Abstract
Background
Endoscopic submucosal dissection allows for “en bloc” removal of early gastrointestinal neoplasms. However, it is technically demanding and time-consuming. Alternatives could rely on energy-based techniques. We aimed to evaluate a predictive numerical model of thermal damage to preoperatively define optimal laser settings allowing for a controlled ablation down to the submucosa, and the ability of confocal endomicroscopy to provide damage information.
Materials and methods
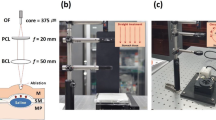
A Nd:YAG laser was applied onto the gastric mucosa of 21 Wistar rats on 10 spots (total 210). Power settings ranging from 0.5 to 2.5W were applied during 1–12 s, with a consequent energy delivery varying from 0.5 to 30 J. Out of the 210 samples, a total of 1050 hematoxilin–eosin stained slides were obtained. To evaluate thermal injury, the ratio between the damage depth (DD) over the mucosa and the submucosa thickness (T) was calculated. Effective and safe ablation was considered for a DD/T ratio ≤ 1 (only mucosal and submucosal damage). Confocal endomicroscopy was performed before and after ablation. A numerical model, using human physical properties, was developed to predict thermal damage.
Results
No full-thickness perforations were detected. On histology, the DD/T ratio at 0.5 J was 0.57 ± 0.21, significantly lower when compared to energies ranging from 15 J (a DD/T ratio = 1.2 ± 0.3; p < 0.001) until 30 J (a DD/T ratio = 1.33 ± 0.31; p < 0.001). Safe mucosal and submucosal ablations were achieved applying energy between 4 and 12 J, never impairing the muscularis propria. Confocal endomicroscopy showed a distorted gland architecture. The predicted damage depth demonstrated a significant positive linear correlation with the experimental data (Pearson’s r 0.85; 95% CI 0.66–0.94).
Conclusions
Low-power settings achieved effective and safe mucosal and submucosal ablation. The numerical model allowed for an accurate prediction of the ablated layers. Confocal endomicroscopy provided real-time thermal damage visualization. Further studies on larger animal models are required.






Similar content being viewed by others
References
Marin-Gabriel JC, Fernandez-Esparrach G, Diaz-Tasende J, Herreros de Tejada A (2016) Colorectal endoscopic submucosal dissection from a Western perspective: today’s promises and future challenges. World J Gastrointest Endosc 8:40–55
Holmes I, Friedland S (2016) Endoscopic mucosal resection versus endoscopic submucosal dissection for large polyps: a Western colonoscopist’s view. Clin Endosc 49:454–456
Uedo N, Takeuchi Y, Ishihara R (2012) Endoscopic management of early gastric cancer: endoscopic mucosal resection or endoscopic submucosal dissection: data from a Japanese high-volume center and literature review. Ann Gastroenterol 25:281–290
Ohta T, Ishihara R, Uedo N, Takeuchi Y, Nagai K, Matsui F, Kawada N, Yamashina T, Kanzaki H, Hanafusa M, Yamamoto S, Hanaoka N, Higashino K, Iishi H (2012) Factors predicting perforation during endoscopic submucosal dissection for gastric cancer. Gastrointest Endosc 75:1159–1165
Oda I, Suzuki H, Nonaka S, Yoshinaga S (2013) Complications of gastric endoscopic submucosal dissection. Dig Endosc 25(Suppl 1):71–78
Hanaoka N, Uedo N, Ishihara R, Higashino K, Takeuchi Y, Inoue T, Chatani R, Hanafusa M, Tsujii Y, Kanzaki H, Kawada N, Iishi H, Tatsuta M, Tomita Y, Miyashiro I, Yano M (2010) Clinical features and outcomes of delayed perforation after endoscopic submucosal dissection for early gastric cancer. Endoscopy 42:1112–1115
