Abstract
Background
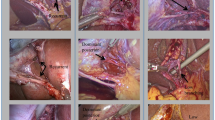
Based on the spatial relationship of an aberrant right hepatic duct (ARHD) with the cystic duct and gallbladder neck, we propose a practical classification to evaluate the specific form predisposing to injury in laparoscopic cholecystectomy (LC).
Methods
We retrospectively investigated the preoperative images (mostly magnetic resonance cholangiopancreatography) and clinical outcomes of 721 consecutive patients who underwent LC at our institute from 2015 to 2018. We defined the high-risk ARHD as follows: Type A: communicating with the cystic duct and Type B: running along the gallbladder neck or adjacent to the infundibulum (the minimal distance from the ARHD < 5 mm), regardless of the confluence pattern in the biliary tree. Other ARHDs were considered to be of low risk.
Results
A high-risk ARHD was identified in 16 cases (2.2%): four (0.6%) with Type A anatomy and 12 (1.7%) with Type B. The remaining ARHD cases (n = 34, 4.7%) were categorized as low risk. There were no significant differences in the operative outcomes (operative time, blood loss, hospital stay) between the high- and low- risk groups. Subtotal cholecystectomy was applied in four cases (25%) in the high-risk group, a significantly higher percentage than the low-risk group (n = 1, 2.9%). In all patients with high-risk ARHD, LC was completed safely without bile duct injury or conversion to laparotomy.
Conclusions
Our simple classification of high-risk ARHD can highlight the variants located close to the dissecting site to achieve a critical view of safety and may contribute to avoiding inadvertent damage of an ARHD in LC.





Similar content being viewed by others
References
Chung YH, Kim DJ, Kim IG, Kim HJ, Chon SE, Jeon JY, Jung JP, Jeong JC, Kim JS, Yun EJ (2012) Relationship between the risk of bile duct injury during laparoscopic cholecystectomy and the types of preoperative magnetic resonance cholangiopancreatiocography (MRCP). Korean J Hepatobiliary Pancreat Surg 16:17–23
Noji T, Nakamura F, Nakamura T, Kato K, Suzuki O, Ambo Y, Kishida A, Maguchi H, Kondo S, Kashimura N (2011) ENBD tube placement prior to laparoscopic cholecystectomy may reduce the rate of complications in cases with predictably complicating biliary anomalies. J Gastroenterol 46:73–77
Suhocki PV, Meyers WC (1999) Injury to aberrant bile ducts during cholecystectomy: a common cause of diagnostic error and treatment delay. AJR Am J Roentgenol 172:955–959
Kurata M, Honda G, Okuda Y, Kobayashi S, Sakamoto K, Iwasaki S, Chiba K, Tabata T, Kuruma S, Kamisawa T (2015) Preoperative detection and handling of aberrant right posterior sectoral hepatic duct during laparoscopic cholecystectomy. J Hepatobiliary Pancreat Sci 22:558–562
Ohkubo M, Nagino M, Kamiya J, Yuasa N, Oda K, Arai T, Nishio H, Nimura Y (2004) Surgical anatomy of the bile ducts at the hepatic hilum as applied to living donor liver transplantation. Ann Surg 239:82–86
Onder H, Ozdemir MS, Tekbas G, Ekici F, Gumus H, Bilici A (2013) 3-T MRI of the biliary tract variations. Surg Radiol Anat 35:161–167
Ausch C, Hochwarter G, Taher M, Holzer B, Rosen HR, Urban M, Sebesta C, Hruby W, Schiessel R (2005) Improving the safety of laparoscopic cholecystectomy: the routine use of preoperative magnetic resonance cholangiography. Surg Endosc 19:574–580
Chaib E, Kanas AF, Galvao FH, D'Albuquerque LA (2014) Bile duct confluence: anatomic variations and its classification. Surg Radiol Anat 36:105–109
Hirano Y, Tatsuzawa Y, Shimizu J, Kinoshita S, Kawaura Y, Takahashi S (2006) Efficacy of multi-slice computed tomography cholangiography before laparoscopic cholecystectomy. ANZ J Surg 76:693–695
Hirao K, Miyazaki A, Fujimoto T, Isomoto I, Hayashi K (2000) Evaluation of aberrant bile ducts before laparoscopic cholecystectomy: helical CT cholangiography versus MR cholangiography. AJR Am J Roentgenol 175:713–720
Ishii H, Noguchi A, Fukami T, Sugimoto R, Tada H, Takeshita H, Umehara S, Izumi H, Tani N, Yamaguchi M, Yamane T (2017) Preoperative evaluation of accessory hepatic ducts by drip infusion cholangiography with CT. BMC Surg 17:52
