Abstract
Background
Endoscopic submucosal dissection (ESD) has a favorable outcome, compared to esophagectomy, for early esophageal neoplasia. Recent studies used general anesthesia for esophageal ESD to minimize complications due to insufficient sedation and patient movement. We aimed to evaluate the safety of general anesthesia in comparison with conscious sedation provided by anesthesiologists for esophageal ESD.
Methods
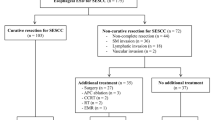
We retrospectively reviewed the electronic medical records of 158 patients who underwent esophageal ESD under general anesthesia or conscious sedation provided by anesthesiologists. We evaluated the incidence of procedure-related complications, including perforation, post-ESD bleeding, cardiopulmonary adverse events (arrhythmia, hypotension, and hypoxemia), procedure failure, stricture, and new lung consolidation after ESD. Cases of frank perforation, post-ESD bleeding requiring a vigorous diagnostic approach, and cardiopulmonary adverse events were regarded as acute complications of ESD.
Results
Acute complications occurred only in the conscious sedation group (8/83 [9.6%] vs. 0/75 [0.0%]; p value = 0.007). The numbers of patients with frank perforation, post-ESD bleeding, and cardiopulmonary adverse events were four, one, and three, respectively. Moreover, new lung consolidation after ESD developed only in the conscious sedation group (7/83 [8.4%] vs. 0/75 [0.0%]; p value = 0.014). ESD failed in four patients in the conscious sedation group. The incidences of stricture that required stent insertion and hospital stay after ESD were comparable between the two groups.
Conclusion
General anesthesia is associated with a lower incidence of acute procedure-related complications in esophageal ESD compared to conscious sedation provided by anesthesiologists. Therefore, we recommend general anesthesia as a safer option for esophageal ESD.

Similar content being viewed by others
References
Dimick JB, Wainess RM, Upchurch GR Jr, Iannettoni MD, Orringer MB (2005) National trends in outcomes for esophageal resection. Ann Thorac Surg 79:212–216
Ra J, Paulson EC, Kucharczuk J, Armstrong K, Wirtalla C, Rapaport-Kelz R, Kaiser LR, Spitz FR (2008) Postoperative mortality after esophagectomy for cancer: development of a preoperative risk prediction model. Ann Surg Oncol 15:1577–1584
Markar SR, Karthikesalingam A, Thrumurthy S, Low DE (2012) Volume-outcome relationship in surgery for esophageal malignancy: systematic review and meta-analysis 2000–2011. J Gastrointest Surg 16:1055–1063
Isono K, Sato H, Nakayama K (1991) Results of a nationwide study on the three-field lymph node dissection of esophageal cancer. Oncology 48:411–420
Takahashi H, Arimura Y, Masao H, Okahara S, Tanuma T, Kodaira J, Kagaya H, Shimizu Y, Hokari K, Tsukagoshi H, Shinomura Y, Fujita M (2010) Endoscopic submucosal dissection is superior to conventional endoscopic resection as a curative treatment for early squamous cell carcinoma of the esophagus (with video). Gastrointest Endosc 72:255–264
Malik S, Sharma G, Sanaka MR, Thota PN (2018) Role of endoscopic therapy in early esophageal cancer. World J Gastroenterol 24:3965–3973
Nishizawa T, Yahagi N (2017) Endoscopic mucosal resection and endoscopic submucosal dissection: technique and new directions. Curr Opin Gastroenterol 33:315–319
Cho JW, Choi SC, Jang JY, Shin SK, Choi KD, Lee JH, Kim SG, Sung JK, Jeon SW, Choi IJ, Kim GH, Jee SR, Lee WS, Jung HY (2014) Lymph node metastases in esophageal carcinoma: an endoscopist's view. Clin Endosc 47:523–529
Triantafillidis JK, Merikas E, Nikolakis D, Papalois AE (2013) Sedation in gastrointestinal endoscopy: current issues. World J Gastroenterol 19:463–481
Park CH, Min JH, Yoo YC, Kim H, Joh DH, Jo JH, Shin S, Lee H, Park JC, Shin SK, Lee YC, Lee SK (2013) Sedation methods can determine performance of endoscopic submucosal dissection in patients with gastric neoplasia. Surg Endosc 27:2760–2767