Baldaque-Silva F, Cardoso H, Lopes J, Carneiro F, Macedo G (2013) Radiofrequency ablation for the treatment of gastric dysplasia: a pilot experience in three patients. Eur J Gastroenterol Hepatol 25:863–868
Diana M, Schiraldi L, Liu YY, Memeo R, Mutter D, Pessaux P, Marescaux J (2016) High intensity focused ultrasound (HIFU) applied to hepato-bilio-pancreatic and the digestive system-current state of the art and future perspectives. Hepatobiliary Surg Nutr 5:329–344
Luigiano C, Iabichino G, Eusebi LH, Arena M, Consolo P, Morace C, Opocher E, Mangiavillano B (2016) Outcomes of radiofrequency ablation for dysplastic Barrett’s esophagus: a comprehensive review. Gastroenterol Res Pract 2016:4249510
Mao Y, Qiu H, Liu Q, Lu Z, Fan K, Huang Y, Yang Y (2013) Endoscopic holmium:YAG laser ablation of early gastrointestinal intramucosal cancer. Lasers Med Sci 28:1505–1509
Peter S, Monkemuller K (2015) Ablative endoscopic therapies for Barrett’s-esophagus-related neoplasia. Gastroenterol Clin North Am 44:337–353
Rabenstein T, May A, Gossner L, Manner H, Pech O, Gunter E, Huijmans J, Vieth M, Stolte M, Ell C (2008) Invisible gastric carcinoma detected by random biopsy: long-term results after photodynamic therapy. Endoscopy 40:899–904
Schena E, Saccomandi P, Fong Y (2017) Laser ablation for cancer: past, present and future. J Funct Biomater 8
Sibille A, Descamps C, Jonard P, Dive C, Warzee P, Schapira M, Geubel A (1995) Endoscopic Nd:YAG treatment of superficial gastric carcinoma: experience in 18 Western inoperable patients. Gastrointest Endosc 42:340–345
Tajiri H, Oguro Y (1991) Laser endoscopic treatment for upper gastrointestinal cancers. J Laparoendosc Surg 1:71–78
Tani M, Takeshita K, Honda T, Saito N, Endo M (1997) Results of endoscopic treatment for early gastric cancer by Nd-YAG Laser. Diagn Ther Endosc 3:203–210
Yang GR, Zhao LQ, Li SS, Qiu SL, Wang YM, Jia JH (1994) Endoscopic Nd:YAG laser therapy in patients with early superficial carcinoma of the esophagus and the gastric cardia. Endoscopy 26:681–685
Yasuda K, Mizuma Y, Nakajima M, Kawai K (1993) Endoscopic laser treatment for early gastric cancer. Endoscopy 25:451–454
Lightdale CJ, Heier SK, Marcon NE, McCaughan JS Jr, Gerdes H, Overholt BF, Sivak MV Jr, Stiegmann GV, Nava HR (1995) Photodynamic therapy with porfimer sodium versus thermal ablation therapy with Nd:YAG laser for palliation of esophageal cancer: a multicenter randomized trial. Gastrointest Endosc 42:507–512
Saccomandi P, Quero G, Costamagna G, Diana M, Marescaux J (2017) Effects of Nd:YAG laser for the controlled and localized treatment of early gastrointestinal tumors: Preliminary in vivo study. Conf Proc IEEE Eng Med Biol Soc 2017:4533–4536
Müller GJ, Roggan A (1995) Laser-induced interstitial thermotherapy. SPIE Press, Bellingham
Saccomandi P, Schena E, Caponero MA, Di Matteo FM, Martino M, Pandolfi M, Silvestri S (2012) Theoretical analysis and experimental evaluation of laser-induced interstitial thermotherapy in ex vivo porcine pancreas. IEEE Trans Biomed Eng 59:2958–2964
Takemoto T (1986) Laser therapy of early gastric carcinoma. Endoscopy 18(Suppl 1):32–36
Fleischer D, Kessler F, Haye O (1982) Endoscopic Nd: YAG laser therapy for carcinoma of the esophagus: a new palliative approach. Am J Surg 143:280–283
Fleischer D, Sivak MV Jr (1985) Endoscopic Nd:YAG laser therapy as palliation for esophagogastric cancer. Parameters affecting initial outcome. Gastroenterology 89:827–831
