Abstract
Background
Laparoscopic sigmoidectomy for diverticulitis is widely accepted, using either endolinear staplers or traditional linear staplers under direct vision through the extraction site to transect the rectum. The aim of this study was to assess modifiable factors affecting perioperative morbidity after elective laparoscopic sigmoidectomy for diverticulitis.
Methods
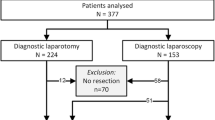
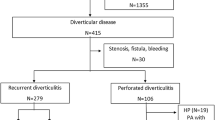
Potential associations between perioperative morbidity and demographic, disease-related, and treatment-related factors were assessed on all consecutive patients included in a prospectively collected database undergoing elective laparoscopic sigmoidectomy for diverticulitis between 1992 and 2013. Rectal transection with a linear stapler under direct vision through the extraction site was considered compatible with laparoscopic technique.
Results
There were two deaths out of 1059 patients (0.19 %). Conversion rate was 13.1 %, overall morbidity 28 %, and anastomotic leak 3.7 %. Independent factors associated with morbidity in an intent-to-treat analysis were ASA 3 (OR 1.53, p = 0.006), conversion (OR 1.71, p = 0.015), and rectal transection without endolinear stapling (traditional linear stapler: OR 1.75, p = 0.003; surgical knife: OR 2.09, p = 0.002). The same factors along with complicated diverticulitis (OR 1.56, p = 0.013) were independently associated with overall morbidity among laparoscopically completed cases. BMI ≥ 35 (OR 2.3, p = 0.017), complicated diverticulitis (OR 2.37, p = 0.002), and rectal transection with a traditional linear stapler (OR 2.19, p = 0.018) were independently associated with abdomino-pelvic infections, both in an intent-to-treat analysis and among laparoscopically completed cases. The number of endolinear stapler firings was not associated with morbidity.
Conclusions
Most factors associated with morbidity of laparoscopic sigmoidectomy for diverticulitis cannot be easily modified. With the limitation of a retrospective analysis, modifiable factors to minimize morbidity are laparoscopic completion and endolinear stapling.
Similar content being viewed by others
Abbreviations
- ASA:
-
American Society of Anesthesiology
- BMI:
-
Body mass index
- CT:
-
Computed tomography
- IRA:
-
Ileorectal anastomosis
- AR:
-
Anterior resection
- TAC:
-
Total abdominal colectomy
References
Gervaz P, Inan I, Perneger T, Schiffer E, Morel P (2010) A prospective, randomized, single-blind comparison of laparoscopic versus open sigmoid colectomy for diverticulitis. Ann Surg 252:3–8
Klarenbeek BR, Veenhof AA, Bergamaschi R, van der Peet DL, van den Broek WT, de Lange ES, Bemelman WA, Heres P, Lacy AM, Engel AF, Cuesta MA (2009) Laparoscopic sigmoid resection for diverticulitis decreases major morbidity rates: a randomized control trial: short-term results of the Sigma trial. Ann Surg 249:39–44
Feingold D, Steele SR, Lee S, Kaiser A, Boushey R, Buie WD, Rafferty JF (2014) Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum 57:284–294
Masoomi H, Buchberg B, Nguyen B, Tung V, Stamos MJ, Mills S (2011) Outcomes of laparoscopic versus open colectomy in elective surgery for diverticulitis. World J Surg 35:2143–2148
Pendlimari R, Touzios J, Azodo I, Chua H, Dozois E, Cima R, Larson D (2011) Short-term outcomes after elective minimally invasive colectomy for diverticulitis. Br J Surg 98:431–435
Jones OM, Stevenson AR, Clark D, Stitz RW, Lumley JW (2008) Laparoscopic resection for diverticular disease: follow-up of 500 consecutive patients. Ann Surg 248:1092–1097
