Abstract
Introduction
Recent studies show contrasting data on the impact of laparoscopy on long-term complications such as the occurrence of small bowel obstruction (SBO) and incisional hernia (IH). The objective of the study was to assess the impact of the laparoscopic approach on the occurrence of SBO and IH after colorectal resection.
Methods
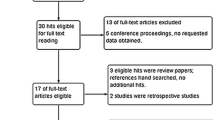
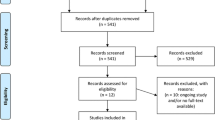
Two trained investigators independently searched MEDLINE, Embase, PubMed, and the Cochrane Central Register of clinical trials for studies comparing laparoscopy to open surgery for mid- to long-term outcomes after colorectal surgery. No language restriction was set. Sensitivity analyses for study design and quality, conversion rate, type of procedure (colon or rectal surgery), and length of follow-up were performed.
Results
Eleven RCTs and 14 non-RCT comparative studies for a total of 6540 patients were included in the analysis. Laparoscopy was associated with a significant reduction in the occurrence of SBO (RR 0.57, [95 %CI 0.42–0.76], 16 trials) and IH (RR 0.60, [95 %CI 0.50–0.72], 19 trials). Sensitivity analysis including only RCTs confirmed the reduction in SBO (RR 0.58, [95 %CI 0.39–0.87], 8 trials), while the difference was close to significance for IH (RR 0.76, [95 %CI 0.56–1.03], 7 trials). Sensitivity analysis including only studies with conversion rate lower than 15 % showed a significant protective effect of laparoscopy for both SBO (RR 0.53, [95 %CI 0.37–0.77], 11 trials) and IH (RR 0.58, [95 %CI 0.47–0.72], 12 trials). No significant difference between laparoscopy and open surgery was found when the analysis was limited to studies with conversion rate >15 % (SBO: RR 0.60 [0.32–1.12], IH: RR 0.70 [0.46–1.06]). Length of follow-up did not substantially impact on results.
Conclusion
Laparoscopic surgery is associated with a significant reduction in both SBO and IH compared to the open approach. A low conversion rate in the laparoscopic group plays a key role for reduction in both SBO and IH.









Similar content being viewed by others
References
Schwenk W, Haase O, Neudecker J, Muller JM (2005) Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. doi:10.1002/14651858.CD003145.pub2
Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, Lacy AM, Bemelman WA, Andersson J, Angenete E, Rosenberg J, Fuerst A, Haglind E, Group CIS (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, Choi HS, Kim DW, Chang HJ, Kim DY, Jung KH, Kim TY, Kang GH, Chie EK, Kim SY, Sohn DK, Kim DH, Kim JS, Lee HS, Kim JH, Oh JH (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
Bartels SA, Vlug MS, Hollmann MW, Dijkgraaf MG, Ubbink DT, Cense HA, van Wagensveld BA, Engel AF, Gerhards MF, Bemelman WA, Collaborative LSG (2014) Small bowel obstruction, incisional hernia and survival after laparoscopic and open colonic resection (LAFA study). Br J Surg 101:1153–1159
Scholin J, Buunen M, Hop W, Bonjer J, Anderberg B, Cuesta M, Delgado S, Ibarzabal A, Ivarsson ML, Janson M, Lacy A, Lange J, Pahlman L, Skullman S, Haglind E (2011) Bowel obstruction after laparoscopic and open colon resection for cancer: results of 5 years of follow-up in a randomized trial. Surg Endosc 25:3755–3760
Taylor GW, Jayne DG, Brown SR, Thorpe H, Brown JM, Dewberry SC, Parker MC, Guillou PJ (2010) Adhesions and incisional hernias following laparoscopic versus open surgery for colorectal cancer in the CLASICC trial. Br J Surg 97:70–78
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100
