Abstract
Background
Simulation is widely used to teach and assess fundamental laparoscopic skills; however, program directors have reported that current simulation programs do not meet the needs for trainees and surgeons learning advanced laparoscopic procedures (ALP). The purpose of our study was to identify the key skills required to perform ALP, to serve as the basis to establish an advanced laparoscopic skills training program.
Methods
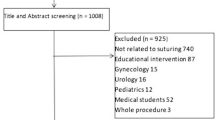
Semi-structured interviews were conducted with attending surgeons, fellows, and senior residents in general surgery, gynaecology, and urology. The questions were developed through an iterative process using relevant literature, expert opinions, and in consultation with a qualitative researcher. Interviews were conducted in person, over the phone, or by videoconference, and inductive thematic analysis was performed.
Results
25 interviews were conducted with 16 attending surgeons and 9 fellows/residents from 9 institutions in Canada and USA. Twenty-one skills were identified to be important when performing ALP. The skills most commonly described by faculty were the following : (a) suturing, (b) dissection, (c) procedural expertise, (d) retraction and exposure, and (e) familiarity with relevant anatomy as viewed through the laparoscope. The skills most commonly described by trainees were the following: (a) suturing, (b) dissection, (c) procedural expertise, (d) trocar positioning, and (e) patient factors. There was a large difference between the importance the faculty attributed to the ‘Retraction and Exposure’ skill compared to the trainees.
Conclusion
This study identified key skills that are important when performing ALP. In order to address the current needs of trainees/surgeons learning ALP, this work provides the building blocks for the development of an advanced laparoscopic surgery simulation program.
Similar content being viewed by others
References
Zendejas B, Hernandez-Irizarry R, Farley DR (2012) Does simulation training improve outcomes in laparoscopic procedures? Adv Surg 46:61–71
Stefanidis D, Sevdalis N, Paige J, Zevin B, Aggarwal R, Grantcharov T, Jones DB (2015) Simulation in surgery: what's needed next? Ann Surg 261:846–853
Scott DJ, Bergen PC, Rege RV, Laycock R, Tesfay ST, Valentine RJ, Euhus DM, Jeyarajah DR, Thompson WM, Jones DB (2000) Laparoscopic training on bench models: better and more cost effective than operating room experience? J Am Coll Surg 191:272–283
Fried GM (2004) Simulators for laparoscopic surgery—a coming of age. Asian J Surg 27:1–3
Kelly WE (1990s) The evolution of laparoscopy and the revolution in surgery in the decade of the 1990s. J Soc Laparoendosc Surg 12:351–357
Rattner DW, Apelgren KN, Eubanks WS (2001) The need for training opportunities in advanced laparoscopic surgery. Surg Endosc 15:1066–1070
Derossis AM, Fried GM, Abrahamowicz M, Sigman HH, Barkun JS, Meakins JL (1998) Development of a model for training and evaluation of laparoscopic skills. Am J Surg 175:482–487
Peters JH, Fried GM, Swanstrom LL, Soper NJ, Sillin LF, Schirmer B, Hoffman K, The SFLSC (2004) Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery 135:21–27
Sroka G, Feldman LS, Vassiliou MC, Kaneva PA, Fayez R, Fried GM (2010) Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room-a randomized controlled trial. Am J Surg 199:115–120
Stefanidis D, Acker C, Heniford BT (2008) Proficiency-based laparoscopic simulator training leads to improved operating room skill that is resistant to decay. Surg Innov 15:69–73
McCluney AL, Vassiliou MC, Kaneva PA, Cao J, Stanbridge DD, Feldman LS, Fried GM (2007) FLS simulator performance predicts intraoperative laparoscopic skill. Surg Endosc 21:1991–1995
Mattar SG, Alseidi AA, Jones DB, Jeyarajah DR, Swanstrom LL, Aye RW, Wexner SD, Martinez JM, Ross SB, Awad MM, Franklin ME, Arregui ME, Schirmer BD, Minter RM (2013) General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg 258:440–449
Nepomnayshy D, Alseidi AA, Fitzgibbons SC, Stefanidis D (2016) Identifying the need for and content of an advanced laparoscopic skills curriculum: results of a national survey. Am J Surg 211:421–425
