Abstract
Background
Prolonged postoperative ileus (PPOI) is a common complication after colorectal resection but data regarding PPOI risk factors after laparoscopic rectal cancer surgery is lacking. This study aimed to identify risk factors for PPOI after laparoscopic sphincter-saving total mesorectal excision (TME) for cancer.
Methods
All patients who underwent a laparoscopic sphincter-saving TME for cancer from 2005 to 2014 were identified from our prospective database. PPOI was defined as abdominal distension, nausea, and/or vomiting, requiring a nasogastric tube insertion, during the postoperative period.
Results
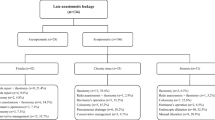
Among 428 consecutive patients, 65 patients (15%) presented with POI. In multivariate analysis, male gender (Odds Ratio (OR) 2.3 [1.1–4.5]; p = 0.026, age >70 years (OR: 2.0 [1.1–4.0]; p = 0.037)], conversion to open approach (OR 4.9 [1.5–15.4]; p = 0.007), and intra-abdominal surgical site infection (OR 3.8 [1.9–7.5]; p < 0.001) were identified as independent risk factor for PPOI. PPOI risk was 5% in patients without any risk factor but raised to 11, 28, and 54% in patients with 1, 2, or ≥3 risk factors, respectively (p < 0.001).
Conclusion
PPOI is observed in 15% of the patients after laparoscopic sphincter-saving surgery for rectal cancer. We identified four independent factors for PPOI in multivariate analysis: male, gender, age >70, conversion to open approach, and intra-abdominal surgical site infection, leading to the construction of a simple and pragmatic predictive score. This score might help the surgeon to assess patient at risk of PPOI.

Similar content being viewed by others
References
Holte K, Kehlet H (2000) Postoperative ileus: a preventable event. Br J Surg 87:1480–1493
Iyer S, Saunders WB, Stemkowski S (2009) Economic burden of postoperative ileus associated with colectomy in the United States. J Manag Care Pharm 15:485–494
Moghadamyeghaneh Z, Hwang GS, Hanna MH, Phelan M, Carmichael JC, Mills S, Pigazzi A, Stamos MJ (2016) Risk factors for prolonged ileus following colon surgery. Surg Endosc 30:603–609
Chapuis PH, Bokey L, Keshava A, Rickard MJ, Stewart P, Young CJ, Dent OF (2013) Risk factors for prolonged ileus after resection of colorectal cancer: an observational study of 2400 consecutive patients. Ann Surg 257:909–915
Wolthuis AM, Bislenghi G, Fieuws S, de Buck van Overstraeten A, Boeckxstaens G, D’Hoore A (2016) Incidence of prolonged postoperative ileus after colorectal surgery: a systematic review and meta-analysis. Colorectal Dis 18:O1–O9
Stewart RM, Page CP, Brender J, Schwesinger W, Eisenhut D (1987) The incidence and risk of early postoperative small bowel obstruction. A cohort study. Am J Surg 154:643–647
Ellozy SH, Harris MT, Bauer JJ, Gorfine SR, Kreel I (2002) Early postoperative small-bowel obstruction: a prospective evaluation in 242 consecutive abdominal operations. Dis Colon Rectum 45:1214–1217
Artinyan A, Nunoo-Mensah JW, Balasubramaniam S, Gauderman J, Essani R, Gonzalez-Ruiz C, Kaiser AM, Beart RW Jr (2008) Prolonged postoperative ileus-definition, risk factors, and predictors after surgery. World J Surg 32:1495–1500
Kehlet H, Holte K (2001) Review of postoperative ileus. Am J Surg 182:3S–10S
Millan M, Biondo S, Fraccalvieri D, Frago R, Golda T, Kreisler E (2012) Risk factors for prolonged postoperative ileus after colorectal cancer surgery. World J Surg 36:179–185
Kronberg U, Kiran RP, Soliman MS, Hammel JP, Galway U, Coffey JC, Fazio VW (2011) A characterization of factors determining postoperative ileus after laparoscopic colectomy enables the generation of a novel predictive score. Ann Surg 253:78–81
Schwenk W, Haase O, Neudecker J, Muller JM (2005) Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. doi:10.1002/14651858.CD003145.pub2
van der Pas MH, Haglind E, Cuesta MA, Furst A, Lacy AM, Hop WC, Bonjer HJ, Group COcLoORIS (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14:210–218
