Abstract
Background
How increasing age affects the characteristics of groin hernia remains uncertain. This study evaluated the association between age and the type of groin hernia, especially with respect to its multiplicity, observed during laparoscopic transabdominal preperitoneal (TAPP) hernia repair.
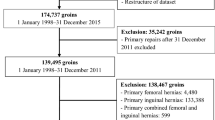
Methods
We retrospectively evaluated 634 consecutive patients with primary groin hernia who underwent laparoscopic TAPP repair between October 2000 and June 2017. Patients were stratified into 4 age groups: < 60 years, 60–69 years, 70–79 years, and 80 years or older.
Results
The incidence of occult contralateral hernia and multiple ipsilateral hernias increased significantly with each increasing age group: 7.3%, 10.4%, 12.7%, and 20.8% for occult contralateral hernia (p = 0.005), and 5.6%, 9.2%, 16.8%, and 21.7% for multiple ipsilateral hernias (p < 0.001), respectively. Univariate analyses showed that an older age (age ≥ 70 years) was the only factor significantly associated with the presence of multiple groin hernias (odds ratio, 2.69; 95% confidence interval, 1.89–3.81; p < 0.001). In patients with multiple ipsilateral hernias, the prevalent form in men was a pantaloons hernia, with an incidence of about 70% across all age groups, whereas in women it was groin hernias, with one component being a femoral hernia, an obturator hernia, or both.
Conclusions
The multiple occurrence of groin hernias, either unilaterally or bilaterally, was a clinical feature in the elderly.


Similar content being viewed by others
References
Ruhl CE, Everhart JE (2007) Risk factors for inguinal hernia among adults in the US population. Am J Epidemiol 165:1154–1161
Rosemar A, Angeras U, Rosengren A (2008) Body mass index and groin hernia: a 34-year follow-up study in Swedish men. Ann Surg 247:1064–1068
Burcharth J, Pedersen M, Bisgaard T, Pedersen C, Rosenberg J (2013) Nationwide prevalence of groin hernia repair. PLoS ONE 8:e54367
Wagh PV, Leverich AP, Sun CN, White HJ, Read RC (1974) Direct inguinal herniation in men: a disease of collagen. J Surg Res 17:425–433
Pallati PK, Gupta PK, Bichala S, Gupta H, Fang X, Forse RA (2013) Short-term outcomes of inguinal hernia repair in octogenarians and nonagenarians. Hernia 17:723–727
Abrahamson J (1998) Etiology and pathophysiology of primary and recurrent groin hernia formation. Surg Clin North Am 78:953–972, vi
Lau H, Fang C, Yuen WK, Patil NG (2007) Risk factors for inguinal hernia in adult males: a case-control study. Surgery 141:262–266
Nations U (2017) World population prospects: the 2017 revision
Panton ON, Panton RJ (1994) Laparoscopic hernia repair. Am J Surg 167:535–537
Evans DS, Ghaneh P, Khan IM (1996) Day-case laparoscopic hernia repair. Br J Surg 83:1361–1363
Sayad P, Abdo Z, Cacchione R, Ferzli G (2000) Incidence of incipient contralateral hernia during laparoscopic hernia repair. Surg Endosc 14:543–545
Koehler RH (2002) Diagnosing the occult contralateral inguinal hernia. Surg Endosc 16:512–520
O’Rourke A, Zell JA, Varkey-Zell TT, Barone JL, Bayona M (2002) Laparoscopic diagnosis and repair of asymptomatic bilateral inguinal hernias. Am J Surg 183:15–19
Bochkarev V, Ringley C, Vitamvas M, Oleynikov D (2007) Bilateral laparoscopic inguinal hernia repair in patients with occult contralateral inguinal defects. Surg Endosc 21:734–736
Novitsky YW, Czerniach DR, Kercher KW, Kaban GK, Gallagher KA, Kelly JJ, Heniford BT, Litwin DE (2007) Advantages of laparoscopic transabdominal preperitoneal herniorrhaphy in the evaluation and management of inguinal hernias. Am J Surg 193:466–470
Griffin KJ, Harris S, Tang TY, Skelton N, Reed JB, Harris AM (2010) Incidence of contralateral occult inguinal hernia found at the time of laparoscopic trans-abdominal pre-peritoneal (TAPP) repair. Hernia 14:345–349
