Abstract
Introduction
Assessment of regional lymph nodes (LN) is essential for determining prognosis among patients with gallbladder cancer (GBC). The impact of surgical technique on LN yield has not been well explored. We investigated the impact of minimally invasive surgery (MIS; robotic or laparoscopic) on the evaluation and retrieval of regional LN for patients with GBC.
Methods
We queried the National Cancer Database (NCDB) to identify patients with GBC who underwent curative-intent surgery between 2010 and 2015. Patients with metastatic disease or those with missing data on surgical resection or LN evaluation were excluded.
Results
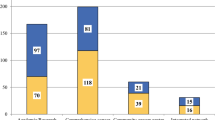
We identified 2014 patients who underwent an open (n = 1141, 56.6%) or MIS approach (n = 873, 43.4%) for GBC and met the inclusion criteria. Patients who underwent MIS were older (open: 68 years, IQR: 60, 75 vs. MIS: 70 years, IQR (61, 77); P = 0.02), and were more commonly treated at a comprehensive community cancer program (P < 0.001). Approximately 3 out of 4 patients (n = 1468, 72.9%) underwent an evaluation of regional LN, with nearly half of these patients (n = 607, 41.7%) having LN metastasis. Among patients who underwent a regional lymphadenectomy, average lymph node yield was 3 (IQR: 1, 6) and was similar between the two groups (P = 0.04). After controlling for all factors, operative approach was not associated with likelihood of receiving a lymphadenectomy during curative-intent resection (OR 0.81, 95% CI 0.63–1.04; P = 0.11).
Conclusion
In conclusion, patients undergoing curative-intent resection for GBC had similar rates of lymph node evaluation and yield regardless of operative approach. Over one-quarter of patients did not undergo a lymphadenectomy at the time of surgery. Further studies are needed to identify barriers to lymph node evaluation and yield among patients undergoing surgery for gallbladder cancer. Presented at the 2019 2nd World Congress of the International Laparoscopic Liver Society, Tokyo, Japan

Similar content being viewed by others
References
Lazcano-Ponce EC, Miquel JF, Munoz N et al (2001) Epidemiology and molecular pathology of gallbladder cancer. CA Cancer J Clin. https://doi.org/10.3322/canjclin.51.6.349
Hundal R, Shaffer EA (2014) Gallbladder cancer: epidemiology and outcome. Clin Epidemiol. https://doi.org/10.2147/CLEP.S37357
Buettner S, Margonis GA, Kim Y et al (2016) Changing odds of survival over time among patients undergoing surgical resection of gallbladder carcinoma. Ann Surg Oncol. https://doi.org/10.1245/s10434-016-5470-2
Tsilimigras DI, Hyer JM, Paredes AZ et al (2019) The optimal number of lymph nodes to evaluate among patients undergoing surgery for gallbladder cancer: correlating the number of nodes removed with survival in 6531 patients. J Surg Oncol. https://doi.org/10.1002/jso.25450
Amini N, Spolverato G, Kim Y et al (2015) Lymph node status after resection for gallbladder adenocarcinoma: prognostic implications of different nodal staging/scoring systems. J Surg Oncol. https://doi.org/10.1002/jso.23813
Amini N, Kim Y, Wilson A et al (2016) Prognostic implications of lymph node status for patients with gallbladder cancer: a multi-institutional study. Ann Surg Oncol. https://doi.org/10.1245/s10434-016-5243-y
Tran TB, Nissen NN (2015) Surgery for gallbladder cancer in the US: a need for greater lymph node clearance. J Gastrointest Oncol. https://doi.org/10.3978/j.issn.2078-6891.2015.062
Dixon E, Vollmer CM, Sahajpal A et al (2005) An aggressive surgical approach leads to improved survival in patients with gallbladder cancer: a 12-year study at a North American Center. Ann Surg. https://doi.org/10.1097/01.sla.0000154118.07704.ef
Ejaz A, Sachs T, He J et al (2014) A comparison of open and minimally invasive surgery for hepatic and pancreatic resections using the nationwide inpatient sample. Surgery. https://doi.org/10.1016/j.surg.2014.03.046
Vega EA, Sanhueza M, Viñuela E (2019) Minimally invasive surgery for gallbladder cancer. Surg Oncol Clin N Am. https://doi.org/10.1016/j.soc.2018.11.001
Boffa DJ, Rosen JE, Mallin K et al (2017) Using the national cancer database for outcomes research a review. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2016.6905
Feng JW, Yang XH, Liu CW et al (2019) Comparison of laparoscopic and open approach in treating gallbladder cancer. J Surg Res. https://doi.org/10.1016/j.jss.2018.09.025
Mayo SC, Shore AD, Nathan H et al (2010) National trends in the management and survival of surgically managed gallbladder adenocarcinoma over 15 years: a population-based analysis. J Gastrointest Surg. https://doi.org/10.1007/s11605-010-1335-3
Nag HH, Raj P, Sisodia K (2018) The technique of laparoscopic hepatic bisegmentectomy with regional lymphadenectomy for gallbladder cancer. J Minim Access Surg. https://doi.org/10.4103/jmas.JMAS_181_16
Tam V, Borrebach J, Dunn SA, Bellon J, Zeh HJ, Hogg ME (2019) Proficiency-based training and credentialing can improve patients outcomes and decrease cost to a hospital system. Am J Surg. https://doi.org/10.1016/j.amjsurg.2018.07.053
Fretland AA, Dagenborg VJ, Bjørnelv GMW et al (2018) Laparoscopic versus open resection for colorectal liver metastases. Ann Surg. https://doi.org/10.1097/SLA.0000000000002353
Hilal MA, Aldrighetti L, Dagher I et al (2018) The Southampton Consensus Guidelines for laparoscopic liver surgery: from indication to implementation. Ann Surg. https://doi.org/10.1097/SLA.0000000000002524
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Ahmad Hamad, Jordan Cloyd, Mary Dillhoff, Andrei Manilchuk, Timothy Pawlik, Allan Tsung and Aslam Ejaz have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hamad, A., Cloyd, J.M., Dillhoff, M. et al. Comparison of lymph node evaluation and yield among patients undergoing open and minimally invasive surgery for gallbladder adenocarcinoma. Surg Endosc 35, 2223–2228 (2021). https://doi.org/10.1007/s00464-020-07635-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07635-z