Abstract
Background
Minimally Invasive Liver Resection (MILR) techniques range from a hybrid-technique to full robotic approaches. When compared with open techniques, MILR has been shown to be advantageous by reducing pain, complications, length of stay and blood loss. The aim of this study was to compare clinical outcomes and hospital resource utilization between full laparoscopic, hand-assisted, and robotic liver resections among major (≥ 3 segments) and minor (≤ 2 segments) resections.
Methods
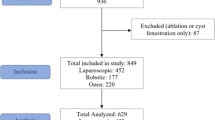
A single-center comparative retrospective review was completed on 214 patients undergoing full laparoscopic, hand-assisted, or robotic liver resection procedures between 2005 and 2018.
Results
Among minor resections: 85 full laparoscopic, 40 hand-assisted, and 35 robotic liver resection cases were analyzed; and among major resections: 13, 33, and 8 cases were analyzed, respectively. In the adjusted subgroup analysis of minor resections, OR time was significantly longer for the minor hand-assisted group (\( \bar{x} \) = 181 min; p < 0.05), and the average lesion size was smaller for the minor full laparoscopic group (\( \bar{x} \) = 4.2 cm; p < 0.05). Overall, direct hospital charges were lowest in the group of patients who underwent a minor resection using the full laparoscopic technique (\( \bar{x} \) = $39,054.90; p < 0.05), compared to the robotic technique. Due to the smaller sample size (n = 54) in the major resection subgroup, only two significant observations were made - the full laparoscopic group had the least amount of blood loss (\( \bar{x} \) = 227 cc; p < 0.05) and incurred the least amount of room and board charges compared to the other two techniques.
Conclusions
The robotic approach appears favorable for minor resections as evidenced by shorter length of stay but more costly than full laparoscopy. Clinical outcomes appear to be more dependent upon the magnitude of the resection (i.e. major vs. minor) than the MILR technique chosen. Randomized trials may be indicated to discern the best indications and advantages of each technique.



Similar content being viewed by others
References
Katkhouda N, Fabiani P, Benizri E, Mouiel J (1992) Laser resection of a liver hydatid cyst under videolaparoscopy. Br J Surg 79:560–561
Komatsu S, Scatton O, Goumard C, Sepulveda A, Brustia R, Perdigao F, Soubrane O (2017) Development process and technical aspects of laparoscopic hepatectomy: learning curve based on 15 years of experience. J Am Coll Surg 224:841–850
Thornblade LW, Shi X, Ruiz A, Flum DR, Park JO (2017) Comparative effectiveness of minimally invasive surgery and conventional approaches for major or challenging hepatectomy. J Am Coll Surg 224:851–861
Croner RS, Perrakis A, Hohenberger W, Brunner M (2016) Robotic liver surgery for minor hepatic resections: a comparison with laparoscopic and open standard procedures. Langenbecks Arch Surg 401:707–714
Nota CL, Rinkes IHB, Molenaar IQ, van Santvoort HC, Fong Y, Hagendoorn J (2016) Robot-assisted laparoscopic liver resection: a systematic review and pooled analysis of minor and major hepatectomies. HPB 18:113–120
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection-2,804 patients. Ann Surg 250:831–841
Schiffman SC, Kim KH, Tsung A, Marsh JW, Geller DA (2015) Laparoscopic versus open liver resection for metastatic colorectal cancer: a metaanalysis of 610 patients. Surgery 157:211–222
Sham JG, Richards MK, Seo YD, Pillarisetty VG, Yeung RS, Park JO (2016) Efficacy and cost of robotic hepatectomy: is the robot cost-prohibitive? J Robot Surg 10:307–313
