Abstract
Background
Esophageal achalasia is a rare disease and there have been very few reports about it, especially in children. We reviewed our experience in dealing with esophageal achalasia in 13 children.
Methods
Thirteen children (6 boys and 7 girls), who had been diagnosed with achalasia over a 12-year period between May 1993 and October 2005, were analysed with regard to clinical manifestations, esophageal manometry, endoscopic findings, and treatment. Their age ranged from 3 years to 14 years and 5 months (average 10.3 years) at the time of diagnosis.
Results
In the 13 children, 3 had a family history of esophageal achalasia, 2 of them were sisters. All the 3 children suffered from achalasia/alacrimia/ACTH deficiency. Dysphagia was the most common symptom in the affected children. Vomiting/regurgitation, retrosternal pain, retarded growth, and respiratory symptoms were also observed in some patients. Heller’s esophagocardiomyotomy was performed in 9 (69.23%) children, among whom 3 had an antireflux operation at the same time. In the remaining 4 children, 3 received a pneumatic dilatation and 1 received regular administration of nifedipine. Twelve patients were followed up: 8 patients by surgery were cured and have been in perfect condition until now, 3 patients recovered fairly, and 1 patient showed improvement.
Conclusions
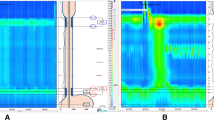
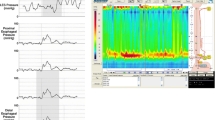
Esophageal manometry combined with X-ray examination proves to be an effective diagnostic method for achalasia. It is also effective in evaluating the result of treatment. Heller’s esophagocardiomyotomy is a treatment of choice for children with achalasia because of its safety and long-term effective results after surgery.
Similar content being viewed by others
References
Mayberry JF, Mayell MJ. Epidemiological study of achalasia in children. Gut 1988;29:90–93.
Willis T. The companation of madication and surgery of esophageal achalasia. In: Willis T, eds. Achalasia. London: Hgas-comitis, 1674: 18–19.
Goldblum JR, Rice TW, Richter JE. Histopathologic features in esophagomyotomy specimens from patients with achalasia. Gastroenterology 1996;111:648–654.
Kahrilas PJ. Esophageal motility disorders: current concepts of pathogenesis and treatment. Can J Gastroenterol 2000;14:221–231.
Smith CD, Stival A, Howell DL, Swafford V. Endoscopic therapy for achalasia before Heller myotomy results in worse outcomes than heller myotomy alone. Ann Surg 2006;243:579–584.
Hunter JG, Trus TL, Branum GD, Waring JP. Laparoscopic Heller myotomy and fundoplication for achalasia. Ann Surg 1997;225:655–664.
Asch MJ, Liebman W, Lachman RS. Esophageal achalasia: diagnosis and cardiomyotomy in a newborn infant. J Pediatr Surg 1974;9:911–915.
Myers NA, Jolley SG, Taylor R. Achalasia of the cardia in children: a worldwide survey. J Pediatr Surg 1994;29:1375–1379.
Jara FM, Toledo-Pereyra LH, Lewis JW, Magilligan DJ Jr. Long-term results of esophagomyotomy for achalasia of esophagus. Arch Surg 1979;114:935–936.
Okike N, Payne WS, Neufeld DM, Bernatz PE, Pairolero PC, Sanderson DR. Esophagomyotomy versus forceful dilation for achalasia of the esophagus: results in 899 patients. Ann Thorac Surg 1979;28:119–125.
Hussain SZ, Thomas R, Tolia V. A review of achalasia in 33 children. Dig Dis Sci 2002;47:2538–2543.
Mukhopadhya A, Danda S, Huebner A, Chacko A. Mutations of the AAAS gene in an Indian family with Allgrove’s syndrome. World J Gastroenterol 2006;12:4764–4766.
Sellami D, Bouacida W, Frikha F. Allgrove syndrome. Report on a family. J Fr Ophtalmol 2006;29:4184–4221.
Ragunath K, Williams JG. A review of oesophageal manometry testing in a district general hospital. Postgraol Med J 2002;78:34–36.
Mehta R, John A, Sadasivan S, Mustafa CP, Nandkumar R, Raj VV, et al. Factors determining successful outcome following pneumatic balloon dilation in achalasia cardia. Indian J Gastroenterol 2005;24:243–245.
Boyle JT, Cohen S, Watkins JB. Successful treatment of achalasia in childhood by pneumatic dilation. J Pediatr 1981;99:35–40.
Heller E. Extramukose cardioplastik beim chronischen cardiospasmus mit dilation des esophagus. Mitt Grenzgeb Med Chir 1914;27:141.
Zaaijer J. Cardiospasm in the aged. Ann Surg 1923;77:615–617.
Ortiz A, de Haro LF, Parrilla P, Lage A, Perez D, Munitiz V, et al. Very long-term objective evaluation of heller myotomy plus posterior partial fundoplication in patients with achalasia of the cardia. Ann Surg 2008;247:258–264.
Bonavina L. Minimally invasive surgery for esophageal achalasia. World J Gastroenterol 2006;12:5921–5925.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Y., Xu, CD., Zaouche, A. et al. Diagnosis and management of esophageal achalasia in children: analysis of 13 cases. World J Pediatr 5, 56–59 (2009). https://doi.org/10.1007/s12519-009-0010-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-009-0010-9