Abstract
Objective
Hepatectomy is a complex operative procedure frequently performed at academic institutions with trainee participation. The aim of this study was to determine the effect of assistant’s training level on outcomes following hepatectomy.
Methods
A retrospective review of a prospective, single-institution ACS-NSQIP database was performed for patients that underwent hepatectomy (2013–2016). Patients were divided by trainee assistant level: hepatopancreatobiliary (HPB) fellow versus general surgery resident (PGY 4–5). Demographic, perioperative, and 30-day outcome variables were compared using Chi-Square/Fisher’s exact, Mann–Whitney U test, and multivariable regression. Cases involving a senior-level general surgery resident or HPB fellow as first assistant were included (n = 352). Those with a second attending, junior-level resident, or no documented assistant were excluded (n = 39).
Results
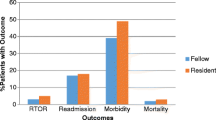
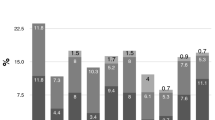
Patients undergoing hepatectomy with an HPB fellow as primary assistant had more frequent preoperative biliary stenting, longer operative time, and more concomitant procedures including biliary reconstruction, resulting in a higher rate of post-hepatectomy liver failure (PHLF) (15% vs. 8%, P = 0.044). However, trainee level did not impact PHLF on multivariable analysis (OR 0.60, 95% CI [0.29–1.25], P = 0.173). Fellows assisted with proportionally more major hepatectomies (45% vs. 31%; P = 0.010) and resections for hepatobiliary cancers (31% vs. 19%, P = 0.014). On stratified analysis of major and minor hepatectomies, outcomes were similar between trainee groups.
Conclusion
Fellows performed higher complexity cases with longer operative time. Despite these differences, outcomes were similar regardless of assistant training level. Resident and HPB fellow participation in operations requiring liver resection provide comparable quality of care.

Similar content being viewed by others
Abbreviations
- ACS-NSQIP:
-
American College of Surgeons National Surgical Quality Improvement Program
- DVT:
-
Deep venous thrombosis
- HPB:
-
Hepatopancreatobiliary
- ISGLS:
-
International Study Group of Liver Surgery
- MELD:
-
Model for End-Stage Liver Disease Score
- PGY:
-
Post-graduate-year
- PHLF:
-
Post-hepatectomy liver failure
References
Sachs TE, Ejaz A, Weiss M, Spolverato G, Ahuja N, Makary MA, Wolfgang CL, Hirose K, Pawlik TM (2014) Assessing the experience in complex hepatopancreatobiliary surgery among graduating chief residents: is the operative experience enough? Surgery 156:385–393
Steiner CA, Karaca Z, Moore BJ, Imshaug MC, Pickens G. Surgeries in Hospital-Based Ambulatory Surgery and Hospital Inpatient Settings, 2014. HCUP Statistical Brief #223. May 2017. Agency for Healthcare Research and Quality, Rockville, MD. Retrieved from www.hcupus.ahrq.gov/reports/statbriefs/sb223-Ambulatory-Inpatient-Surgeries-2014.pdf.
Raval MV, Wang X, Cohen ME, Ingraham AM, Bentrem DJ, Dimick JB, Flynn T, Hall BL, Ko CY (2011) The influence of resident involvement on surgical outcomes. J Am Coll Surg 212:889–898
Bellini G, Teng A, Lee DY, Rose K (2017) The effects of resident participation on patient morbidity and mortality in major gastrointestinal oncologic surgery. J Clin Oncol 35:437–437
Kiran RP, Ahmed Ali U, Coffey JC, Vogel JD, Pokala N, Fazio VW (2012) Impact of resident participation in surgical operations on postoperative outcomes: National Surgical Quality Improvement Program. Ann Surg 256:469–475
Shubert CR, Habermann EB, Truty MJ, Thomsen KM, Kendrick ML, Nagorney DM (2014) Defining perioperative risk after hepatectomy based on diagnosis and extent of resection. J Gastrointest Surg 18:1917–1928
Hyder O, Sachs T, Ejaz A, Spolverato G, Pawlik TM (2013) Impact of hospital teaching status on length of stay and mortality among patients undergoing complex hepatopancreaticobiliary surgery in the USA. J Gastrointest Surg 17:2114–2122
McKay A, You I, Bigam D, Lafreniere R, Sutherland F, Ghali W, Dixon E (2008) Impact of surgeon training on outcomes after resective hepatic surgery. Ann Surg Oncol 15:1348–1355
Kohn GP, Nikfarjam M (2010) The effect of surgical volume and the provision of residency and fellowship training on complications of major hepatic resection. J Gastrointest Surg 14:1981–1989
Jeyarajah DR, Berman RS, Doyle MB, Geevarghese SK, Posner MC, Farmer D, Minter RM (2016) Consensus Conference on North American Training in Hepatopancreaticobiliary Surgery: a review of the conference and presentation of consensus statements. Am J Transplant 16:1086–1093
Surgery RCf Defined Category Minimum Numbers: General Surgery Effective for Program Graduates Beginning Academic Year 2017–2018 [Internet] (2017). [cited 6/8/2018]. Available at https://www.acgme.org/Portals/0/UPDATED_DEFINED_CATEGORY_MINIMUM_NUMBERS_EFFECTIVE_ACADEMIC_YEAR_2017-2018_GENERAL_SURGERY.pdf.