Schardt C, Adams MB, Owens T, Keitz S, Fontelo P (2007) Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak 7:16
Robinson KA, Dickersin K (2002) Development of a highly sensitive search strategy for the retrieval of reports of controlled trials using PubMed. Int J Epidemiol 31:150–153
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed) 343:d5928
Savovic J, Weeks L, Sterne JA, Turner L, Altman DG, Moher D, Higgins JP (2014) Evaluation of the Cochrane Collaboration’s tool for assessing the risk of bias in randomized trials: focus groups, online survey, proposed recommendations and their implementation. Syst Rev 3:37
Mudge M, Hughes LE (1985) Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg 72:70–71
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L (2006) Comparison of two methods to detect publication bias in meta-analysis. JAMA 295:676–680
Ng SS, Lee JF, Yiu RY, Li JC, Hon SS, Mak TW, Ngo DK, Leung WW, Leung KL (2014) Laparoscopic-assisted versus open total mesorectal excision with anal sphincter preservation for mid and low rectal cancer: a prospective, randomized trial. Surg Endosc 28:297–306
Ng SS, Leung KL, Lee JF, Yiu RY, Li JC, Hon SS (2009) Long-term morbidity and oncologic outcomes of laparoscopic-assisted anterior resection for upper rectal cancer: ten-year results of a prospective, randomized trial. Dis Colon Rectum 52:558–566
Braga M, Pecorelli N, Frasson M, Vignali A, Zuliani W, Carlo VD (2011) Long-term outcomes after laparoscopic colectomy. World J Gastrointest Oncol 3:43–48
Eshuis EJ, Slors JF, Stokkers PC, Sprangers MA, Ubbink DT, Cuesta MA, Pierik EG, Bemelman WA (2010) Long-term outcomes following laparoscopically assisted versus open ileocolic resection for Crohn’s disease. Br J Surg 97:563–568
Gervaz P, Mugnier-Konrad B, Morel P, Huber O, Inan I (2011) Laparoscopic versus open sigmoid resection for diverticulitis: long-term results of a prospective, randomized trial. Surg Endosc 25:3373–3378
Polle SW, Dunker MS, Slors JF, Sprangers MA, Cuesta MA, Gouma DJ, Bemelman WA (2007) Body image, cosmesis, quality of life, and functional outcome of hand-assisted laparoscopic versus open restorative proctocolectomy: long-term results of a randomized trial. Surg Endosc 21:1301–1307
Stocchi L, Milsom JW, Fazio VW (2008) Long-term outcomes of laparoscopic versus open ileocolic resection for Crohn’s disease: follow-up of a prospective randomized trial. Surgery 144:622–627 (discussion 627–628)
Winslow ER, Fleshman JW, Birnbaum EH, Brunt LM (2002) Wound complications of laparoscopic vs open colectomy. Surg Endosc 16:1420–1425
Andersen LP, Klein M, Gogenur I, Rosenberg J (2008) Incisional hernia after open versus laparoscopic sigmoid resection. Surg Endosc 22:2026–2029
Champault GG, Barrat C, Raselli R, Elizalde A, Catheline JM (2002) Laparoscopic versus open surgery for colorectal carcinoma: a prospective clinical trial involving 157 cases with a mean follow-up of 5 years. Surg Laparosc Endosc Percutan Tech 12:88–95
Duepree H-J, Senagore AJ, Delaney CP, Fazio VW (2003) Does means of access affect the incidence of small bowel obstruction and ventral hernia after bowel resection? J Am Coll Surg 197:177–181
Eshuis EJ, Polle SW, Slors JF, Hommes DW, Sprangers MA, Gouma DJ, Bemelman WA (2008) Long-term surgical recurrence, morbidity, quality of life, and body image of laparoscopic-assisted vs. open ileocolic resection for Crohn’s disease: a comparative study. Dis Colon Rectum 51:858–867