Yamagata T, Hirasawa D, Fujita N, Suzuki T, Obana T, Sugawara T, Ohira T, Harada Y, Maeda Y, Koike Y, Suzuki K, Noda Y (2011) Efficacy of propofol sedation for endoscopic submucosal dissection (ESD): assessment with prospective data collection. Intern Med 50:1455–1460
Choi IJ, Lee NR, Kim SG, Lee WS, Park SJ, Kim JJ, Lee JH, Kwon JW, Park SH, You JH, Kim JH, Lim CH, Cho JY, Kim GH, Lee YC, Jung HY, Kim JY, Chun HJ, Seol SY (2016) Short-term outcomes of endoscopic submucosal dissection in patients with early gastric cancer: a prospective multicenter cohort study. Gut Liver 10:739–748
Pyo JH, Lee H, Min BH, Lee JH, Choi MG, Lee JH, Sohn TS, Bae JM, Kim KM, Ahn JH, Carriere KC, Kim JJ, Kim S (2016) Long-term outcome of endoscopic resection vs. surgery for early gastric cancer: a non-inferiority-matched cohort study. Am J Gastroenterol 111:240–249
Isomoto H, Yamaguchi N, Minami H, Nakao K (2013) Management of complications associated with endoscopic submucosal dissection/ endoscopic mucosal resection for esophageal cancer. Dig Endosc 25:29–38
Tsujii Y, Nishida T, Nishiyama O, Yamamoto K, Kawai N, Yamaguchi S, Yamada T, Yoshio T, Kitamura S, Nakamura T, Nishihara A, Ogiyama H, Nakahara M, Komori M, Kato M, Hayashi Y, Shinzaki S, Iijima H, Michida T, Tsujii M, Takehara T (2015) Clinical outcomes of endoscopic submucosal dissection for superficial esophageal neoplasms: a multicenter retrospective cohort study. Endoscopy 47:775–783
Park HC, Kim DH, Gong EJ, Na HK, Ahn JY, Lee JH, Jung KW, Choi KD, Song HJ, Lee GH, Jung HY, Kim JH (2016) Ten-year experience of esophageal endoscopic submucosal dissection of superficial esophageal neoplasms in a single center. Korean J Intern Med 31:1064–1072
Kim GH, Jee SR, Jang JY, Shin SK, Choi KD, Lee JH, Kim SG, Sung JK, Choi SC, Jeon SW, Jang BI, Huh KC, Chang DK, Jung SA, Keum B, Cho JW, Choi IJ, Jung HY (2014) Stricture occurring after endoscopic submucosal dissection for esophageal and gastric tumors. Clin Endosc 47:516–522
Yagi Kuwata N, Gotoda T, Suzuki S, Mukai S, Itoi T, Moriyasu F (2016) Reasonable decision of anesthesia methods in patients who underwent endoscopic submucosal dissection for superficial esophageal carcinoma: A retrospective analysis in a single Japanese institution. Turk J Gastroenterol 27:91–96
Yamashita K, Shiwaku H, Ohmiya T, Shimaoka H, Okada H, Nakashima R, Beppu R, Kato D, Sasaki T, Hoshino S, Nimura S, Yamaura K, Yamashita Y (2016) Efficacy and safety of endoscopic submucosal dissection under general anesthesia. World J Gastrointest Endosc 8:466–471
Song BG, Min YW, Cha RR, Lee H, Min BH, Lee JH, Rhee PL, Kim JJ (2018) Endoscopic submucosal dissection under general anesthesia for superficial esophageal squamous cell carcinoma is associated with better clinical outcomes. BMC Gastroenterol 18:80
Berry MF (2014) Esophageal cancer: staging system and guidelines for staging and treatment. J Thorac Dis 6:S289–297
Ning B, Abdelfatah MM, Othman MO (2017) Endoscopic submucosal dissection and endoscopic mucosal resection for early stage esophageal cancer. Ann Cardiothorac Surg 6:88–98
Kataoka Y, Tsuji Y, Sakaguchi Y, Minatsuki C, Asada-Hirayama I, Niimi K, Ono S, Kodashima S, Yamamichi N, Fujishiro M, Koike K (2016) Bleeding after endoscopic submucosal dissection: risk factors and preventive methods. World J Gastroenterol 22:5927–5935
Libanio D, Costa MN, Pimentel-Nunes P, Dinis-Ribeiro M (2016) Risk factors for bleeding after gastric endoscopic submucosal dissection: a systematic review and meta-analysis. Gastrointest Endosc 84:572–586
Guo HM, Zhang XQ, Chen M, Huang SL, Zou XP (2014) Endoscopic submucosal dissection vs endoscopic mucosal resection for superficial esophageal cancer. World J Gastroenterol 20:5540–5547
Aadam AA, Abe S (2018) Endoscopic submucosal dissection for superficial esophageal cancer. Dis Esophagus 1:31
Fujita R, Kumura F (1975) Arrythmias and ischemic changes of the heart induced by gastric endoscopic procedures. Am J Gastroenterol 64:44–48
Yazawa K, Adachi W, Koide N, Watanabe H, Koike S, Hanazaki K (2000) Changes in cardiopulmonary parameters during upper gastrointestinal endoscopy in patients with heart disease: towards safer endoscopy. Endoscopy 32:287–293
