Abstract
Background
Multiple simulation training programs have demonstrated that effective transfer of skills can be attained and applied into a more complex scenario, but evidence regarding transfer to the operating room is limited.
Objective
To assess junior residents trained with simulation performing an advanced laparoscopic procedure in the OR and compare results to those of general surgeons without simulation training and expert laparoscopic surgeons.
Methods
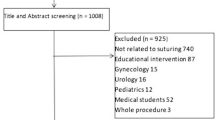
Experimental study: After a validated 16-session advanced laparoscopy simulation training program, junior trainees were compared to general surgeons (GS) with no simulation training and expert bariatric surgeons (BS) in performing a stapled jejuno-jejunostomy (JJO) in the OR. Global rating scale (GRS) and specific rating scale scores, operative time and the distance traveled by both hands measured with a tracking device, were assessed. In addition, all perioperative and immediate postoperative morbidities were registered.
Results
Ten junior trainees, 12 GS and 5 BS experts were assessed performing a JJO in the OR. All trainees completed the entire JJO in the OR without any takeovers by the BS. Six (50 %) BS takeovers took place in the GS group. Trainees had significantly better results in all measured outcomes when compared to GS with considerable higher GRS median [19.5 (18.8–23.5) vs. 12 (9–13.8) p < 0.001] and lower operative time. One morbidity was registered; a patient in the trainees group was readmitted at postoperative day 10 for mechanical ileus that resolved with medical treatment.
Conclusion
This study demonstrated transfer of advanced laparoscopic skills acquired through a simulated training program in novice surgical residents to the OR.



Similar content being viewed by others
References
Al-Kadi AS, Donnon T, Oddone Paolucci E, Mitchell P, Debru E, Church N (2012) The effect of simulation in improving students’ performance in laparoscopic surgery: a meta-analysis. Surg Endosc 26:3215–3224
Zendejas B, Brydges R, Hamstra SJ, Cook DA (2013) State of the evidence on simulation-based training for laparoscopic surgery. A systematic review. Ann Surg 257:586–593
Dawe SR, Windsor JA, Broeders JA, Cregan PC, Hewett PJ, Maddern GJ (2014) A systematic review of surgical skills transfer after simulation-based training laparoscopic cholecystectomy and endoscopy. Ann Surg 259:236–248
Buckley CE, Kavanagh DO, Traynor O, Neary PC (2014) Is the skillset obtained in surgical simulation transferable to the operating theatre? Am J Surg 207:146–157
Palter VN, Orzech N, Reznick RK, Grantcharov TP (2013) Validation of a structured training and assessment curriculum for technical skill acquisition in minimally invasive surgery: a randomized controlled trial. Ann Surg 257:224–230
Ikonen TS, Antikainen T, Silvennoinen M, Isojärvi J, Mäkinen E, Scheinin TM (2012) Virtual reality simulator training of laparoscopic cholecystectomies—a systematic review. Scand J Surg 101:5–12
Scott DJ, Ritter EM, Tesfay ST, Pimentel EA, Nagji A, Fried GM (2008) Certification pass rate of 100% for fundamentals of laparoscopic surgery skills after proficiency-based training. Surg Endosc 22:1887–1893
Aggarwal R, Boza C, Hance J, Leong J, Lacy A, Darzi A (2007) Skills acquisition for laparoscopic gastric bypass in the training laboratory: an innovative approach. Obes Surg 17:19–27
Dehabadi M, Fernando B, Berlingieri P (2014) The use of simulation in the acquisition of laparoscopic suturing skills. Int J Surg 12:258–268
Sabbagh R, Chatterjee S, Chawla A, Hoogenes J, Kapoor A, Matsumoto ED (2012) Transfer of laparoscopic radical prostatectomy skills from bench model to animal model: a prospective, single-blind, randomized, controlled study. J Urol 187:1861–1866
Beyer-Berjot L, Palter V, Grantcharov T, Aggarwal R (2014) Advanced training in laparoscopic abdominal surgery: a systematic review. Surgery 156:676–688