Levack M, Berger D, Sylla P, Rattner D, Bordeianou L (2011) Laparoscopy decreases anastomotic leak rate in sigmoid colectomy for diverticulitis. Arch Surg 146:207–210
Kirchhoff P, Matz D, Dincler S, Buchmann P (2011) Predictive risk factors for intra-and postoperative complications in 526 laparoscopic sigmoid resections due to recurrent diverticulitis: a multivariate analysis. World J Surg 35:677–683
Kim JS, Cho SY, Min BS, Kim NK (2009) Risk factors for anastomotic leakage after laparoscopic intracorporeal colorectal anastomosis with a double stapling technique. J Am Coll Surg 209:694–701
Ito M, Sugito M, Kobayashi A, Nishizawa Y, Tsunoda Y, Saito N (2008) Relationship between multiple numbers of stapler firings during rectal division and anastomotic leakage after laparoscopic rectal resection. Int J Colorectal Dis 23:703–707
Park JS, Choi GS, Kim SH, Kim HR, Kim NK, Lee KY, Kang SB, Kim JY, Lee KY, Kim BC, Bae BN, Son GM, Lee SI, Kang H (2013) Multicenter analysis of risk factors for anastomotic leakage after laparoscopic rectal cancer excision: the Korean laparoscopic colorectal surgery study group. Ann Surg 257:665–671
Yamamoto S, Fujita S, Akasu T, Moriya Y (2005) Safety of laparoscopic intracorporeal rectal transection with double-stapling technique anastomosis. Surg Laparosc Endosc Percutan Tech 15:70–74
Yamamoto S, Fujita S, Akasu T, Inada R, Moriya Y, Yamamoto S (2012) Risk factors for anastomotic leakage after laparoscopic surgery for rectal cancer using a stapling technique. Surg Laparosc Endosc Percutan Tech 22:239–243
Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Kuroyanagi H, Yamaguchi T (2011) Incidence of and risk factors for anastomotic leakage after laparoscopic anterior resection with intracorporeal rectal transection and double-stapling technique anastomosis for rectal cancer. Am J Surg 202:259–264
Milsom JW, de Oliveira O, Jr Trencheva KI, Pandey S, Lee SW, Sonoda T (2009) Long-term outcomes of patients undergoing curative laparoscopic surgery for mid and low rectal cancer. Dis Colon Rectum 52:1215–1222
Senagore AJ (2001) Laparoscopic techniques in intestinal surgery. Surg Innov 8:183–188
Senagore AJ, Duepree HJ, Delaney CP, Brady KM, Fazio VW (2003) Results of a standardized technique and postoperative care plan for laparoscopic sigmoid colectomy. Dis Colon Rectum 46:503–509
Senagore AJ (2005) Laparoscopic sigmoid colectomy for diverticular disease. Surg Clin North Am 85:19–24
Heneghan HM, Martin ST, Kiran RP, Khoury W, Stocchi L, Remzi FH, Vogel JD (2013) Laparoscopic colorectal surgery for obese patients: decreased conversions with the hand-assisted technique. J Gastrointest Surg 17:548–554
Ozturk E, da Luz Moreira A, Vogel J (2010) Hand-assisted laparoscopic colectomy: the learning curve is for operative speed, not for quality. Colorectal Dis 12:e304–e309
Ozturk E, Kiran RP, Geisler DP, Hull TL, Vogel JD (2009) Hand-assisted laparoscopic colectomy: benefits of laparoscopic colectomy at no extra cost. J Am Coll Surg 209:242–247
Delaney C, Fazio V, Senagore A, Robinson B, Halverson A, Remzi F (2001) ‘Fast track’ postoperative management protocol for patients with high co-morbidity undergoing complex abdominal and pelvic colorectal surgery. Br J Surg 88:1533–1538
Zutshi M, Delaney CP, Senagore AJ, Mekhail N, Lewis B, Connor JT, Fazio VW (2005) Randomized controlled trial comparing the controlled rehabilitation with early ambulation and diet pathway versus the controlled rehabilitation with early ambulation and diet with preemptive epidural anesthesia/analgesia after laparotomy and intestinal resection. Am J Surg 189:268–272
