Abstract
Background
The short-term results of single-incision laparoscopic colectomy (SILC) showed the safety, feasibility, and effectiveness when performed by skilled laparoscopic surgeons. However, the long-term complications, such as SILC-associated incisional hernia, have not been evaluated. The aim of this study was to determine the incidence of incisional hernia after SILC compared with multi-port laparoscopic colectomy (MPC) for colon cancer.
Methods
From March 2012, to March 2015, a total of 200 patients were enrolled in this study. The patients were randomized to the MPC arm and SILC arm. A total of 200 patients (MPC arm; 100 patients, SILC arm; 100 patients) were therefore analyzed. In all cases the specimen was extracted through the umbilical port, which was extended according to the size of the specimen. A diagnosis of incisional hernia was made either based on a physical examination or computed tomography.
Results
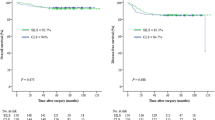
The baseline factors were well balanced between the arms. The median follow-up period was 42.4 (range 9.4–70.0) months. Twenty-one patients were diagnosed with incisional hernia, giving an incidence rate of 12.1% in the MPC arm and 9.0% in the SILC arm at 36 months (P = 0.451). In the multivariate analysis, the body mass index (≥ 25 kg/m2) (hazard ratio [HR] 3.03; 95% confidence interval [CI] 1.03–8.92; P = 0.044), umbilical incision (≥ 5.0 cm) (HR 3.22; 95% CI 1.16–8.93; P = 0.025), and history of umbilical hernia (HR 3.16; 95% CI 1.02–9.77; P = 0.045) were shown to be correlated with incisional hernia.
Conclusions
We found no significant difference in the incidence of incisional hernia after SILC arm versus MPC arm with a long-term follow-up. However, this result may be biased because all specimens were harvested through the umbilical port.
The study was registered with the Japanese Clinical Trials Registry as UMIN000007220.


Similar content being viewed by others
References
Champagne BJ, Lee EC, Leblanc F, Stein SL, Delaney CP (2011) Single-incision vs straight laparoscopic segmental colectomy: a case-controlled study. Dis Colon Rectum 54:183–186
Chen WT, Chang SC, Chiang HC et al (2011) Single-incision laparoscopic versus conventional laparoscopic right hemicolectomy: a comparison of short-term surgical results. Surg Endosc 25:1887–1892
Kim SJ, Ryu GO, Choi BJ et al (2011) The short-term outcomes of conventional and single-port laparoscopic surgery for colorectal cancer. Ann Surg 254:933–940
Papaconstantinou HT, Thomas JS (2011) Single-incision laparoscopic colectomy for cancer: assessment of oncologic resection and short-term outcomes in a case-matched comparison with standard laparoscopy. Surgery 150:820–827
Champagne BJ, Papaconstantinou HT, Parmar SS et al (2012) Single-incision versus standard multiport laparoscopic colectomy: a multicenter, case-controlled comparison. Ann Surg 255:66–69
Lu CC, Lin SE, Chung KC, Rau KM (2012) Comparison of clinical outcome of single-incision laparoscopic surgery using a simplified access system with conventional laparoscopic surgery for malignant colorectal disease. Colorectal Dis 14:e171–e176
Ramos-Valadez DI, Ragupathi M, Nieto J et al (2012) Single-incision versus conventional laparoscopic sigmoid colectomy: a case-matched series. Surg Endosc 26:96–102
Velthuis S, van den Boezem PB, Lips DJ, Prins HA, Cuesta MA, Sietses C (2012) Comparison of short-term surgical outcomes after single-incision laparoscopic versus multiport laparoscopic right colectomy: a two-center, prospective case-controlled study of 100 patients. Dig Surg 29:477–483
Takemasa I, Uemura M, Nishimura J et al (2014) Feasibility of single-site laparoscopic colectomy with complete mesocolic excision for colon cancer: a prospective case-control comparison. Surg Endosc 28:1110–1118
Katsuno G, Fukunaga M, Nagakari K, Yoshikawa S, Azuma D, Kohama S (2015) Short-term and long-term outcomes of single-incision versus multi-incision laparoscopic resection for colorectal cancer: a propensity-score-matched analysis of 214 cases. Surg Endosc 30:1317–1325
Kim CW, Cho MS, Baek SJ et al (2015) Oncologic outcomes of single-incision versus conventional laparoscopic anterior resection for sigmoid colon cancer: a propensity-score matching analysis. Ann Surg Oncol 22:924–930
Suzuki O, Nakamura F, Kashimura N, Nakamura T, Takada M, Ambo Y (2015) A case-matched comparison of single-incision versus multiport laparoscopic right colectomy for colon cancer. Surg Today 46:297–302
Watanabe J, Ota M, Fujii S, Suwa H, Ishibe A, Endo I (2016) Randomized clinical trial of single-incision versus multiport laparoscopic colectomy. Br J Surg 103:1276–1281
Kang BM, Kim HJ, Kye BH et al (2018) Multicenter, randomized single-port versus multiport laparoscopic surgery (SIMPLE) trial in colon cancer: an interim analysis. Surg Endosc 32:1540–1549
Maggiori L, Tuech JJ, Cotte E et al (2018) Single-incision laparoscopy versus multiport laparoscopy for colonic surgery: a multicenter, double-blinded, randomized controlled trial. Ann Surg 268:740–746
