Abstract
Background
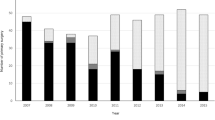
Laparoscopic surgery is frequently performed, and laparoscopic gastrectomy (LG) is also widely performed for gastric cancer. Elderly population with gastric cancer has increased in East Asia, including in Japan.
Methods
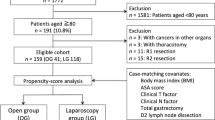
We examined 1131 patients with gastric cancer who underwent laparoscopic and open standard surgeries (OG). A total of 921 patients of age < 75 years (non-E group) and 210 patients of age ≥ 75 years (E group) underwent surgery for gastric cancer. The mortality, morbidity, and prognosis of LG and OG were compared by propensity score-matched analysis.
Results
Mortality and morbidity in the E group were significantly higher than those in the non-E group (p < 0.05). Propensity score-matching revealed that the incidence of postoperative complications of grade ≥ 2 in the OG subgroup was significantly higher than that in the LG subgroup in the E group (p < 0.05). The overall survival rate of the LG subgroup was significantly higher than that of the OG subgroup in both the non-E and E groups (p < 0.05). The depth of tumor invasion, lymph node metastasis, and the number of dissected lymph nodes were dependent factors for survival in the non-E group, whereas the depth of tumor invasion was the only dependent factor for survival in the E group in the multivariate analysis.
Conclusion
The survival rate of patients who underwent LG showed significantly good prognosis in both the non-E and E groups, although the E group patients who underwent OG subgroup showed higher severe complication incidences than those who underwent LG subgroup.



Similar content being viewed by others
References
Bertuccio P, Chatenoud L, Levi F, Praud D, Ferlay J, Negri E (2009) Recent patterns in gastric cancer: a global overview. Int J Cancer 125:666–673
Roder DM (2002) The epidemiology of gastric cancer. Gastric Cancer 5:5–11
Sierra A, Regueira FM, Hernández-Lizoáin JL, Pardo F, Martinez-Gonzalez MA, Javier A (2003) Role of the extended lymphadenectomy in gastric cancer surgery: experience in a single institution. Ann Surg Oncol 10:219–226
Roukos DH, Lorenz M, Encke A (1998) Evidence of survival benefit of extended (D2) lymphadenectomy in western patients with gastric cancer based on a new concept: a prospective long-term follow-up study. Surgery 123:573–578
Giovanetti M, Brotto AC, Tiberio GA, Campedelli L, Vettoretto N, Roncenti M, Di Flumeri G, Giulini SM (1999) D2 lymphectomy in the treatment of gastric cancer: a retrospective view on our experience (1990–1997). J Exp Clin Cancer Res 18:455–458
Okada Y (2013) Emergency medical services in a hyper-aged society. Nihon Rinsho 71:953–963
Polanczk CA, Marcantonio E, Goldman L, Rohde LE, Orav J, Mangione CM, Lee TH (2001) Impact of age on perioperative complications and length of stay in patients undergoing noncardiac surgery. Ann Intern Med 134:637–643
Ryynänen OP, Myllykangas M, Kinnunen J, Takala J (1997) Doctor’s willingness to refer elderly patients for elective surgery. Fam Pract 14:216–219
Monson K, Litvak DA, Bold RJ (2003) Surgery in the aged population: surgical oncology. Arch Surg 138:1061–1067
Story DA (2008) Postoperative complications on elderly patients and their significance for long-term prognosis. Curr Opin Anesthesiol 21:375–379
Kitano S, Iso Y, Moriyama M, Sugimachi K (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4:146–148
Fujiwara M, Kodera Y, Kasai Y, Kanyama Y, Hibi K, Ito K, Akiyama S, Nakao A (2003) Laparoscopy-assisted distal gastrectomy with systemic lymph node dissection for early gastric carcinoma: review of 43 cases. J Am Coll Surg 196:75–81