Pawanindra L, Philips P, Chander J, Ramteke VK (2010) Is unilateral laparoscopic TEP inguinal hernia repair a job half done? The case for bilateral repair. Surg Endosc 24:1737–1745
van den Heuvel B, Beudeker N, van den Broek J, Bogte A, Dwars BJ (2013) The incidence and natural course of occult inguinal hernias during TAPP repair: repair is beneficial. Surg Endosc 27:4142–4146
Wu CC, Chueh SC, Tsai YC (2016) Is contralateral exploration justified in endoscopic total extraperitoneal repair of clinical unilateral groin hernias—a prospective cohort study. Int J Surg 36:206–211
Ekberg O, Lasson A, Kesek P, van Westen D (1994) Ipsilateral multiple groin hernias. Surgery 115:557–562
Ramshaw B, Shuler FW, Jones HB, Duncan TD, White J, Wilson R, Lucas GW, Mason EM (2001) Laparoscopic inguinal hernia repair: lessons learned after 1224 consecutive cases. Surg Endosc 15:50–54
HerniaSurge G (2018) International guidelines for groin hernia management. Hernia 22:1–165
Thumbe VK, Evans DS (2001) To repair or not to repair incidental defects found on laparoscopic repair of groin hernia: early results of a randomized control trial. Surg Endosc 15:47–49
Lilly MC, Arregui ME (2002) Lipomas of the cord and round ligament. Ann Surg 235:586–590
Nasr AO, Tormey S, Walsh TN (2005) Lipoma of the cord and round ligament: an overlooked diagnosis? Hernia 9:245–247
Henriksen NA, Thorup J, Jorgensen LN (2012) Unsuspected femoral hernia in patients with a preoperative diagnosis of recurrent inguinal hernia. Hernia 16:381–385
Abramson JH, Gofin J, Hopp C, Makler A, Epstein LM (1978) The epidemiology of inguinal hernia. A survey in western Jerusalem. J Epidemiol Community Health 32:59–67
Liem MS, van der Graaf Y, Zwart RC, Geurts I, van Vroonhoven TJ (1997) Risk factors for inguinal hernia in women: a case-control study. The Coala trial group. Am J Epidemiol 146:721–726
Zendejas B, Hernandez-Irizarry R, Ramirez T, Lohse CM, Grossardt BR, Farley DR (2014) Relationship between body mass index and the incidence of inguinal hernia repairs: a population-based study in Olmsted County. MN Hernia 18:283–288
Glassow F (1985) Femoral hernia. Review of 2,105 repairs in a 17 year period. Am J Surg 150:353–356
Andresen K, Bisgaard T, Kehlet H, Wara P, Rosenberg J (2014) Reoperation rates for laparoscopic versus open repair of femoral hernias in Denmark: a nationwide analysis. JAMA Surg 149:853–857
Bjork KJ, Mucha P Jr, Cahill DR (1988) Obturator hernia. Surg Gynecol Obstet 167:217–222
Ziegler DW, Rhoads JE Jr (1995) Obturator hernia needs a laparotomy, not a diagnosis. Am J Surg 170:67–68
Skandalakis LJSP, Gray SW (1995) Hernia. In: Nyhus LMCR (ed) Hernia O, J.B. Lippincott, Philadelphia, pp 425–439
Koch A, Edwards A, Haapaniemi S, Nordin P, Kald A (2005) Prospective evaluation of 6895 groin hernia repairs in women. Br J Surg 92:1553–1558
Yokoyama T, Kobayashi A, Kikuchi T, Hayashi K, Miyagawa S (2011) Transabdominal preperitoneal repair for obturator hernia. World J Surg 35:2323–2327
Gray SW, Skandalakis JE, Soria RE, Rowe JS Jr (1974) Strangulated obturator hernia. Surgery 75:20–27
Donahue PE (1995) Hernia. In: Nyhus LMCR (ed) Theoretic aspects of hernia. J.B. Lippincott, Philadelphia, pp 73–82
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Kentaro Fukushima, Takahide Yokoyama, Shiro Miwa, Hiroaki Motoyama, Takuma Arai, Noriyuki Kitagawa, Akira Shimizu, Tsuyoshi Notake, Toshiki Kikuchi, Akira Kobayashi, and Shin-ichi Miyagawa have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Fukushima, K., Yokoyama, T., Miwa, S. et al. Impact of age on groin hernia profiles observed during laparoscopic transabdominal preperitoneal hernia repair. Surg Endosc 33, 2602–2611 (2019). https://doi.org/10.1007/s00464-018-6556-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6556-7