Yang TX, Chua TC (2013) Single-incision laparoscopic colectomy versus conventional multiport laparoscopic colectomy: a meta-analysis of comparative studies. Int J Colorectal Dis 28:89–101
Lujan JA, Soriano MT, Abrisqueta J, Perez D, Parrilla P (2015) Single-port colectomy VS multi-port laparoscopic colectomy. systematic review and meta-analysis of more than 2800 procedures. Cir Esp 93:307–319
Hoyuela C, Juvany M, Carvajal F (2017) Single-incision laparoscopy versus standard laparoscopy for colorectal surgery: a systematic review and meta-analysis. Am J Surg 214:127–140
Levic K, Bulut O (2018) Single-incision laparoscopy versus standard laparoscopy for colorectal surgery: a systematic review and meta-analysis. Am J Surg 216:1233
Alptekin H, Yilmaz H, Acar F, Kafali ME, Sahin M (2012) Incisional hernia rate may increase after single-port cholecystectomy. J Laparoendosc Adv Surg Tech A 22:731–737
Marks JM, Phillips MS, Tacchino R et al (2013) Single-incision laparoscopic cholecystectomy is associated with improved cosmesis scoring at the cost of significantly higher hernia rates: 1-year results of a prospective randomized, multicenter, single-blinded trial of traditional multiport laparoscopic cholecystectomy vs single-incision laparoscopic cholecystectomy. J Am Coll Surg 216:1037–1047 discussion 47–48
Sangster W, Kulaylat AN, Stewart DB, Schubart JR, Koltun WA, Messaris E (2015) Hernia incidence following single-site vs standard laparoscopic colorectal surgery. Colorectal Dis 17:250–256
Sobin LH, Gospodarowicz MK, Wittekind C (2010) International Union against Cancer. TNM classification of malignant tumours, 7th edn. Wiley-Blackwell, Chichester, West Sussex, Hoboken
Antoniou SA, Garcia-Alamino JM, Hajibandeh S et al (2018) Single-incision surgery trocar-site hernia: an updated systematic review meta-analysis with trial sequential analysis by the Minimally Invasive Surgery Synthesis of Interventions Outcomes Network (MISSION). Surg Endosc 32:14–23
Lee L, Mata J, Droeser RA et al (2018) Incisional hernia after midline versus transverse specimen extraction incision: a randomized trial in patients undergoing laparoscopic colectomy. Ann Surg 268:41–47
Lee L, Abou-Khalil M, Liberman S, Boutros M, Fried GM, Feldman LS (2017) Incidence of incisional hernia in the specimen extraction site for laparoscopic colorectal surgery: systematic review and meta-analysis. Surg Endosc 31:5083–5093
Flum DR, Horvath K, Koepsell T (2003) Have outcomes of incisional hernia repair improved with time? A population-based analysis. Ann Surg 237:129–135
Fink C, Baumann P, Wente MN et al (2014) Incisional hernia rate 3 years after midline laparotomy. Br J Surg 101:51–54
Soderback H, Gunnarsson U, Hellman P, Sandblom G (2018) Incisional hernia after surgery for colorectal cancer: a population-based register study. Int J Colorectal Dis 33:1411–1417
Bartels SA, Vlug MS, Hollmann MW et al (2014) Small bowel obstruction, incisional hernia and survival after laparoscopic and open colonic resection (LAFA study). Br J Surg 101:1153–1159
Sadava EE, Kerman Cabo J, Carballo FH, Bun ME, Rotholtz NA (2014) Incisional hernia after laparoscopic colorectal surgery Is there any factor associated? Surg Endosc 28:3421–3424
Jensen KK, Krarup PM, Scheike T, Jorgensen LN, Mynster T (2016) Incisional hernias after open versus laparoscopic surgery for colonic cancer: a nationwide cohort study. Surg Endosc 30:4469–4479
Laurent C, Leblanc F, Bretagnol F, Capdepont M, Rullier E (2008) Long-term wound advantages of the laparoscopic approach in rectal cancer. Br J Surg 95:903–908
Aquina CT, Rickles AS, Probst CP et al (2015) Visceral obesity, not elevated BMI, is strongly associated with incisional hernia after colorectal surgery. Dis Colon Rectum 58:220–227
Bellon JM, Bajo A, Ga-Honduvilla N et al (2001) Fibroblasts from the transversalis fascia of young patients with direct inguinal hernias show constitutive MMP-2 overexpression. Ann Surg 233:287–291
Fachinelli A, Maciel Trindade MR (2007) Qualitative and quantitative evaluation of total and types I and III collagens in patients with ventral hernias. Langenbecks Arch Surg 392:459–464
Zoller B, Ji J, Sundquist J, Sundquist K (2013) Shared and nonshared familial susceptibility to surgically treated inguinal hernia, femoral hernia, incisional hernia, epigastric hernia, and umbilical hernia. J Am Coll Surg 217:289–299
Funding
Grant support for the research reported: None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Jun Watanabe, Atsushi Ishibe, Yusuke Suwa, Hirokazu Suwa, Mitsuyoshi Ota, Kazumi Kubota, Takeharu Yamanaka, Chikara Kunisaki and Itaru Endo have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Watanabe, J., Ishibe, A., Suwa, Y. et al. Hernia incidence following a randomized clinical trial of single-incision versus multi-port laparoscopic colectomy. Surg Endosc 35, 2465–2472 (2021). https://doi.org/10.1007/s00464-020-07656-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07656-8