Abstract
Background
Approximately 3–6% of patients undergoing anti-reflux surgery require “redo” surgery for persistent gastroesophageal reflux disease (GERD). Further surgery for patients with two failed prior anti-reflux operations is controversial due to the morbidity of reoperation and poor outcomes. We examined our experience with surgical revision of patients with at least two failed anti-reflux operations.
Methods
Adults undergoing at least a second-time revision anti-reflux surgery between 1999 and 2017 were eligible. The primary outcomes were general and disease-specific quality-of-life (QoL) scores determined by Short-Form-36 (SF36) and GERD-Health-Related QoL (GERD-HRQL) instruments, respectively. Secondary outcomes included perioperative morbidity and mortality.
Results
Eighteen patients undergoing redo–redo surgery (13 with 2 prior operations, 5 with 3 prior operations) were followed for a median of 6 years [IQR 3, 12]. Sixteen patients (89%) underwent open revisions (14 thoracoabdominal, 2 laparotomy) and two patients had laparoscopic revisions. Indications for surgery included reflux (10 patients), regurgitation (5 patients), and dysphagia (3 patients). Intraoperative findings were mediastinal wrap herniation (9 patients), misplaced wrap (2 patients), mesh erosion (1 patient), or scarring/stricture (6 patients). Procedures performed included Collis gastroplasty + fundoplication (6 patients), redo fundoplication (5 patients), esophagogastrectomy (4 patients), and primary hiatal closure (3 patients). There were no deaths and 13/18 patients (72%) had no postoperative complications. Ten patients completed QoL surveys; 8 reported resolution of reflux, 6 reported resolution of regurgitation, while 4 remained on proton-pump inhibitors (PPI). Mean SF36 scores (± standard deviation) in the study cohort in the eight QoL domains were as follows: physical functioning (79.5 [± 19.9]), physical role limitations (52.5 [± 46.3]), emotional role limitations (83.3 [± 36.1]), vitality (60.0 [± 22.7]), emotional well-being (88.4 [± 8.7]), social functioning (75.2 [± 31.0]), pain (66.2 [± 30.9]), and general health (55.0 [± 39.0]).
Conclusion
An open thoracoabdominal approach in appropriately selected patients needing third-time anti-reflux surgery carries low morbidity and provides excellent results as reflected in QoL scores.
Graphic abstract



Similar content being viewed by others
References
Al Hashmi A-W, Pineton de Chambrun G, Souche R, Bertrand M, De Blasi V, Jacques E, Azagra S, Fabre JM, Borie F, Prudhomme M, Nagot N, Navarro F, Panaro F (2019) A retrospective multicenter analysis on redo-laparoscopic anti-reflux surgery: conservative or conversion fundoplication? Surg Endosc 33:243–251. https://doi.org/10.1007/s00464-018-6304-z
Carlson MA, Frantzides CT (2001) Complications and results of primary minimally invasive antireflux procedures: a review of 10,735 reported cases. J Am Coll Surg 193:428–439. https://doi.org/10.1016/S1072-7515(01)00992-9
Makdisi G, Nichols FC, Cassivi SD, Wigle DA, Shen KR, Allen MS, Deschamps C (2014) Laparoscopic repair for failed antireflux procedures. Ann Thorac Surg 98:1261–1266. https://doi.org/10.1016/j.athoracsur.2014.05.036
Ohnmacht GA, Deschamps C, Cassivi SD, Nichols FC, Allen MS, Schleck CD, Pairolero PC (2006) Failed antireflux surgery: results after reoperation. Ann Thorac Surg 81:2050–2054. https://doi.org/10.1016/j.athoracsur.2006.01.019
Smith CD, McClusky DA, Rajad MA, Lederman AB, Hunter JG (2005) When fundoplication fails. Ann Surg 241:861–871. https://doi.org/10.1097/01.sla.0000165198.29398.4b
Awais O, Luketich JD, Schuchert MJ, Morse CR, Wilson J, Gooding WE, Landreneau RJ, Pennathur A (2011) Reoperative antireflux surgery for failed fundoplication: an analysis of outcomes in 275 patients. Ann Thorac Surg 92:1083–1089. https://doi.org/10.1016/j.athoracsur.2011.02.088