Varas J, Mejia R, Riquelme A, Maluenda F, Buckel E, Salinas J, Martínez J, Aggarwal R, Jarufe N, Boza C (2012) Significant transfer of surgical skills obtained with an advanced laparoscopic training program to a laparoscopic jejunojejunostomy in a live porcine model: feasibility of learning advanced laparoscopy in a general surgery residency. Surg Endosc 26:3486–3494
Szabo Z, Hunter J, Berci G, Sackier J, Cuschieri A (1994) Analysis of surgical movements during suturing in laparoscopy. Endosc Surg Allied Technol 2:55–61
Martin JA, Regehr G, Reznick R, MacRae H, Murnaghan J, Hutchison C, Brown M (1997) Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg 84:273–278
Aggarwal R, Dosis A, Bello F, Darzi A (2006) Motion tracking systems for assessment of surgical skill. Surg Endosc 21:339
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Orzech N, Palter VN, Reznick RK, Aggarwal R, Grantcharov TP (2012) A comparison of 2 ex vivo training curricula for advanced laparoscopic skills: a randomized controlled trial. Ann Surg 255:833–839
Lewis TM, Aggarwal R, Kwasnicki RM, Rajaretnam N, Moorthy K, Ahmed A, Darzi A (2012) Can virtual reality simulation be used for advanced bariatric surgical training? Surgery 151:779–784
Zimmerman H, Latifi R, Dehdashti R, Ong E, Jie T, Galvani C, Waer A, Wynne J, Biffar D, Gruessner R (2011) Intensive laparoscopic training course for surgical residents: program description, initial results, and requirements. Surg Endosc 25:3636–3641
Korndorffer JR Jr, Dunne JB, Sierra R, Stefanidis D, Touchard CL, Scott DJ (2005) Simulator training for laparoscopic suturing using performance goals translates to the operating room. J Am Coll Surg 201:23–29
Scheeres DE, Mellinger JD, Brasser BA, Davis AT (2004) Animate advanced laparoscopic courses improve resident operative performance. Am J Surg 188:157–160
Palter VN, Grantcharov TP (2012) Development and validation of a comprehensive curriculum to teach an advanced minimally invasive procedure: a randomized controlled trial. Ann Surg 256:25–32
Ghaderi I, Manji F, Park YS, Juul D, Ott M, Harris I, Farrell TM (2015) Technical skills assessment toolbox: a review using the unitary framework of validity. Ann Surg 261:251–262
Norcini J, Burch V (2007) Workplace-based assessment as an educational tool: AMEE Guide No. 31. Med Teach 29:855–871
Kirkpatrick DL (1994) Evaluating training programs: the four levels. Berrett-Koehler, San Fransisco
Kirkpatrick D (1996) Revisiting Kirkpatrick’s four-level model, part of Great Ideas Revisited series. In: Training and development, pp 54–59
Sturm LP, Windsor JA, Cosman PH, Cregan P, Hewett PJ, Maddern GJ (2008) A systematic review of skills transfer after surgical simulation training. Ann Surg 248:166–179
Morrison JE, Hammon C (2000) On measuring the effectiveness of large-scale training simulations. VA: Institute for Defense Analysis (DTIC No ADA394491)
Harrington DT, Roye GD, Ryder BA, Miner TJ, Richardson P, Cioffi WG (2007) A time-cost analysis of teaching a laparoscopic entero-enterostomy. J Surg Educ 64:342–345
KA Ericsson (1998) The scientific study of expert levels of performance: General implications for optimal learning and creativity. In: High ability studies. European Council for High Ability, p 90
Acknowledgments
The authors thank Oslando Padilla for his support with the statistical analysis of the data.
Funding
This study was financed and supported by Chilean Research Grant FONDECYT REG.1141196 from CONICYT and by the Department of Digestive Surgery, Faculty of Medicine, Pontificia Universidad Católica de Chile. Dr. Rajesh Aggarwal is consultant for Applied Medical and supported by grant funding from the Montreal General Hospital Foundation and from the Fonds de Recherche Sante Quebec.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Camilo Boza, Felipe León, Erwin Buckel, Arnoldo Riquelme, Fernando Crovari, Jorge Martínez, Teodor Grantcharov, Nicolás Jarufe and Julián Varas have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Boza, C., León, F., Buckel, E. et al. Simulation-trained junior residents perform better than general surgeons on advanced laparoscopic cases. Surg Endosc 31, 135–141 (2017). https://doi.org/10.1007/s00464-016-4942-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4942-6