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy AM, Group COcLoORS (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Shussman N, Brown MR, Johnson MC, Da Silva G, Wexner SD, Weiss EG (2013) Does nasogastric tube decompression get used less often with laparoscopic and hand-assisted compared with open colectomy? Surg Endosc 27:4564–4568
Chen HH, Wexner SD, Iroatulam AJ, Pikarsky AJ, Alabaz O, Nogueras JJ, Nessim A, Weiss EG (2000) Laparoscopic colectomy compares favorably with colectomy by laparotomy for reduction of postoperative ileus. Dis Colon Rectum 43:61–65
Kanso F, Maggiori L, Debove C, Chau A, Ferron M, Panis Y (2015) Perineal or abdominal approach first during intersphincteric resection for low rectal cancer: which is the best strategy? Dis Colon Rectum 58:637–644
Maggiori L, Bretagnol F, Aslam MI, Guedj N, Zappa M, Ferron M, Panis Y (2014) Does pathologic response of rectal cancer influence postoperative morbidity after neoadjuvant radiochemotherapy and total mesorectal excision? Surgery 155:468–475
Kehlet H, Wilmore DW (2002) Multimodal strategies to improve surgical outcome. Am J Surg 183:630–641
Diemunsch P (2008) Conference of experts–short text. Management of postoperative nausea and vomiting. French Society of Anesthesia and Resuscitation. Ann Fr Anesth Reanim 27:866–878
Bretagnol F, Panis Y, Rullier E, Rouanet P, Berdah S, Dousset B, Portier G, Benoist S, Chipponi J, Vicaut E, French Research Group of Rectal Cancer Surgery (2010) Rectal cancer surgery with or without bowel preparation: The French GRECCAR III multicenter single-blinded randomized trial. Ann Surg 252:863–868
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
Rahbari NN, Weitz J, Hohenberger W, Heald RJ, Moran B, Ulrich A, Holm T, Wong WD, Tiret E, Moriya Y, Laurberg S, den Dulk M, van de Velde C, Buchler MW (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 147:339–351
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457
Masoomi H, Kang CY, Chaudhry O, Pigazzi A, Mills S, Carmichael JC, Stamos MJ (2012) Predictive factors of early bowel obstruction in colon and rectal surgery: data from the Nationwide Inpatient Sample, 2006–2008. J Am Coll Surg 214:831–837
Vather R, Josephson R, Jaung R, Robertson J, Bissett I (2015) Development of a risk stratification system for the occurrence of prolonged postoperative ileus after colorectal surgery: a prospective risk factor analysis. Surgery 157:764–773
Delaney CP, Marcello PW, Sonoda T, Wise P, Bauer J, Techner L (2010) Gastrointestinal recovery after laparoscopic colectomy: results of a prospective, observational, multicenter study. Surg Endosc 24:653–661
Kalff JC, Carlos TM, Schraut WH, Billiar TR, Simmons RL, Bauer AJ (1999) Surgically induced leukocytic infiltrates within the rat intestinal muscularis mediate postoperative ileus. Gastroenterology 117:378–387
Alves A, Panis Y, Pocard M, Regimbeau JM, Valleur P (1999) Management of anastomotic leakage after nondiverted large bowel resection. J Am Coll Surg 189:554–559
Goettsch WG, Sukel MP, van der Peet DL, van Riemsdijk MM, Herings RM (2007) In-hospital use of opioids increases rate of coded postoperative paralytic ileus. Pharmacoepidemiol Drug Saf 16:668–674
Vlug MS, Wind J, Hollmann MW, Ubbink DT, Cense HA, Engel AF, Gerhards MF, van Wagensveld BA, van der Zaag ES, van Geloven AA, Sprangers MA, Cuesta MA, Bemelman WA (2011) Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann Surg 254:868–875
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Elisabeth Hain, Léon Maggiori, Cécile Mongin, Justine Prost a la Denise, and Yves Panis have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Hain, E., Maggiori, L., Mongin, C. et al. Risk factors for prolonged postoperative ileus after laparoscopic sphincter-saving total mesorectal excision for rectal cancer: an analysis of 428 consecutive patients. Surg Endosc 32, 337–344 (2018). https://doi.org/10.1007/s00464-017-5681-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5681-z