Uyama I, Sakurai Y, Komori Y, Nakamura Y, Syoji M, Tonomura S, Yoshida I, Masui T, Inaba K, Ochiai M (2005) Laparoscopy-assisted uncut Roux-en-Y operation after distal gastrectomy for gastric cancer. Gastric Cancer 8:253–257
Jeong O, Ryu SY, Zhao XF, Jung MR, Kim KY, Park YK (2012) Short-term survival outcomes and operative risks of laparoscopic total gastrectomy (LTG) for gastric carcinoma: experience at a large-volume center. Surg Endosc 26:3418–3425
Tanimura S, Higashino M, Fukunaga Y, Kishida S, Ogata A, Fujiwara Y, Osugi H (2006) Respiratory function after laparoscopic distal gastrectomy: an index of minimally invasive surgery. World J Surg 30:1211–1215
Huscher CG, Mingoli A, Sgarzini G, Sansonetti A, Di Paola M, Recher A, Ponzano C (2005) Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: 5-year results of a randomized prospective trial. Ann Surg 241:232–237
Kim MC, Kim KH, Kim HH, Jung GJ (2005) Comparison of laparoscopy-assisted by conventional open distal gastrectomy and extraperigastric lymph node dissection in early gastric cancer. J Surg Oncol 91:90–94
Kim MG, Yook JH, Kim KC, Kim TM, Kim HS, Kim BS, Kim BS (2011) Influence of obesity on early surgical outcomes of laparoscopic-assisted gastrectomy in gastric cancer. Surg Laparosc Endosc Percutan Tech 21:151–154
Weber KJ, Rey CD, Ganger M, Divino CM (2003) Comparison of laparoscopic and open gastrectomy for malignant disease. Surg Endosc 17:968–971
Varela JE, Hiyashi M, Nguyen T, Sabio A, Wilson SE, Nguyen NT (2006) Comparison of laparoscopic and open gastrectomy for gastric cancer. Am J Surg 192:837–842
Turrentine FE, Wang H, Simpson VB, Jones RS (2006) Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg 203:865–877
Wang JF, Zhang SZ, Zhang NY, Wu ZY, Feng JY, Ying LP, Zhang JJ (2016) Laparoscopic gastrectomy versus open gastrectomy for elderly patients with gastric cancer: a systemic review and meta-analysis. World J Surg Oncol 14:90–99
Yamamoto M, Kawano H, Yamaguchi S, Egashira A, Minami K, Morita M, Sakaguchi Y, Toh Y (2017) Technical and survival risks associated with esophagojejunostomy by laparoscopic total gastrectomy for gastric carcinoma. Surg Laparosc Endosc Percutan Tech 27:197–202
Jeong O, Park YK (2009) Intracorporeal circular stapling esophagojejunostomy using the transorally inserted anvil (OrVil) after laparoscopic total gastrectomy. Surg Endosc 23:2624–2630
Japanese Classification of Gastric Carcinoma (2010) Japanese Gastric Cancer Association. 14th edn, Kanehara, Fukuoka
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Jeong O, Jung MR, Kim GY, Kim HS, Ryu SY, Park YK (2013) Comparison of short-term surgical outcomes between laparoscopic and open total gastrectomy for gastric carcinoma; case-control study using propensity score matching method. J Am Coll Surg 216:184–191
Katai H, Sasako M, Sano T, Fukagawa T (2004) Gastric cancer surgery in the elderly without operative mortality. Surg Oncol 13:235–238
Marugame T, Dongmeri Q (2007) Comparison of time trends in stomach cancer incidence (1973–1997) in East Asia. Europe and USA, from Cancer incidence in five continents. Vol. IV–VIII. Jpn J Clin Oncol 37:242–243
Evers BM, Townsend CM Jr, Thompson JC (1994) Organ physiology of aging. Surg Clin North Am 74:23–39
Fujisaki M, Shinohara T, Hanyu N, Kawano S, Tanaka Y, Watanabe Y, Yanaga K (2016) Laparoscopic gastrectomy for gastric cancer in elderly patients. Surg Endosc 30:1380–1387
Ueno D, Matsumoto H, Kubota H, Higashi M, Akiyama T, Shiotani A, Hirai T (2017) Prognostic factors for gastrectomy in elderly patients with gastric cancer. World J Surg Oncol. https://doi.org/10.1186/s12957-017-1131-6
