Abstract
Background
The fundamentals of laparoscopic surgery (FLS) trainer box, which is now established as a standard for evaluating minimally invasive surgical skills, consists of five tasks: peg transfer, pattern cutting, ligation, intra- and extracorporeal suturing. Virtual simulators of these tasks have been developed and validated as part of the Virtual Basic Laparoscopic Skill Trainer (VBLaST) (Arikatla et al. in Int J Med Robot Comput Assist Surg 10:344–355, 2014; Zhang et al. in Surg Endosc 27(10):3603–3615, 2013; Sankaranarayanan et al. in J Laparoendosc Adv Surg Tech 20(2):153–157, 2010; Qi et al. J Biomed Inform 75:48–62, 2017). The virtual task trainers have many advantages including automatic real-time objective scoring, reduced costs, and eliminating human proctors. In this paper, we extend VBLaST by adding two camera navigation system tasks: (a) pattern matching and (b) path tracing.
Methods
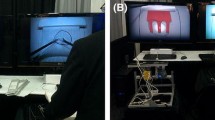
A comprehensive camera navigation simulator with two virtual tasks, simplified and cheaper hardware interface (compared to the prior version of VBLaST), graphical user interface, and automated metrics has been designed and developed. Face validity of the system is tested with medical students and residents from the University at Buffalo’s medical school.
Results
The subjects rated the simulator highly in all aspects including its usefulness in training to center the target and to teach sizing skills. The quality and usefulness of the force feedback scored the lowest at 2.62.











Similar content being viewed by others
References
Vanounou T et al (2010) Comparing the clinical and economic impact of laparoscopic versus open liver resection. Ann Surg Oncol 17(4):998–1009
Peters JH et al (2004) Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery 135(1):21–27
Fraser SA, Klassen DR, Feldman LS, Ghitulescu GA, Stanbridge D, Fried GM (2003) Evaluating laparoscopic skills: setting the pass/fail score for the MISTELS system. Surg Endosc 17(6):964–967
Vassiliou MC et al (2006) The MISTELS program to measure technical skill in laparoscopic surgery. Surg Endosc 20(5):744–747
Liu A, Tendick F, Cleary K, Kaufmann C (2003) A survey of surgical simulation: applications, technology, and education. Presence Teleoper Virtual Environ 12(6):599–614
Satava RM (2007) Historical review of surgical simulation—a personal perspective. World J Surg 32(2):141–148
Larsen CR, Oestergaard J, Ottesen BS, Soerensen JL (2012) The efficacy of virtual reality simulation training in laparoscopy: a systematic review of randomized trials. Acta Obstet Gynecol Scand 91(9):1015–1028
Ahlberg G et al (2007) Proficiency-based virtual reality training significantly reduces the error rate for residents during their first 10 laparoscopic cholecystectomies. Am J Surg 193(6):797–804
Jordan JA, Gallagher AG, McGuigan J, McClure N (2001) Virtual reality training leads to faster adaptation to the novel psychomotor restrictions encountered by laparoscopic surgeons. Surg Endosc 15(10):1080–1084
Seymour NE et al (2002) Virtual reality training improves operating room performance. Ann Surg 236(4):458–464
Maciel A, Liu Y, Ahn W, Singh TP, Dunnican W, De S (2008) Development of the VBLaST™: a virtual basic laparoscopic skill trainer. Int J Med Robot Comput Assist Surg 4(2):131–138
Arikatla VS, Ahn W, Sankaranarayanan G, De S (2014) Towards virtual FLS: development of a peg transfer simulator. Int J Med Robot Comput Assist Surg 10:344–355
Zhang L et al (2013) Characterizing the learning curve of the VBLaST-PT© (Virtual Basic Laparoscopic Skill Trainer). Surg Endosc 27(10):3603–3615
Sankaranarayanan G et al (2010) Preliminary face and construct validation study of a virtual basic laparoscopic skill trainer. J Laparoendosc Adv Surg Tech 20(2):153–157