Bagante F, Spolverato G, Strasberg SM, Gani F, Thompson V, Hall BL, Bentrem DJ, Pitt HA, Pawlik TM (2016) Minimally invasive vs. open hepatectomy: a comparative analysis of the national surgical quality improvement program database. J Gastrointest Surgery 20:1608–1617
Rao A, Rao G, Ahmed I (2012) Laparoscopic vs. open liver resection for malignant liver disease. A systematic review. Surgeon 10:194–201
Pilgrim CH, To H, Usatoff V, Evans PM (2009) Laparoscopic hepatectomy is a safe procedure for cancer patients. HPB 11:247–251
Simillis C, Constantinides VA, Tekkis PP, Darzi A, Lovegrove R, Jiao L, Antoniou A (2007) Laparoscopic versus open hepatic resections for benign and malignant neoplasms—a meta-analysis. Surgery 141:203–211
Medbery RL, Chadid TS, Sweeney JF, Knechtle SJ, Kooby DA, Maithel SK, Lin E, Sarmiento JM (2014) Laparoscopic vs open right hepatectomy: a value-based analysis. J Am Coll Surg 218:929–939
Yu YD, Kim KH, Jung DH, Namkoong JM, Yoon SY, Jung SW, Lee SK, Lee SG (2014) Robotic versus laparoscopic liver resection: a comparative study from a single center. Langenbecks Arch Surg 399:1039–1045
Magistri P, Tarantino G, Guidetti C, Assirati G, Olivieri T, Ballarin R, Coratti A, Di Benedetto F (2017) Laparoscopic versus robotic surgery for hepatocellular carcinoma: the first 46 consecutive cases. J Surg Res 217:92–99
Wu YM, Hu RH, Lai HS, Lee PH (2014) Robotic-assisted minimally invasive liver resection. Asian J Surg 37:53–57
Koffron AJ, Auffenberg G, Kung R, Abecassis M (2007) Evaluation of 300 minimally invasive liver resections at a single institution: less is more. Ann Surg 246:385–392; discussion 384–392
Daskalaki D, Gonzalez-Heredia R, Brown M, Bianco FM, Tzvetanov I, Davis M, Kim J, Benedetti E, Giulianotti PC (2017) Financial impact of the robotic approach in liver surgery: a comparative study of clinical outcomes and costs between the robotic and open technique in a single institution. J Laparoendosc Adv Surg Tech A 27:375–382
Cannon RM, Scoggins CR, Callender GG, Quillo A, McMasters KM, Martin RC II (2013) Financial comparison of laparoscopic versus open hepatic resection using deviation-based cost modeling. Ann Surg Oncol 20:2887–2892
Kawaguchi Y, Otsuka Y, Kaneko H, Nagai M, Nomura Y, Yamamoto M, Otani M, Ohashi Y, Sugawara K, Koike D, Ishida T, Kokudo N, Tanaka N (2016) Comparisons of financial and short-term outcomes between laparoscopic and open hepatectomy: benefits for patients and hospitals. Surg Today 46:535–542
Limongelli P, Vitiello C, Belli A, Pai M, Tolone S, Del Genio G, Brusciano L, Docimo G, Habib N, Belli G, Jiao LR, Docimo L (2014) Costs of laparoscopic and open liver and pancreatic resection: a systematic review. World J Gastroenterol 20:17595–17602
Vanounou T, Steel JL, Nguyen KT, Tsung A, Marsh JW, Geller DA, Gamblin TC (2010) Comparing the clinical and economic impact of laparoscopic versus open liver resection. Ann Surg Oncol 17:998–1009
Packiam V, Bartlett DL, Tohme S, Reddy S, Marsh JW, Geller DA, Tsung A (2012) Minimally invasive liver resection: robotic versus laparoscopic left lateral sectionectomy. J Gastrointest Surg 16:2233–2238
Rich MW, Nease RF (1999) Cost-effectiveness analysis in clinical practice: the case of heart failure. Arch Intern Med 159:1690–1700
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Author Alejandro Mejia participates in an Institutional Agreement with Intuitive Surgical as a Proctor and case observations for surgeons. Dr. Stephen Cheng, Mrs. Elaina Vivian, Mr. Jimmy Shah, Mrs. Hellen Oduor, and Mrs. Priyanka Archarya have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mejia, A., Cheng, S.S., Vivian, E. et al. Minimally invasive liver resection in the era of robotics: analysis of 214 cases. Surg Endosc 34, 339–348 (2020). https://doi.org/10.1007/s00464-019-06773-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06773-3