Karakas HM, Celik T, Alicioglu B (2008) Bile duct anatomy of the Anatolian Caucasian population: Huang classification revisited. Surg Radiol Anat 30:539–545
Ochiai T, Yamazaki S, Ohta K, Takahashi M, Iwai T, Irie T, Noguchi N, Takamatsu S, Kawamura T, Teramoto K, Arii S (2004) Is drip infusion cholecystocholangiography (DIC) an acceptable modality at cholecystectomy for cholecystolithiasis, considering the frequency of bile duct maljunction and intraoperative bile duct injury? J Hepatobiliary Pancreat Surg 11:135–139
Uchiyama K, Tani M, Kawai M, Ueno M, Hama T, Yamaue H (2006) Preoperative evaluation of the extrahepatic bile duct structure for laparoscopic cholecystectomy. Surg Endosc 20:1119–1123
Larobina M, Nottle PD (2005) Extrahepatic biliary anatomy at laparoscopic cholecystectomy: is aberrant anatomy important? ANZ J Surg 75:392–395
Strasberg SM, Brunt LM (2010) Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg 211:132–138
Strasberg SM, Brunt LM (2017) The critical view of safety: why it is not the only method of ductal identification within the standard of care in laparoscopic cholecystectomy. Ann Surg 265:464–465
Tatsuaki S, Yasuo S, Takehiro O, Yasuhiro H, Yoshihiro N, Michihiko K, Kenta S, Yuji N, Taijiro S (2017) Multidetector CT in detection of troublesome posterior sectoral hepatic duct communicating with cystic duct. Br J Radiol 90:20170260
Matsumura T, Komatsu S, Komaya K, Ando K, Arikawa T, Ishiguro S, Saito T, Osawa T, Kurahashi S, Uchino T, Yasui K, Kato S, Suzuki K, Kato Y, Sano T (2018) Closure of the cystic duct orifice in laparoscopic subtotal cholecystectomy for severe cholecystitis. Asian J Endosc Surg 11:206–211
Honda G, Iwanaga T, Kurata M, Watanabe F, Satoh H, Iwasaki K (2009) The critical view of safety in laparoscopic cholecystectomy is optimized by exposing the inner layer of the subserosal layer. J Hepatobiliary Pancreat Surg 16:445–449
Elshaer M, Gravante G, Thomas K, Sorge R, Al-Hamali S, Ebdewi H (2015) Subtotal cholecystectomy for "difficult gallbladders": systematic review and meta-analysis. JAMA Surg 150:159–168
Shingu Y, Komatsu S, Norimizu S, Taguchi Y, Sakamoto E (2016) Laparoscopic subtotal cholecystectomy for severe cholecystitis. Surg Endosc 30:526–531
Li JH, Zheng CZ, Ke CW, Yin K (2002) Management of aberrant bile duct during laparoscopic cholecystectomy. Hepatobiliary Pancreat Dis Int 1:438–441
Mazer LM, Tapper EB, Sarmiento JM (2011) Non-operative management of right posterior sectoral duct injury following laparoscopic cholecystectomy. J Gastrointest Surg 15:1237–1242
Flum DR, Dellinger EP, Cheadle A, Chan L, Koepsell T (2003) Intraoperative cholangiography and risk of common bile duct injury during cholecystectomy. JAMA 289:1639–1644
Dili A, Bertrand C (2017) Laparoscopic ultrasonography as an alternative to intraoperative cholangiography during laparoscopic cholecystectomy. World J Gastroenterol 23:5438–5450
Liu YY, Liao CH, Diana M, Wang SY, Kong SH, Yeh CN, Dallemagne B, Marescaux J, Yeh TS (2018) Near-infrared cholecystocholangiography with direct intragallbladder indocyanine green injection: preliminary clinical results. Surg Endosc 32:1506–1514
Pesce A, Latteri S, Barchitta M, Portale TR, Di Stefano B, Agodi A, Russello D, Puleo S, La Greca G (2018) Near-infrared fluorescent cholangiography—real-time visualization of the biliary tree during elective laparoscopic cholecystectomy. HPB (Oxford) 20:538–545
Acknowledgements
We are grateful to Kojiro Suzuki in the Department of Radiology, Aichi Medical University for valuable comments on radiological methods.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
S Kurahashi, S Komatsu, T Matsumura, Y Fukami, T Arikawa, T Saito, T Osawa, T Uchino, S Kato, K Suzuki, Y Toda, K Kaneko and T Sano have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kurahashi, S., Komatsu, S., Matsumura, T. et al. A novel classification of aberrant right hepatic ducts ensures a critical view of safety in laparoscopic cholecystectomy. Surg Endosc 34, 2904–2910 (2020). https://doi.org/10.1007/s00464-020-07610-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07610-8