Qi D, Panneerselvam K, Ahn W, Arikatla V, Enquobahrie A, De S (2017) Virtual interactive suturing for the fundamentals of laparoscopic surgery (FLS). J Biomed Inform 75:48–62
Stefanidis D et al (2007) Construct and face validity and task workload for laparoscopic camera navigation: virtual reality versus videotrainer systems at the SAGES Learning Center. Surg Endosc 21(7):1158–1164
Nilsson C et al (2017) Simulation-based camera navigation training in laparoscopy—a randomized trial. Surg Endosc 31(5):2131–2139
Ganai S, Donroe JA, St. Louis MR, Lewis GM, Seymour NE (2007) Virtual-reality training improves angled telescope skills in novice laparoscopists. Am J Surg 193(2):260–265
Korndorffer JR et al (2005) Development and transferability of a cost-effective laparoscopic camera navigation simulator. Surg Endosc 19(2):161–167
Bennett A, Birch DW, Menzes C, Vizhul A, Karmali S (2011) Assessment of medical student laparoscopic camera skills and the impact of formal camera training. Am J Surg 201(5):655–659
Richstone L, Schwartz MJ, Seideman C, Cadeddu J, Marshall S, Kavoussi LR (2010) Eye metrics as an objective assessment of surgical skill. Ann Surg 252(1):177–182
Mori M, Liao A, Hagopian TM, Perez SD, Pettitt BJ, Sweeney JF (2015) Medical students impact laparoscopic surgery case time. J Surg Res 197(2):277–282
Franzeck FM et al (2012) Prospective randomized controlled trial of simulator-based versus traditional in-surgery laparoscopic camera navigation training. Surg Endosc 26(1):235–241
Roch PJ et al (2018) Impact of visual–spatial ability on laparoscopic camera navigation training. Surg Endosc 32(3):1174–1183
Interactive Medical Simulation Toolkit (iMSTK) [Online] (2018). http://www.imstk.org/. Accessed 07 May 2018
Dawson SL, Kaufman JA (1998) The imperative for medical simulation. Proc IEEE 86(3):479–483
Fried GM et al (2004) Proving the value of simulation in laparoscopic surgery. Ann Surg 240(3):518–525 (discussion 525–528)
Watanabe Y et al (2015) Camera navigation and cannulation: validity evidence for new educational tasks to complement the Fundamentals of Laparoscopic Surgery Program. Surg Endosc 29(3):552–557
Kothari LG, Shah K, Barach P (2017) Simulation based medical education in graduate medical education training and assessment programs. Prog Pediatr Cardiol 44:33–42
Zhang A, Hünerbein M, Dai Y, Schlag P, Beller S (2008) Construct validity testing of a laparoscopic surgery simulator (Lap Mentor®). Surg Endosc 22(6):1440–1444
Epona Medical | LAP-X.” 13-May-2012
Iwata N et al (2011) Construct validity of the LapVR virtual-reality surgical simulator. Surg Endosc 25(2):423–428
Chellali A et al (2015) Preliminary evaluation of the pattern cutting and the ligating loop virtual laparoscopic trainers. Surg Endosc 29(4):815–821
Arikatla VS et al (2013) Face and construct validation of a virtual peg transfer simulator. Surg Endosc Other Interv Tech 27(5):1721–1729
Hwang H et al (2005) Correlating motor performance with surgical error in laparoscopic cholecystectomy. Surg Endosc 20:651–655
Acknowledgements
Research reported in this publication was supported by the National Institute of Biomedical Imaging And Bioengineering of the National Institutes of Health under Award Number R44EB019802. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding
National Institute of Biomedical Imaging and Bioengineering of the National Institutes of Health under Award Number R44EB019802.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Venkata Arikatla, Sam Horvath, Yaoyu Fu, Lora Cavuoto, Suvranu De, Steve Schwaitzberg, and Andinet Enquobahrie have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Arikatla, V., Horvath, S., Fu, Y. et al. Development and face validation of a virtual camera navigation task trainer. Surg Endosc 33, 1927–1937 (2019). https://doi.org/10.1007/s00464-018-6476-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6476-6