Franklin ME Jr, Rosenthal D, Abrego-Medina D, Dorman JP, Glass JL, Norem R, Diaz A (1996) Prospective comparison of open vs. laparoscopic colon surgery for carcinoma. Five-year results. Dis Colon Rectum 39:S35–S46
Ihedioha U, Mackay G, Leung E, Molloy RG, O’Dwyer PJ (2008) Laparoscopic colorectal resection does not reduce incisional hernia rates when compared with open colorectal resection. Surg Endosc 22:689–692
Kellokumpu IH, Kairaluoma MI, Nuorva KP, Kautiainen HJ, Jantunen IT (2012) Short- and long-term outcome following laparoscopic versus open resection for carcinoma of the rectum in the multimodal setting. Dis Colon Rectum 55:854–863
Laurent C, Leblanc F, Bretagnol F, Capdepont M, Rullier E (2008) Long-term wound advantages of the laparoscopic approach in rectal cancer. Br J Surg 95:903–908
Llaguna OH, Avgerinos DV, Lugo JZ, Matatov T, Abbadessa B, Martz JE, Leitman IM (2010) Incidence and risk factors for the development of incisional hernia following elective laparoscopic versus open colon resections. Am J Surg 200:265–269
Makni A, Chebbi F, Ksantini R, Fetirich F, Bedioui H, Jouini M, Kacem M, Ben Mami N, Filali A, Ben Safta Z (2013) Laparoscopic-assisted versus conventional ileocolectomy for primary Crohn’s disease: results of a comparative study. J Visc Surg 150:137–143
Patankar SK, Larach SW, Ferrara A, Williamson PR, Gallagher JT, DeJesus S, Narayanan S (2003) Prospective comparison of laparoscopic vs. open resections for colorectal adenocarcinoma over a ten-year period. Dis Colon Rectum 46:601–611
Pereira JA, Pera M, Grande L (2013) Incidence of incisional hernia after open and laparoscopic colorectal cancer resection. Cir Esp 91:44–49
Saklani AP, Naguib N, Shah PR, Mekhail P, Winstanley S, Masoud AG (2013) Adhesive intestinal obstruction in laparoscopic vs open colorectal resection. Colorectal Dis 15:80–84
Vignali A, De Nardi P, Ghirardelli L, Di Palo S, Staudacher C (2013) Short and long-term outcomes of laparoscopic colectomy in obese patients. World J Gastroenterol WJG 19:7405–7411
Kuhry E, Schwenk WF, Gaupset R, Romild U, Bonjer HJ (2008) Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev. doi:10.1002/14651858.CD003432.pub2
Lee L, Mappin-Kasirer B, Sender Liberman A, Stein B, Charlebois P, Vassiliou M, Fried GM, Feldman LS (2012) High incidence of symptomatic incisional hernia after midline extraction in laparoscopic colon resection. Surg Endosc 26:3180–3185
Parker MC, Wilson MS, Menzies D, Sunderland G, Clark DN, Knight AD, Crowe AM, Surgical Clinical Adhesions, Research G (2005) The SCAR-3 study: 5-year adhesion-related readmission risk following lower abdominal surgical procedures. Colorectal Dis 7:551–558
Holmdahl L, Eriksson E, Eriksson BI, Risberg B (1998) Depression of peritoneal fibrinolysis during operation is a local response to trauma. Surgery 123:539–544
Rosin D, Zmora O, Hoffman A, Khaikin M, Zakai BB, Munz Y, Shabtai M, Ayalon A (2007) Low incidence of adhesion-related bowel obstruction after laparoscopic colorectal surgery. J Laparoendosc Adv Surg Tech 17:604–607
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Nicolò Pecorelli, Massimiliano Greco, Salvatore Amodeo, and Marco Braga have no conflict of interest to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pecorelli, N., Greco, M., Amodeo, S. et al. Small bowel obstruction and incisional hernia after laparoscopic and open colorectal surgery: a meta-analysis of comparative trials. Surg Endosc 31, 85–99 (2017). https://doi.org/10.1007/s00464-016-4995-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4995-6