Abstract
Background
Reliable prediction of operative duration is essential for improving patient and care team satisfaction, optimizing resource utilization and reducing cost. Current operative scheduling systems are unreliable and contribute to costly over- and underestimation of operative time. We hypothesized that the inclusion of patient-specific factors would improve the accuracy in predicting operative duration.
Methods
We reviewed all elective laparoscopic cholecystectomies performed at a single institution between 01/2007 and 06/2013. Concurrent procedures were excluded. Univariate analysis evaluated the effect of age, gender, BMI, ASA, laboratory values, smoking, and comorbidities on operative duration. Multivariable linear regression models were constructed using the significant factors (p < 0.05). The patient factors model was compared to the traditional surgical scheduling system estimates, which uses historical surgeon-specific and procedure-specific operative duration. External validation was done using the ACS-NSQIP database (n = 11,842).
Results
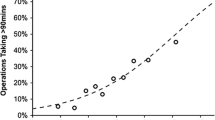
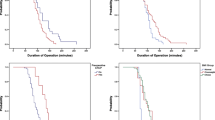
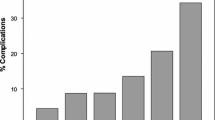
A total of 1801 laparoscopic cholecystectomy patients met inclusion criteria. Female sex was associated with reduced operative duration (−7.5 min, p < 0.001 vs. male sex) while increasing BMI (+5.1 min BMI 25–29.9, +6.9 min BMI 30–34.9, +10.4 min BMI 35–39.9, +17.0 min BMI 40 + , all p < 0.05 vs. normal BMI), increasing ASA (+7.4 min ASA III, +38.3 min ASA IV, all p < 0.01 vs. ASA I), and elevated liver function tests (+7.9 min, p < 0.01 vs. normal) were predictive of increased operative duration on univariate analysis. A model was then constructed using these predictive factors. The traditional surgical scheduling system was poorly predictive of actual operative duration (R 2 = 0.001) compared to the patient factors model (R 2 = 0.08). The model remained predictive on external validation (R 2 = 0.14).The addition of surgeon as a variable in the institutional model further improved predictive ability of the model (R 2 = 0.18).
Conclusion
The use of routinely available pre-operative patient factors improves the prediction of operative duration during cholecystectomy.



Similar content being viewed by others
Abbreviations
- ACS-NSQIP:
-
American College of Surgery National Surgical Quality Improvement Program
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body Mass Index
- CHAID:
-
Chi-squared Automatic Interaction Detection
- CPT:
-
Current Procedural Terminology
- LFT:
-
Liver Function Test
- WBC:
-
White Blood Cell count
References
May JH, Spangler WE, Strum DP, Vargas LG (2011) The surgical scheduling problem: current research and future opportunities. Prod Op Manage 20:392–405
Dexter F, Macario A, Epstein RH, Ledolter J (2005) Validity and usefulness of a method to monitor surgical services’ average bias in scheduled case durations. Can J Anaesth 52:935–939
Strum DP, Sampson AR, May JH, Vargas LG (2000) Surgeon and type of anesthesia predict variability in surgical procedure times. Anesthesiology 92:1454–1466
Dexter F, Dexter EU, Masursky D, Nussmeier NA (2008) Systematic review of general thoracic surgery articles to identify predictors of operating room case durations. Anesth Analg 106:1232–1241
Li Y, Zhang S, Baugh RF, Huang JZ (2009) Predicting surgical case durations using ill-conditioned CPT code matrix. IIE Trans 42:121–135
Macario A (2009) Truth in scheduling: is it possible to accurately predict how long a surgical case will last? Anesth Analg 108:681–685
Dexter F, Macario A, Ledolter J (2007) Identification of systematic underestimation (bias) of case durations during case scheduling would not markedly reduce overutilized operating room time. J Clin Anesth 19:198–203
Zhou J, Dexter F, Macario A, Lubarsky DA (1999) Relying solely on historical surgical times to estimate accurately future surgical times is unlikely to reduce the average length of time cases finish late. J Clin Anesth 11:601–605
Walter SD (1973) A comparison of appointment schedules in a hospital radiology department. Br J Prev Soc Med 27:160–167
Eijkemans MJ, van Houdenhoven M, Nguyen T, Boersma E, Steyerberg EW, Kazemier G (2010) Predicting the unpredictable: a new prediction model for operating room times using individual characteristics and the surgeon’s estimate. Anesthesiology 112:41–49