Rosenberg J, Jorgensen LN, Rasmussen V, Vibits H, Hansen PE (1992) Hypoxaemia and myocardial ischaemia during and after endoscopic cholangiopancreatography: call for further studies. Scand J Gastroenterol 27:717–720
McAlpine JK, Martin BJ, Devine BL (1990) Cardiac arrhythmias associated with upper gastrointestinal endoscopy in elderly subjects. Scott Med J 35:102–104
Park CH, Shin S, Lee SK, Lee H, Lee YC, Park JC, Yoo YC (2015) Assessing the stability and safety of procedure during endoscopic submucosal dissection according to sedation methods: a randomized trial. PLoS ONE 10:e0120529
Allen ML (2017) Safety of deep sedation in the endoscopy suite. Curr Opin Anaesthesiol 30:501–506
Abe K, Tominaga K, Kanamori A, Suzuki T, Kino H, Nakano M, Sugaya T, Tsuchida K, Majima Y, Murohisa T, Iijima M, Goda K, Irisawa A (2019) Safety and efficacy of nonanesthesiologist-administrated propofol during endoscopic submucosal dissection of gastric epithelial tumors. Gastroenterol Res Pract 2019:5937426
Cho YS, Shin SY, Hwang C, Seo J, Choi JW, Park BK, Won SY, Lee CK, Lee YK, Jeon HH (2017) Safety and effectiveness of endoscopist-directed nurse-administered sedation during gastric endoscopic submucosal dissection. Gastroenterol Res Pract 2017:4723626
Rex DK, Deenadayalu VP, Eid E, Imperiale TF, Walker JA, Sandhu K, Clarke AC, Hillman LC, Horiuchi A, Cohen LB, Heuss LT, Peter S, Beglinger C, Sinnott JA, Welton T, Rofail M, Subei I, Sleven R, Jordan P, Goff J, Gerstenberger PD, Munnings H, Tagle M, Sipe BW, Wehrmann T, Di Palma JA, Occhipinti KE, Barbi E, Riphaus A, Amann ST, Tohda G, McClellan T, Thueson C, Morse J, Meah N (2009) Endoscopist-directed administration of propofol: a worldwide safety experience. Gastroenterology 137:1229–1237
Calderwood AH, Chapman FJ, Cohen J, Cohen LB, Collins J, Day LW, Early DS (2014) Guidelines for safety in the gastrointestinal endoscopy unit. Gastrointest Endosc 79:363–372
Dumonceau JM, Riphaus A, Schreiber F, Vilmann P, Beilenhoff U, Aparicio JR, Vargo JJ, Manolaraki M, Wientjes C, Racz I, Hassan C, Paspatis G (2015) Non-anesthesiologist administration of propofol for gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates Guideline-Updated June 2015. Endoscopy 47:1175–1189
Obara K, Haruma K, Irisawa A, Kaise M, Gotoda T, Sugiyama M, Tanabe S, Horiuchi A, Fujita N, Ozaki M, Yoshida M, Matsui T, Ichinose M, Kaminishi M (2015) Guidelines for sedation in gastroenterological endoscopy. Dig Endosc 27:435–449
Kobayashi S, Kanai N, Ohki T, Takagi R, Yamaguchi N, Isomoto H, Kasai Y, Hosoi T, Nakao K, Eguchi S, Yamamoto M, Yamato M, Okano T (2014) Prevention of esophageal strictures after endoscopic submucosal dissection. World J Gastroenterol 20:15098–15109
Ono S, Fujishiro M, Niimi K, Goto O, Kodashima S, Yamamichi N, Omata M (2009) Predictors of postoperative stricture after esophageal endoscopic submucosal dissection for superficial squamous cell neoplasms. Endoscopy 41:661–665
Author information
Authors and Affiliations
Contributions
SHK designed the research, collected and analyzed the data, and wrote the manuscript; YSC, SKL, and HO collected and analyzed the data, and wrote the manuscript; SHC designed the research, collected and analyzed the data, and wrote the manuscript; all authors reviewed the manuscript prior to its submission, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Disclosures
Drs. Seung Hyun Kim, Yong Seon Choi, Sang Kil Lee, Hanseul Oh, and Seung Ho Choi have no conflicts of interest or financial ties to disclose.
Institutional review board statement
The study protocol was approved by the Institutional Review Board of the Yonsei University Health System, Seoul, South Korea.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, S.H., Choi, Y.S., Lee, S.K. et al. Comparison of general anesthesia and conscious sedation in procedure-related complications during esophageal endoscopic submucosal dissection. Surg Endosc 34, 3560–3566 (2020). https://doi.org/10.1007/s00464-020-07663-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07663-9