Miki Y, Makuuchi R, Honda S, Tokunaga M, Tanizawa Y, Bando E, Kawamura T, Yurikusa T, Tanuma A, Terashima M (2017) Prospective phase II study evaluating the efficacy of swallow ability screening tests and pneumonia prevention using a team approach for elderly patients with gastric cancer. Gastric Cancer. https://doi.org/10.1007/s10120-017-0736-3
Yoshida M, Koga S, Ishimaru K, Yamamoto Y, Matsui Y, Akita S, Kuwabara J, Tanigawa K, Watanabe Y (2017) Laparoscopic-assisted distal gastrectomy is feasible also for elderly patients aged 80 years and over: effectiveness and long-term prognosis. Surg Endosc. https://doi.org/10.1007/s00464-017-5493-1
Konishi H, Ichikawa D, Itoh H, Fukuda K, Kakihara N, Takemura M, Okugawa K, Uchiyama K, Nakata M, Nishi H, Kosuga T, Komatsu S, Okamoto K, Otsuji E (2017) Surgery for gastric cancer patients of age 85 and older: multicenter survey. World J Gastroenterol 23:1215–1223
Kim MC, Jung GJ, Kim HH (2007) Morbidity and mortality of laparoscopy-assisted gastrectomy with extraperigastric lymph node dissection for gastric cancer. Dig Dis Sci 52:543–548
Zeng YK, Yang ZL, Peng JS, Lin HS, Cai S (2012) Laparoscopy-assisted versus open distal gastrectomy for early gastric cancer: evidence from randomized and nonrandomized clinical trials. Ann Surg 256:39–52
Kim W, Kim HH, Han SU, Kim MC, Hyung WJ, Ryu SW, Cho GS, Kim CY, Yang HK, Park DJ, Song KY, Lee SI, Ryu SY, Lee JH, Lee HJ (2016) Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: Short-term outcomes from a multicenter randomized controlled trial (KLASS-01). Ann Surg 263:28–35
Meng CY, Lin JX, Huang CM, Zeng CH, Li P, Xie JW, Wnag JB (2012) Laparoscopy-assisted radical gastrectomy with D2 lymph node dissection for gastric cancer in the elderly. Zhonghua Wei Chang Wai Ke Za Zhi 15:152–156
Hu JH, Yang DS, Zheng L, Li SJ, Wang CY, Ren XQ (2013) Study on the application of laparoscopy-assisted radical gastrectomy for gastric cancer in the elderly. Zhonghua Wei Chang Wai Ke Za Zhi 16:1092–1095
Biffi R, Botteri E, Cenciarelli S, Luca F, Pazzi S, Valvo M, Sonzogni A, Chiappa A, Leal Ghezzi T, Rotmensz N, Banardi V, Andreoni B (2011) Impact on survival of the number of lymph nodes removed in patients with node-negative gastric cancer submitted to extended lymph node dissections. Eur J Surg Oncol 37:305–311
Ling J, Wang C, Wang X, Shen Z, Chen W, Qin J, Qin X, Shen K, Sun Y, Liu F (2014) Impact of the number of lymph nodes dissected on the prognosis of G3 advanced gastric cancer. Zhonghua Wei Chang Wai Ke Za Zhi 17:667–671
Lu J, Huang C-M, Zheng C-H, Li P, Xie JW, Wang JB, Lin JX, Chen QY, Cao LL, Lin M (2015) Short- and long-term outcome after laparoscopic versus open total gastrectomy for elderly gastric cancer patients: a propensity score-matched analysis. J Gastrointest Surg 19:1949–1957
Zong L, Wu A, Wang W, Deng J, Aikou S, Yamashita H, Maeda M, Abe M, Yu D, Jiang Z, Seto Y, Ji J (2017) Feasibility of laparoscopic gastrectomy for elderly gastric cancer patients: meta-analysis of non-randomized controlled studies. Oncotarget 8:51878–51887
Acknowledgements
This work was supported, in part, by a Grant-in Aid from the Ministry of Education, Culture, Sport, Science and Technology of Japan (Grant No. 16K10525), and the Uehara Memorial Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Manabu Yamamoto, Mototsugu Shimokawa, Hiroyuki Kawano, Mitsuhiko Ohta, Daisuke Yoshida, Kazuhito Minami, Masahiko Ikebe, Masaru Morita, and Yasushi Toh have no conflict of interest to disclose.
Rights and permissions
About this article
Cite this article
Yamamoto, M., Shimokawa, M., Kawano, H. et al. Benefits of laparoscopic surgery compared to open standard surgery for gastric carcinoma in elderly patients: propensity score-matching analysis. Surg Endosc 33, 510–519 (2019). https://doi.org/10.1007/s00464-018-6325-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6325-7