Tytgat GN (1990) Endoscopic therapy of esophageal cancer: possibilities and limitations. Endoscopy 22:263–267
Mellow MH, Pinkas H (1984) Endoscopic therapy for esophageal carcinoma with Nd:YAG laser: prospective evaluation of efficacy, complications, and survival. Gastrointest Endosc 30:334–339
Naveau S, Chiesa A, Poynard T, Chaput JC (1990) Endoscopic Nd-YAG laser therapy as palliative treatment for esophageal and cardial cancer. Parameters affecting long-term outcome. Dig Dis Sci 35:294–301
Diana M, Noll E, Charles AL, Diemunsch P, Geny B, Liu YY, Marchegiani F, Schiraldi L, Agnus V, Lindner V, Swanstrom L, Dallemagne B, Marescaux J (2017) Precision real-time evaluation of bowel perfusion: accuracy of confocal endomicroscopy assessment of stoma in a controlled hemorrhagic shock model. Surg Endosc 31:680–691
Wu T, Heuillard E, Lindner V, Bou About G, Ignat M, Dillenseger JP, Anton N, Dalimier E, Gosse F, Foure G, Blindauer F, Giraudeau C, El-Saghire H, Bouhadjar M, Calligaro C, Sorg T, Choquet P, Vandamme T, Ferrand C, Marescaux J, Baumert TF, Diana M, Pessaux P, Robinet E (2016) Multimodal imaging of a humanized orthotopic model of hepatocellular carcinoma in immunodeficient mice. Sci Rep 6:35230
Diana M, Robinet E, Liu YY, Legner A, Kong SH, Schiraldi L, Marchegiani F, Halvax P, Swanstrom L, Dallemagne B, Marescaux J (2016) Confocal imaging and tissue-specific fluorescent probes for real-time in vivo immunohistochemistry. Proof of the concept in a gastric lymph node metastasis model. Ann Surg Oncol 23:567–573
Diana M, Dallemagne B, Chung H, Nagao Y, Halvax P, Agnus V, Soler L, Lindner V, Demartines N, Diemunsch P, Geny B, Swanstrom L, Marescaux J (2014) Probe-based confocal laser endomicroscopy and fluorescence-based enhanced reality for real-time assessment of intestinal microcirculation in a porcine model of sigmoid ischemia. Surg Endosc 28:3224–3233
Englhard AS, Palaras A, Volgger V, Stepp H, Mack B, Libl D, Gires O, Betz CS (2017) Confocal laser endomicroscopy in head and neck malignancies using FITC-labelled EpCAM- and EGF-R-antibodies in cell lines and tumor biopsies. J Biophotonics 10:1365–1376
Harlaar NJ, Koller M, de Jongh SJ, van Leeuwen BL, Hemmer PH, Kruijff S, van Ginkel RJ, Been LB, de Jong JS, Kats-Ugurlu G, Linssen MD, Jorritsma-Smit A, van Oosten M, Nagengast WB, Ntziachristos V, van Dam GM (2016) Molecular fluorescence-guided surgery of peritoneal carcinomatosis of colorectal origin: a single-centre feasibility study. Lancet Gastroenterol Hepatol 1:283–290
Acknowledgements
Authors would like to thank Christopher Burel and Guy Temporal, professionals in Medical English proofreading, for their valuable help in revising the manuscript.
Funding
This study was partly funded by the ARC Foundation, through the ELIOS Grant (PI: Michele Diana).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Michele Diana is the recipient of a grant from the ARC Foundation. Jacques Marescaux is the President of IRCAD and IHU-Strasbourg institutes, which are partly funded by Karl Storz, Siemens Healthcare, and Medtronic. Drs. Giuseppe Quero, Paola Saccomandi, Jung-Myun Kwak, Bernard Dallemagne, Guido Costamagna, Didier Mutter, have no conflicts of interests or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Quero, G., Saccomandi, P., Kwak, JM. et al. Modular laser-based endoluminal ablation of the gastrointestinal tract: in vivo dose–effect evaluation and predictive numerical model. Surg Endosc 33, 3200–3208 (2019). https://doi.org/10.1007/s00464-018-6603-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6603-4