Bury MR (1986) Social constructionism and the development of medical sociology. Sociol Health Ill 8:137–169
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qual Res Psychol 3:77–101
Nowell LS, Norris JM, White DE, Moules NJ (2017) Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods 16:1–13
Anney VN (2014) Ensuring the quality of the findings of qualitative research: looking at trustworthiness criteria. J Emerg Trends Educ Res Policy Stud 5:272–281
ten Cate O, Scheele F (2007) Competency-based postgraduate training: can we bridge the gap between theory and clinical practice? Acad Med 82:542–547
Touchie C, Ten Cate O (2016) The promise, perils, problems and progress of competency-based medical education. Med Educ 50:93–100
Enani G, Watanabe Y, McKendy KM, Bilgic E, Feldman LS, Fried GM, Vassiliou MC (2017) What are the training gaps for acquiring laparoscopic suturing skills? J Surg Educ 74:656–662
Bilgic E, Watanabe Y, Nepomnayshy D, Gardner A, Fitzgibbons S, Ghaderi I, Alseidi A, Stefanidis D, Paige J, Seymour N, McKendy KM, Birkett R, Whitledge J, Kane E, Anton NE, Vassiliou MC, Simulation Committee of the Association for Surgical E (2016) Multicenter proficiency benchmarks for advanced laparoscopic suturing tasks. Am J Surg 213:217–221
McKendy KM, Watanabe Y, Bilgic E, Enani G, Munshi A, Lee L, Feldman LS, Fried GM, Vassiliou MC (2017) Establishing meaningful benchmarks: the development of a formative feedback tool for advanced laparoscopic suturing. Surg Endosc 31:5057–5065
Watanabe Y, McKendy KM, Bilgic E, Enani G, Madani A, Munshi A, Feldman LS, Fried GM, Vassiliou MC (2016) New models for advanced laparoscopic suturing: taking it to the next level. Surg Endosc 30:581–587
Nepomnayshy D, Whitledge J, Birkett R, Delmonico T, Ruthazer R, Sillin L, Seymour NE (2015) Evaluation of advanced laparoscopic skills tasks for validity evidence. Surg Endosc 29:349–354
Bilgic E, Takao M, Kaneva P, Endo S, Takao T, Watanabe Y, McKendy KM, Feldman LS, Vassiliou MC (2018) Development of a model for the acquisition and assessment of advanced laparoscopic suturing skills using an automated device. Surg Innov 25:286–290
Vassiliou MC, Dunkin BJ, Marks JM, Fried GM (2010) FLS and FES: comprehensive models of training and assessment. Surg Clin N Am 90:535–558
Madani A, Watanabe Y, Vassiliou M, Feldman LS, Duh QY, Singer MC, Ruan DT, Tabah R, Mitmaker E (2016) Defining competencies for safe thyroidectomy: an international Delphi consensus. Surgery 159(86–94):96–101
Bilgic E, Kaneva P, Okrainec A, Ritter EM, Schwaitzberg SD, Vassiliou MC (2017) Trends in the Fundamentals of Laparoscopic Surgery® (FLS) certification exam over the past 9 years. Surg Endosc 32:2101–2105
Green J, Thorogood N (2018) Qualitative methods for health research, 4th edn. SAGE, London
Pucher PH, Brunt LM, Fanelli RD, Asbun HJ, Aggarwal R (2015) SAGES expert Delphi consensus: critical factors for safe surgical practice in laparoscopic cholecystectomy. Surg Endosc 29:3074–3085
Cook DA, Erwin PJ, Triola MM (2010) Computerized virtual patients in health professions education: a systematic review and meta-analysis. Acad Med 85:1589–1602
Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, Erwin PJ, Hamstra SJ (2011) Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA 306:978–988
Acknowledgements
We would like to thank Drs Dmitry Nepomnayshy, Adnan Alseidi, and all of the other members of Advanced Training in Laparoscopic Suturing (ATLAS) subcommittee for their help throughout the study.
Funding
There was no funding or financial support for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The Steinberg-Bernstein Centre receives unrestricted educational grants from Medtronic Canada. All authors report no relevant conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bilgic, E., Hada, T., Dubé, T. et al. Defining the key skills required to perform advanced laparoscopic procedures: a qualitative descriptive study. Surg Endosc 35, 2645–2659 (2021). https://doi.org/10.1007/s00464-020-07685-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07685-3