Gambadauro P, Campo V, Campo S (2015) How predictable is the operative time of laparoscopic surgery for ovarian endometrioma? Minim Invasive Surg 2015:702631
Hosseini N, Hallbeck MS, Jankowski CJ, Huddleston JM, Kanwar A, Pasupathy KS (2014) Effect of obesity and clinical factors on pre-incision time: study of operating room workflow. AMIA Annu Symp Proc 2014:691–699
Wu RL, Aufses AH Jr (2012) Characteristics and costs of surgical scheduling errors. Am J Surg 204:468–473
Lowndes B, Thiels CA, Habermann EB, Bingener J, Hallbeck S, Yu D (2016) Impact of patient factors on procedure duration during laparoscopic cholecystectomy: evaluation from the national surgical quality improvement program (NSQIP) database. Am J Surg. doi:10.1016/j.amjsurg.2016.01.024
Parhizi S, Steege LM, Pasupathy KS (2013) Mining the relationships between psychosocial factors and fatigue dimensions among registered nurses. Int J Ind Ergon 43:82–90
Pasupathy KS, Barker LM (2012) Impact of fatigue on performance in registered nurses: data mining and implications for practice. J Healthc Qual 34:22–30
Bazoua G, Tilston MP (2014) Male gender impact on the outcome of laparoscopic cholecystectomy. JSLS 18:50–54
Lein HH, Huang CS (2002) Male gender: risk factor for severe symptomatic cholelithiasis. World J Surg 26:598–601
Sidhu RS, Raj PK, Treat RC, Scarcipino MA, Tarr SM (2007) Obesity as a factor in laparoscopic cholecystectomy. Surg Endosc 21:774–776
Simopoulos C, Polychronidis A, Botaitis S, Perente S, Pitiakoudis M (2005) Laparoscopic cholecystectomy in obese patients. Obes Surg 15:243–246
Rosen M, Brody F, Ponsky J (2002) Predictive factors for conversion of laparoscopic cholecystectomy. Am J Surg 184:254–258
Del Pin CA, Arthur KS, Honig C, Silverman EM (2002) Laparoscopic cholecystectomy: relationship of pathology and operative time. JSLS 6:149–154
Russell JC, Walsh SJ, Reed-Fourquet L, Mattie A, Lynch J (1998) Symptomatic cholelithiasis: a different disease in men? Connecticut laparoscopic cholecystectomy registry. Ann Surg 227:195–200
Paajanen H, Kakela P, Suuronen S, Paajanen J, Juvonen P, Pihlajamaki J (2012) Impact of obesity and associated diseases on outcome after laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 22:509–513
Yol S, Kartal A, Vatansev C, Aksoy F, Toy H (2006) Sex as a factor in conversion from laparoscopic cholecystectomy to open surgery. JSLS 10:359–363
Thesbjerg SE, Harboe KM, Bardram L, Rosenberg J (2010) Sex differences in laparoscopic cholecystectomy. Surg Endosc 24:3068–3072
Chang WT, Lee KT, Huang MC, Chen JS, Chiang HC, Kuo KK, Chuang SC, Wang SR, Ker CG (2009) The impact of body mass index on laparoscopic cholecystectomy in Taiwan: an oriental experience. J Hepatobiliary Pancreat Surg 16:648–654
Hosseini N, Sir MY, Jankowski CJ, Pasupathy KS (2015) Surgical duration estimation via data mining and predictive modeling: a case study. AMIA Annu Symp Proc 2015:640–648
Acknowledgments
This publication was made possible by funding from the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. The authors would also like to acknowledge Mayo Clinic Anesthesia Clinical Research Unit for their support and help with data extraction.
Author contributions
Thiels, Yu, Habermann, and Bingener contributed to the study design. Thiels, Yu, Abdelrahman, Habermann, Hallbeck, Pasupathy, and Bingener contributed to the analysis and interpretation. All authors contributed to the drafting and critical revisions of the manuscript and gave final approval prior to publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Thiels, Yu, Abdelrahman, Habermann, Hallbeck, and Pasupathy have no conflicts of interest or financial ties to disclose. Dr. Bingener is on the Surgeon Advisory Board of Titan Medical Inc. Support provided by the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery (Thiels, Yu, Abdelrahman, Habermann, Hallbeck, Pasupathy).
Rights and permissions
About this article
Cite this article
Thiels, C.A., Yu, D., Abdelrahman, A.M. et al. The use of patient factors to improve the prediction of operative duration using laparoscopic cholecystectomy. Surg Endosc 31, 333–340 (2017). https://doi.org/10.1007/s00464-016-4976-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4976-9