Little AG, Ferguson MK, Skinner DB (1986) Reoperation for failed antireflux operations. J Thorac Cardiovasc Surg 91:511–517
36-Item Short Form Survey (SF-36)|RAND (n.d.). https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form.html. Accessed 26 Feb 2019
Contopoulos-Ioannidis DG, Karvouni A, Kouri I, Ioannidis JPA (2009) Reporting and interpretation of SF-36 outcomes in randomised trials: systematic review. BMJ 338:a3006. https://doi.org/10.1136/bmj.a3006
García M, Rohlfs I, Vila J, Sala J, Pena A, Masiá R, Marrugat J, REGICOR Investigators (n.d.) Comparison between telephone and self-administration of Short Form Health Survey Questionnaire (SF-36). Gac Sanit 19: 433–439. http://www.ncbi.nlm.nih.gov/pubmed/16483520. Accessed 26 Feb 2019
Maglinte GA, Hays RD, Kaplan RM (2012) US general population norms for telephone administration of the SF-36v2. J Clin Epidemiol 65:497–502. https://doi.org/10.1016/j.jclinepi.2011.09.008
Velanovich V (2007) The development of the GERD-HRQL symptom severity instrument. Dis Esophagus 20:130–134. https://doi.org/10.1111/j.1442-2050.2007.00658.x
Nason KS, Wichienkuer PP, Awais O, Schuchert MJ, Luketich JD, O’Rourke RW, Hunter JG, Morris CD, Jobe BA (2011) Gastroesophageal reflux disease symptom severity, proton pump inhibitor use, and esophageal carcinogenesis. Arch Surg 146:851–858. https://doi.org/10.1001/archsurg.2011.174
Spechler SJ, Lee E, Ahnen D, Goyal RK, Hirano I, Ramirez F, Raufman J-P, Sampliner R, Schnell T, Sontag S, Vlahcevic ZR, Young R, Williford W (2001) Long-term outcome of medical and surgical therapies for gastroesophageal reflux disease. JAMA 285:2331. https://doi.org/10.1001/jama.285.18.2331
Furnée EJB, Draaisma WA, Broeders IAMJ, Gooszen HG (2009) Surgical reintervention after failed antireflux surgery : a systematic review of the literature. J Gastrointest Surg 13:1539–1549. https://doi.org/10.1007/s11605-009-0873-z
Antiporda M, Jackson C, Smith CD, Thomas M, Elli EF, Bowers SP (2018) Strategies for surgical remediation of the multi-fundoplication failure patient. Surg Endosc 33:1474. https://doi.org/10.1007/s00464-018-6429-0
van Beek DB, Auyang ED, Soper NJ (2011) A comprehensive review of laparoscopic redo fundoplication. Surg Endosc 25:706–712. https://doi.org/10.1007/s00464-010-1254-0
Awais O, Luketich JD, Schuchert MJ, Morse CR, Wilson J, Gooding WE, Landreneau RJ, Pennathur A (2011) Reoperative antireflux surgery for failed fundoplication: an analysis of outcomes in 275 patients. ATS 92:1083–1090. https://doi.org/10.1016/j.athoracsur.2011.02.088
Gee DW, Andreoli MT, Rattner DW (2008) Measuring the effectiveness of laparoscopic antireflux surgery: long-term results. Arch Surg 143:482–487. https://doi.org/10.1001/archsurg.143.5.482
Singhal S, Kirkpatrick DR, Masuda T, Gerhardt J, Mittal SK (2018) Primary and redo antireflux surgery: outcomes and lessons learned. J Gastrointest Surg 22:177–186. https://doi.org/10.1007/s11605-017-3480-4
Aloia TA, Zorzi D, Abdalla EK, Vauthey J-N (2005) Two-surgeon technique for hepatic parenchymal transection of the noncirrhotic liver using saline-linked cautery and ultrasonic dissection. Ann Surg 242:172–177. https://doi.org/10.1097/01.SLA.0000171300.62318.F4
Mallory MA, Losk K, Camuso K, Caterson S, Nimbkar S, Golshan M (2016) Does “two is better than one” apply to surgeons? Comparing single-surgeon versus co-surgeon bilateral mastectomies. Ann Surg Oncol 23:1111–1116. https://doi.org/10.1245/s10434-015-4956-7
Johnson SM, Lee WG, Puapong DP, Woo RK (2019) The pediatric surgical team: a model for increased surgeon index case exposure. J Pediatr Surg 2:89. https://doi.org/10.1016/j.jpedsurg.2018.12.018