R: a language and environment for statistical computing. R Foundation for Statistical Computing. ISBN 3-900051-07-0. http://www.R-project.org/. (2011) 3.0.1
Reshef A, Stocchi L, Kiran R, Flechner S, Budev M, Quintini C, Remzi F (2012) Case-matched comparison of perioperative outcomes after surgical treatment of sigmoid diverticulitis in solid organ transplant recipients versus immunocompetent patients. Colorectal Dis 14:1546–1552
Aytac E, Stocchi L, Ozdemir Y, Kiran R (2013) Factors affecting morbidity after conversion of laparoscopic colorectal resections. Br J Surg 100:1641–1648
Kawada K, Hasegawa S, Hida K, Hirai K, Okoshi K, Nomura A, Kawamura J, Nagayama S, Sakai Y (2014) Risk factors for anastomotic leakage after laparoscopic low anterior resection with DST anastomosis. Surg Endosc 28:2988–2995
HALS Study Group (2000) Hand-assisted laparoscopic surgery vs standard laparoscipic surgery for colorectal disease. Surg Endosc 14:896–901
Marcello PW, Fleshman JW, Milsom JW, Read TE, Arnell TD, Birnbaum EH, Feingold DL, Lee SW, Mutch MG, Sonoda T (2008) Hand-assisted laparoscopic vs. laparoscopic colorectal surgery: a multicenter, prospective, randomized trial. Dis Colon Rectum 51:818–828
Lee SW, Yoo J, Dujovny N, Sonoda T, Milsom JW (2006) Laparoscopic vs. hand-assisted laparoscopic sigmoidectomy for diverticulitis. Dis Colon Rectum 49:464–469
Anderson J, Luchtefeld M, Dujovny N, Hoedema R, Kim D, Butcher J (2007) A comparison of laparoscopic, hand-assist and open sigmoid resection in the treatment of diverticular disease. Am J Surg 193:400–403
Chang Y, Marcello P, Rusin L, Roberts P, Schoetz D (2005) Hand-assisted laparoscopic sigmoid colectomy: helping hand or hindrance? Surg Endosc 19:656–661
Hassan I, You YN, Cima RR, Larson DW, Dozois EJ, Barnes S, Pemberton JH (2008) Hand-assisted versus laparoscopic-assisted colorectal surgery: practice patterns and clinical outcomes in a minimally-invasive colorectal practice. Surg Endosc 22:739–743
Gaertner WB, Kwaan MR, Madoff RD, Willis D, Belzer GE, Rothenberger DA, Melton GB (2013) The evolving role of laparoscopy in colonic diverticular disease: a systematic review. World J Surg 37:629–638
Hassan I, Cima RR, Larson DW, Dozois EJ, O’Byrne MM, Larson DR, Pemberton JH (2007) The impact of uncomplicated and complicated diverticulitis on laparoscopic surgery conversion rates and patient outcomes. Surg Endosc 21:1690–1694
Antolovic D, Reissfelder C, Koch M, Mertens B, Schmidt J, Büchler M, Weitz J (2009) Surgical treatment of sigmoid diverticulitis—analysis of predictive risk factors for postoperative infections, surgical complications, and mortality. Int J Colorectal Dis 24:577–584
Pessaux P, Muscari F, Ouellet J, Msika S, Hay J, Millat B, Fingerhut A, Flamant Y (2004) Risk factors for mortality and morbidity after elective sigmoid resection for diverticulitis: prospective multicenter multivariate analysis of 582 patients. World J Surg 28:92–96
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Jorge Silva-Velazco, Luca Stocchi, Meagan Costedio, Emre Gorgun, Hermann Kessler, and Feza Remzi have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Silva-Velazco, J., Stocchi, L., Costedio, M. et al. Is there anything we can modify among factors associated with morbidity following elective laparoscopic sigmoidectomy for diverticulitis?. Surg Endosc 30, 3541–3551 (2016). https://doi.org/10.1007/s00464-015-4651-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4651-6