Abstract
Background
Inguinal hernia repair is the most common surgery in the world. Health-related quality of life (HRQOL) outcomes are arguably the most important elements of successful repair. This study is aimed to describe short- and long-term quality of life outcomes in patients undergoing laparoscopic inguinal hernia repair.
Methods
We prospectively followed patients who underwent totally extraperitoneal laparoscopic inguinal hernia repair (TEP) as part of an Institutional Review Board-approved study. HRQOL was measured preoperatively, or 3 weeks, 6 months, and 1 year postoperatively using Short Form 36 Health Survey Version 2 (SF-36v2) and Carolinas Comfort Scale. Postoperative HRQOL scores were compared to baseline using paired t tests.
Results
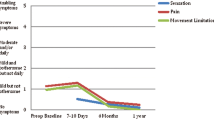
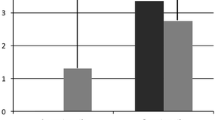
Between June 2009 and February 2014, 1,175 patients underwent TEP by four surgeons. Of those, 301 patients with 388 hernias were registered in the database and followed by a research coordinator. Mean age was 56.4 ± 15.2 years and 93 % were male. Mean body mass index was 26.1 ± 3.7 kg/m2. Seventy-eight percent presented with pain, the majority of which were described as mild. Hernias were unilateral right-sided in 43 %, left-sided in 28 %, and bilateral in 29 %. Eighty-five percent were primary hernias. Average operative time was 43.5 ± 17.9 min and there were no intraoperative complications. Urinary retention occurred in 6 %. Visual analog scale at discharge was 1.9 ± 1.7. Analgesics were used an average of 2.5 ± 3.4 days and return to activities of daily living and work occurred on postoperative 5.5 ± 4.4 and 5.6 ± 3.9 days. Recurrence occurred in 2.1 %. Significant improvements between baseline and 1 year were found in role limitations due to physical health (81.5 ± 25.6 vs. 91.8 ± 19.4, p = 0.02), social functioning (87.4 ± 21.3 vs. 92.9 ± 15.3, p = 0.02), and pain (78.2 ± 19.7 vs. 86.6 ± 15.9, p = 0.007).
Conclusions
TEP results in significant improvement in HRQOL including physical health, social functioning, and pain at 1 year. On average, patients are able to return to activities of daily living and work within a week.


Similar content being viewed by others
References
Bay-Nielsen M, Kehlet H, Strand L, Malmstrom J, Andersen F, Wara P, Juul P, Callesen T (2001) Quality assessment of 26,304 herniorrhaphies in Denmark: a prospective nationwide study. Lancet 358:1124–1128
Rutkow I (1998) Epidemiologic, economic, and sociologic aspects of hernia surgery in the United States in the 1990s. Surg Clin N Am 78:941–951
Palmqvist E, Larsson K, Anell A, Hialmarsson C (2013) Prospective study of pain, quality of life, and the economic impact of open inguinal hernia repair. Br J Surg 100:1483–1488
Magnusson J, Videhult P, Gustafsson U, Nygren J, Thorell A (2014) Relationship between preoperative symptoms and improvement of quality of life in patients undergoing elective inguinal herniorrhaphy. Surgery 155:106–113
Bitzer E, Lorenz C, Nickel S, Dorning H, Trojan A (2008) Patient-reported outcomes in hernia repair. Hernia 12:407–414
Mathur S, Bartlett A, Gilkison W, Krishna G (2006) Quality of life assessment in patients with inguinal hernia. ANZ J Surg 76:491–493
Zieren J, Kupper F, Paul M, Neuss H, Muller J (2003) Inguinal hernia: obligatory indication for elective surgery? A prospective assessment of quality of life before and after plug and patch inguinal hernia repair. Langenbecks Arch Surg 387:417–420
Lawrence K, Jenkinson C, McWhinnie D, Coulter A (1997) Quality of life in patients undergoing inguinal hernia repair. Ann R Coll Surg Engl 79:40–45
Post S, Weiss B, Willer M, Neufang T, Lorenz D (2004) Randomized clinical trial of lightweight composite mesh for Lichtenstein inguinal hernia repair. Br J Surg 91:44–48
Wellwood J, Sculpher M, Stoker D, Nicholls G, Geddes C, Whitehead A, Singh R, Spiegelhalter D (1998) Randomised controlled trial of laparoscopic versus open mesh repair for inguinal hernia: outcome and cost. BMJ 317:103–110
Barrat C, Seriser F, Arnoud R, Trouette P, Champault G (2004) Inguinal hernia repair with beta glucan-coated mesh: prospective multicenter study (115 cases)—preliminary results. Hernia 8:33–38
Arregui M, Davis C, Yucel O, Nagan R (1992) Laparoscopic mesh repair of inguinal hernia using a preperitoneal approach: a preliminary report. Surg Laparosc Endosc 2:53–58