Schlottmann F, Strassle PD, Patti MG (2018) Antireflux surgery in the USA: influence of surgical volume on perioperative outcomes and costs—time for centralization? World J Surg 42:2183–2189. https://doi.org/10.1007/s00268-017-4429-1
Svircevic V, van Dijk D, Nierich AP, Passier MP, Kalkman CJ, van der Heijden GJMG, Bax L (2011) Meta-analysis of thoracic epidural anesthesia versus general anesthesia for cardiac surgery. Anesthesiology 114:271–282. https://doi.org/10.1097/ALN.0b013e318201d300
Wei K, Min S, Hao Y, Ran W, Lv F (2019) Postoperative analgesia after combined thoracoscopic-laparoscopic esophagectomy: a randomized comparison of continuous infusion and intermittent bolus thoracic epidural regimens. J Pain Res 12:29–37. https://doi.org/10.2147/JPR.S188568
Li C, Ferri LE, Mulder DS, Ncuti A, Neville A, Lee L, Kaneva P, Watson D, Vassiliou M, Carli F, Feldman LS (2012) An enhanced recovery pathway decreases duration of stay after esophagectomy. Surgery. 152:606–616. https://doi.org/10.1016/j.surg.2012.07.021
Shewale JB, Correa AM, Baker CM, Villafane-Ferriol N, Hofstetter WL, Jordan VS, Kehlet H, Lewis KM, Mehran RJ, Summers BL, Schaub D, Wilks SA, Swisher SG, T.U. of T.M.A.E.C.C. University of Texas MD Anderson Esophageal Cancer Collaborative Group (2015) Impact of a fast-track esophagectomy protocol on esophageal cancer patient outcomes and hospital charges. Ann Surg 261:1114–1123. https://doi.org/10.1097/sla.0000000000000971
Mittal SK, Légner A, Tsuboi K, Juhasz A, Bathla L, Lee TH (2013) Roux-en-Y reconstruction is superior to redo fundoplication in a subset of patients with failed antireflux surgery. Surg Endosc 27:927–935. https://doi.org/10.1007/s00464-012-2537-4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Nikhil Panda is supported through the NIH T32 DK007754-18 (Research Training in Alimentary Tract Surgery) training grant. Dr. Christopher Morse has a consulting agreement with Olympus. Dr. David Rattner has a consulting agreement with Olympus.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
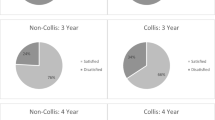
Appendix: GERD-Health Related Quality of Lift Questionnaire (GERD-HRQL) administered to patients in this study. Questions 1–9 were used to determine the “modified GERD-HRQL,” reported in a prior study by our research group [12]
Appendix: GERD-Health Related Quality of Lift Questionnaire (GERD-HRQL) administered to patients in this study. Questions 1–9 were used to determine the “modified GERD-HRQL,” reported in a prior study by our research group [12]
[] On PPIs [] Off PPIs If off, for how long? ____________ (days/months)
-
Scale for following questions:
-
0: no symptom
-
1: symptoms noticeable but not bothersome
-
2: symptoms noticeable and bothersome but not every day
-
3: symptoms bothersome every day
-
4: symptoms affect daily activity
-
5: symptoms are incapacitating to do daily activities
-
1.
How bad is the heartburn?
-
2.
Heartburn when lying down?
-
3.
Heartburn when standing up?
-
4.
Heartburn after meals?
-
5.
Does heartburn change your diet?
-
6.
Does heartburn wake you from sleep?
-
7.
Do you have difficulty swallowing?
-
8.
Do you have pain with swallowing?
-
9.
If you take medication, does this affect your daily life?
-
10.
How bad is the regurgitation?
-
11.
Regurgitation when lying down?
-
12.
Regurgitation when standing up?
-
13.
Regurgitation after meals?
-
14.
Does regurgitation change your diet?
-
15.
Does regurgitation wake you from sleep?
-
16.
How satisfied are you with your present condition?
[] Satisfied
[] Neutral
[] Dissatisfied
-
1.
Rights and permissions
About this article
Cite this article
Panda, N., Rattner, D.W. & Morse, C.R. Third-time (“redo–redo”) anti-reflux surgery: patient-reported outcomes after a thoracoabdominal approach. Surg Endosc 34, 3092–3101 (2020). https://doi.org/10.1007/s00464-019-07059-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07059-4