MELD (Model For End-Stage Liver Disease) (12 and Older). [Internet]. 2016. [cited 6/8/2018]. Available at https://www.mdcalc.com/meld-score-model-end-stage-liver-disease-12-older.
Abdel-Misih SR, Bloomston M (2010) Liver anatomy. Surg Clin North Am 90:643–653
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, Koch M, Makuuchi M, Dematteo RP, Christophi C, Banting S, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Yokoyama Y, Fan ST, Nimura Y, Figueras J, Capussotti L, Buchler MW, Weitz J (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149:713–724
van Mierlo KM, Schaap FG, Dejong CH, Olde Damink SW (2016) Liver resection for cancer: New developments in prediction, prevention and management of postresectional liver failure. J Hepatol 65:1217–1231
van den Broek MA, Olde Damink SW, Dejong CH, Lang H, Malago M, Jalan R, Saner FH (2008) Liver failure after partial hepatic resection: definition, pathophysiology, risk factors and treatment. Liver Int 28:767–780
Jara M, Reese T, Malinowski M, Valle E, Seehofer D, Puhl G, Neuhaus P, Pratschke J, Stockmann M (2015) Reductions in post-hepatectomy liver failure and related mortality after implementation of the LiMAx algorithm in preoperative work-up: a single-centre analysis of 1170 hepatectomies of one or more segments. HPB 17:651–658
Kauffmann R, Fong Y (2014) Post-hepatectomy liver failure. Hepatobiliary Surg Nutr 3:238–246
Helling TS, Khandelwal A (2008) The challenges of resident training in complex hepatic, pancreatic, and biliary procedures. J Gastrointest Surg 12:153–158
Zyromski NJ, Torbeck L, Canal DF, Lillemoe KD, Pitt HA (2010) Incorporating an HPB fellowship does not diminish surgical residents' HPB experience in a high-volume training centre. HPB 12:123–128
Carr RA, Chung CW, Schmidt CM 2nd, Jester A, Kilbane ME, House MG, Zyromski NJ, Nakeeb A, Schmidt CM, Ceppa EP (2017) Impact of fellow versus resident assistance on outcomes following pancreatoduodenectomy. J Gastrointest Surg 21:1025–1030
Linn JG, Hungness ES, Clark S, Nagle AP, Wang E, Soper NJ (2011) General surgery training without laparoscopic surgery fellows: the impact on residents and patients. Surgery 150:752–758
Ross SW, Oommen B, Kim M, Walters AL, Green JM, Heniford BT, Augenstein VA (2014) A little slower, but just as good: postgraduate year resident versus attending outcomes in laparoscopic ventral hernia repair. Surg Endosc 28:3092–3100
Kingham TP, Correa-Gallego C, D'Angelica MI, Gonen M, DeMatteo RP, Fong Y, Allen PJ, Blumgart LH, Jarnagin WR (2015) Hepatic parenchymal preservation surgery: decreasing morbidity and mortality rates in 4,152 resections for malignancy. J Am Coll Surg 220:471–479
Virani S, Michaelson JS, Hutter MM, Lancaster RT, Warshaw AL, Henderson WG, Khuri SF, Tanabe KK (2007) Morbidity and mortality after liver resection: results of the patient safety in surgery study. J Am Coll Surg 204:1284–1292
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
RE Simpson, KL Carpenter, CY Wang, CM Schmidt II, EM Kilbane, CL Colgate, MG House, NJ Zyromski, CM Schmidt, A Nakeeb, and EP Ceppa have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Simpson, R.E., Carpenter, K.L., Wang, C.Y. et al. Is resident assistance equivalent to fellows during hepatectomy?. Surg Endosc 35, 260–269 (2021). https://doi.org/10.1007/s00464-020-07388-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07388-9