Eur J Surg Oncol 45:2059–2069
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation–technical notes and outcome. Colorectal Dis 11:354–364 discussion 364-35
Merkel S, Weber K, Matzel KE, Agaimy A, Gohl J, Hohenberger W (2016) Prognosis of patients with colonic carcinoma before, during and after implementation of complete mesocolic excision. Br J Surg 103:1220–1229
Kitano S, Inomata M, Mizusawa J, Katayama H, Watanabe M, Yamamoto S, Ito M, Saito S, Fujii S, Konishi F, Saida Y, Hasegawa H, Akagi T, Sugihara K, Yamaguchi T, Masaki T, Fukunaga Y, Murata K, Okajima M, Moriya Y, Shimada Y (2017) Survival outcomes following laparoscopic versus open D3 dissection for stage II or III colon cancer (JCOG0404): a phase 3, randomised controlled trial. Lancet Gastroenterol Hepatol 2:261–268
Nagasaki T, Akiyoshi T, Fujimoto Y, Konishi T, Nagayama S, Fukunaga Y, Arai M, Ueno M (2015) Prognostic impact of distribution of lymph node metastases in stage III colon cancer. World J Surg 39:3008–3015
Akiyoshi T, Kuroyanagi H, Oya M, Konishi T, Fukuda M, Fujimoto Y, Ueno M, Yamaguchi T, Muto T (2009) Safety of laparoscopic total mesorectal excision for low rectal cancer with preoperative chemoradiation therapy. J Gastrointest Surg 13:521–525
Fujimoto Y, Akiyoshi T, Kuroyanagi H, Konishi T, Ueno M, Oya M, Yamaguchi T (2010) Safety and feasibility of laparoscopic intersphincteric resection for very low rectal cancer. J Gastrointest Surg 14:645–650
Konishi T, Watanabe T, Nagawa H, Oya M, Ueno M, Kuroyanagi H, Fujimoto Y, Akiyoshi T, Yamaguchi T, Muto T (2010) Preoperative chemoradiation and extended pelvic lymphadenectomy for rectal cancer: two distinct principles. World J Gastrointest Surg 2:95–100
Nagasaki T, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Yamaguchi T (2014) Laparoscopic salvage surgery for locally recurrent rectal cancer. J Gastrointest Surg 18:1319–1326
Ogura A, Akiyoshi T, Nagasaki T, Konishi T, Fujimoto Y, Nagayama S, Fukunaga Y, Ueno M, Kuroyanagi H (2017) Feasibility of laparoscopic total mesorectal excision with extended lateral pelvic lymph node dissection for advanced lower rectal cancer after preoperative chemoradiotherapy. World J Surg 41:868–875
Takatsu Y, Fukunaga Y, Nagasaki T, Akiyoshi T, Konishi T, Fujimoto Y, Nagayama S, Ueno M (2017) Short- and long-term outcomes of laparoscopic total mesenteric excision for neuroendocrine tumors of the rectum. Dis Colon Rectum 60:284–289
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242:83–91
Akiyoshi T, Kuroyanagi H, Ueno M, Oya M, Fujimoto Y, Konishi T, Yamaguchi T (2011) Learning curve for standardized laparoscopic surgery for colorectal cancer under supervision: a single-center experience. Surg Endosc 25:1409–1414
Tsai KY, Kiu KT, Huang MT, Wu CH, Chang TC (2016) The learning curve for laparoscopic colectomy in colorectal cancer at a new regional hospital. Asian J Surg 39:34–40
Funding
All authors have no funds specific to this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Ryota Nakanishi, Yosuke Fukunaga, Toshiki Mukai, Toshiya Nagasaki, Tomohiro Yamaguchi, Takashi Akiyoshi, Tsuyoshi Konishi, Satoshi Nagayama, Masashi Ueno have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nakanishi, R., Fukunaga, Y., Mukai, T. et al. Educational system for acquiring appropriate laparoscopic colorectal surgical skills: analysis in a Japanese high-volume cancer center. Surg Endosc 35, 2660–2666 (2021). https://doi.org/10.1007/s00464-020-07686-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07686-2