Abstract
Background
There is limited and conflicting data on the optimal intervention for the treatment of achalasia in adolescents and young adults (AYA), Heller myotomy (HM), esophageal dilation (ED) or botulinum toxin injection (botox). The goal of this study is to determine the most appropriate index intervention for achalasia in the AYA population.
Methods
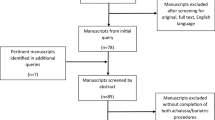
We completed a longitudinal, population-based analysis of the California (2005–2010) and New York (1999–2014) statewide databases. We included patients 9–25 years old with achalasia who underwent HM, ED or botox. Comparisons were made based on the patients’ index procedure. Rates of 30-day complications, long-term complications, and re-intervention up to 14 years were calculated. Cox regression was performed to determine the risk of re-intervention, adjusting for patient demographics.
Results
A total of 442 AYAs were analyzed, representing the largest cohort of young patients with this disease studied to date. Median follow-up was 5.2 years (IQR 1.8–8.0). The overall rate of re-intervention was 29.3%. Rates of re-intervention for ED and botox were equivalent and higher than HM (65.0% for ED, 47.4% for botox and 16.4% for HM, p < 0.001). Ultimately, 46.9% of ED and botox patients underwent HM. The overall short-term complication rate was 4.3% and long-term, 1.9%. There was no difference in the short-term and long-term complication rates between intervention groups (p > 0.05). On adjusted analysis, ED and botox were associated with increased risks of re-intervention when compared to HM (HR 5.9, HR 4.8, respectively, p < 0.01). Black patients were found to have a risk of re-intervention twice that of white patients (HR 2.0, p = 0.05).
Conclusions
HM has a similar risk of complications but a significantly lower risk of re-intervention when compared to ED and botox. Based on our findings, we recommend HM as the optimal index procedure for AYAs with achalasia.

Similar content being viewed by others
References
Marlais M et al., UK incidence of achalasia: an 11-year national epidemiological study. Arch Dis Child, 2010: p. archdischild171975
Smits M et al (2016) Pediatric achalasia in the Netherlands: incidence, clinical course, and quality of life. J Pediatr 169:110–115.e3
Mayberry J (2001) Epidemiology and demographics of achalasia. Gastrointest Endosc Clin N Am. 11(2): 235–248
Sonnenberg A (2009) Hospitalization for achalasia in the United States 1997–2006. Dig Dis Sci 54(8):1680–1685
Hallal C et al (2012) Diagnosis, misdiagnosis, and associated diseases of achalasia in children and adolescents: a twelve-year single center experience. Pediatr Surg Int 28(12):1211–1217
Molena D et al (2015) Hospitalization for esophageal achalasia in the United States. World J Gastrointest Endosc 7(13):1096–1102
Lee CW et al (2010) Outcomes of treatment of childhood achalasia. J Pediatr Surg 45(6):1173–1177
Hussain SZ, Thomas R, Tolia V (2002) A review of achalasia in 33 children. Dig Dis Sci 47(11):2538–2543
Sharp NE, St Peter SD (2016) Treatment of idiopathic achalasia in the pediatric population: a systematic review. Eur J Pediatr Surg 26(2):143–149
Zhang Y et al (2009) Diagnosis and management of esophageal achalasia in children: analysis of 13 cases. World J Pediatr 5(1):56–59
Grabowski A et al (2017) Pediatric achalasia. Single-center study of interventional treatment. Prz Gastroenterol 12(2):98
Markar SR et al (2018) Population-based cohort study of surgical myotomy and pneumatic dilatation as primary interventions for oesophageal achalasia. Br J Surg 105(8):1028–1035
Ehlers AP et al, Treatment A (2017) Outcomes, utilization, and costs: a population-based study from the United States. J Am Coll Surg 225(3):380–386
Boeckxstaens GE et al (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364(19):1807–1816
Campos GM et al (2009) Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 249:45–47
Cheng J-W et al. (2017) Laparoscopic Heller myotomy is not superior to pneumatic dilation in the management of primary achalasia: conclusions of a systematic review and meta-analysis of randomized controlled trials. Medicine. 96(7): e5525
Schoenberg MB et al (2013) Laparoscopic Heller myotomy versus endoscopic balloon dilatation for the treatment of achalasia: a network meta-analysis. Ann Surg 258(6):943–952
Persson J et al (2015) Treatment of achalasia with laparoscopic myotomy or pneumatic dilatation: long-term results of a prospective, randomized study. World J Surg 39(3):713–720
Pacilli M, Davenport M (2017) Results of laparoscopic Heller’s myotomy for achalasia in children: a systematic review of the literature. J Laparoendosc Adv Surg Tech 27(1):82–90
Cowgill SM et al (2007) Difficult myotomy is not determined by preoperative therapy and does not impact outcome. JSLS 11(3):336
Patti MG et al (1999) Effects of previous treatment on results of laparoscopic Heller myotomy for achalasia. Dig Dis Sci 44(11):2270–2276
Bloomston M et al (2003) Preoperative intervention does not affect esophageal muscle histology or patient outcomes in patients undergoing laparoscopic Heller myotomy. J Gastrointest Surg 7(2):181–190
Smith CD et al., Endoscopic therapy for achalasia before Heller myotomy results in worse outcomes than Heller myotomy alone. Ann Surg 2006. 243(5):579
Berquist WE et al (1983) Achalasia: diagnosis, management, and clinical course in 16 children. Pediatrics 71(5):798–805
Franklin AL, Petrosyan M, Kane TD (2014) Childhood achalasia: a comprehensive review of disease, diagnosis and therapeutic management. World J Gastrointest Endosc 6(4):105
Corda L et al (2010) Laparoscopic oesophageal cardiomyotomy without fundoplication in children with achalasia: a 10-year experience. Surg Endosc 24(1):40–44
Di Nardo G et al (2012) Pneumatic balloon dilation in pediatric achalasia: efficacy and factors predicting outcome at a single tertiary pediatric gastroenterology center. Gastrointest Endosc 76(5):927–932
Author information
Authors and Affiliations
Contributions
Dr. Kelleher conceptualized the study, critically reviewed the data and drafted the initial manuscript, and reviewed and revised the final manuscript. Dr. Hung and Dr. Chang conceptualized the study, collected the data and carried out the initial data analysis, critically reviewed the data and drafted the initial manuscript, and reviewed and revised the final manuscript. Dr. Westfal critically reviewed the data, reviewed and revised the initial and final manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Disclosures
ML Westfal is financially supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (Award Number: T32 DK007754) and by the Massachusetts General Hospital Department of Surgery Marshall K. Bartlett Fellowship. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Y-C Hung, DC Chang, CM Kelleher have no conflicts of interest or financial ties to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hung, YC., Westfal, M.L., Chang, D.C. et al. Heller myotomy is the optimal index procedure for esophageal achalasia in adolescents and young adults. Surg Endosc 33, 3355–3360 (2019). https://doi.org/10.1007/s00464-018-06625-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-06625-6