Singh A, Bansal V, Misra M, Kumar S, Rajeshwari S, Kumar A, Sagar R, Kumar A (2011) Testicular functions, chronic groin pain, and quality of life after laparoscopic and open mesh repair of inguinal hernia: a prospective randomized controlled trial. Surg Endosc 26:1304–1317
Abbas A, Abd Ellatif M, Noaman N, Negm A, El-Morsy G, Amin M, Moatamed A (2012) Patient-perspective quality of life after laparoscopic and open hernia repair: a controlled randomized trial. Surg Endosc 26:2465–2470
Eker H, Langeveld H, Klitsie P, Van’t Riet M, Stassen L, Weidema W, Steyerberg E, Lange J, Bonjer H, Jeekel J (2012) Randomized clinical trial of total extraperitoneal inguinal hernioplasty vs Lichtenstein repair: a long-term follow-up study. Arch Surg 147:256–260
Grant A, Scott N, O’Dwyer P (2004) Five-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair of groin hernia. Br J Surg 91:1570–1574
Memon M, Cooper N, Memon B, Memon M, Abrams K (2003) Meta-analysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg 90:1479–1492
Myers E, Browne K, Kavanagh D, Hurley M (2010) Laparoscopic (TEP) versus Lichtenstein inguinal hernia repair: a comparison of quality-of-life outcomes. World J Surg 34:3059–3064
Dhankhar D, Sharma N, Mishra T, Kaur N, Singh S, Gupta S (2014) Totally extraperitoneal repair under general anesthesia versus Lichtenstein repair under local anesthesia for unilateral inguinal hernia: a prospective randomized controlled trial. Surg Endosc 28:996–1002
Kallianpur A, Parshad R, Dehran M, Hazrah P (2007) Ambulatory total extraperitoneal inguinal hernia repair: feasibility and impact on quality of life. JSLS 11:229–234
Pokorny H, Klingler A, Scheyer M, Fugger R, Bischof G (2006) Postoperative pain and quality of life after laparoscopic and open inguinal hernia repair: results of a prospective randomized trial. Hernia 10:331–337
Heniford B, Walters A, Lincourt A, Novitsky Y, Hope W, Kercher K (2008) Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. JACS 206:638–644
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R Jr, Dunlop D, Gibbs J, Reda D, Henderson W (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
Hawn M, Itani K, Giobbie-Hurder A, McCarthy M Jr, Jonasson O, Neumayer L (2006) Patient-reported outcomes after inguinal herniorrhaphy. Surgery 140:198–205
Wauschkuhn C, Schwarz J, Boekeler U, Bittner R (2010) Laparoscopic inguinal hernia repair: gold standard in bilateral repair? Results of more than 2800 patients in comparison to the literature. Surg Endosc 24:3026–3030
Winslow E, Quasebarth M, Brunt L (2004) Perioperative outcomes and complications of open vs laparoscopic extraperitoneal inguinal hernia repair in a mature surgical practice. Surg Endosc 18:221–227
Koch C, Grinberg G, Farley D (2006) Incidence and risk factors for urinary retention after endoscopic hernia repair. Am J Surg 191:381–385
Staerkle R, Buchli C, Villiger P (2009) Patient satisfaction, hernia recurrence rate, and chronic pain 10 years after endoscopic total extraperitoneal inguinal hernia repair. Surg Laparosc Endosc Percutan Tech 19:405–409
Inaba T, Okinaga K, Fukushima R, Ikeda Y, Yamazaki E, Koide T, Horikawa M, Inoue T, Ogawa E (2012) Chronic pain and discomfort after inguinal hernia repair. Surg Today 42:825–829
Alfieeri S, Amid P, Campanelli G, Izard G, Kehlet H, Wijsmuller A, Di Miceli D, Doglietto G (2011) International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia 15:239–249
Reinpold W, Nehls J, Eggert A (2011) Nerve management and chronic pain after open inguinal hernia repair: a prospective two phase study. Ann Surg 254:163–168
Ali S, Zendejas B, Yadav S, Hernandez-Irizarry R, Lohse C, Farley D (2013) Predictors of chronic groin discomfort after laparoscopic totally extraperitoneal inguinal hernia repair. JACS 217:72–78
Acknowledgments
The authors would like to acknowledge the Grainger Foundation for generous financial support that made this project possible.
Disclosures
Michael B. Ujiki, Matthew E. Gitelis, Joann Carbray, Brittany Lapin, John Linn, Steven Haggerty, Chi Wang, Ryota Tanaka, Ermilo Barrera, Zeeshan Butt and Woody Denham have no any relevant conflicts of interest with respect to the authorship and or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ujiki, M.B., Gitelis, M.E., Carbray, J. et al. Patient-centered outcomes following laparoscopic inguinal hernia repair. Surg Endosc 29, 2512–2519 (2015). https://doi.org/10.1007/s00464-014-4011-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-4011-y