Abstract
Background
The ideal incision for laparoscopic specimen extraction is not known. There has been no randomised study thus far evaluating extraction site in laparoscopic colorectal surgery. The aim of our study was to compare post-operative outcomes, pain scores and quality of life scores of vertical periumbilical (VW) versus transverse left iliac fossa (TW) incisions for specimen extraction in laparoscopic anterior resections.
Methods
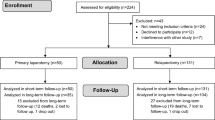
Using an assumption of pain score of 5 in the VW group versus pain score of 2 in the TW group, on day one post-operatively, and based on a 80 % statistical power of analysis to achieve a statistical difference with reduction in pain scores, the sample size per arm calculated was 16. Forty patients undergoing laparoscopic anterior resection were randomised to VW (n = 20) or TW (n = 20). Primary endpoint was post-operative pain. Secondary endpoints were post-operative outcomes, wound cosmesis using Hollander Cosmesis Score and quality of life assessment using EQ-5D at 2 weeks and 2 months post-operatively.
Results
Median pain score on the first post-operative day was 2 in both groups (p = 0.360). There was no significant difference in wound infection rates, operative time or post-operative recovery. Cosmesis scores and EQ-5D scores were also similar in both groups. At a median follow-up of 30 months, the incidence of extraction site incisional hernia was similar.
Conclusion
Transverse and vertical incisions in laparoscopic colorectal surgery have similar post-operative outcomes, with similar pain scores, cosmesis scores, quality of life scores and incisional hernia rates.


Similar content being viewed by others
References
Kam MH, Seow-Choen F, Peng XH, Eu KW, Tang CL, Heah SM, Ooi BS (2004) Minilaparotomy left iliac fossa skin crease incision vs. midline incision for left-sided colorectal cancer. Tech Coloproctol 8:85–88
Donati D, Brown SR, Eu KW, Ho YH, Seow-Choen F (2002) Comparison between midline incision and limited right skin crease incision for right-sided colonic cancers. Tech Coloproctol 6:1–4
Grantcharov TP, Rosenberg J (2001) Vertical compared with transverse incisions in abdominal surgery. Eur J Surg 167:260–267
Brown SR, Goodfellow PB (2005) Transverse verses midline incisions for abdominal surgery. Cochrane Database Syst Rev 19(4):CD005199
Seiler CM, Deckert A, Diener MK, Knaebel HP, Weigand MA, Victor N, Buchler MW (2009) Midline versus transverse incision in major abdominal surgery: a randomized, double-blind equivalence trial. Ann Surg 249:913–920
DeSouza A, Domajnko B, Park J, Marecik S, Prasad L, Abcarian H (2011) Incisional hernia, midline versus low transverse incision: what is the ideal incision for specimen extraction and hand-assisted laparoscopy? Surg Endosc 25:1031–1036
Lim SW, Huh JW, Kim YJ, Kim HR (2013) Vertical transumbilical incision versus left lower transverse incision for specimen retrieval during laparoscopic colorectal surgery. Tech Coloproctol 17:59–65
Mishra A, Keeler B, Maxwell-Armstrong C, Simpson A, Acheson A (2014) The influence of laparoscopy on incisional hernia rates: a retrospective analysis of 1057 colorectal cancer resections. Colorectal Dis. doi:10.1111/codi.12687
Orcutt ST, Balentine CJ, Marshall CL, Robinson CN, Anaya DA, Artinyan A, Awad SS, Berger DH, Albo D (2012) Use of a Pfannenstiel incision in minimally invasive colorectal cancer surgery is associated with a lower risk of wound complications. Tech Coloproctol 16:127–132
Samia H, Lawrence J, Nobel T, Stein S, Champagne BJ, Delaney CP (2013) Extraction site location and incisional hernias after laparoscopic colorectal surgery: should we be avoiding the midline? Am J Surg 205:264–267 discussion 268
Singh R, Omiccioli A, Hegge S, McKinley C (2008) Does the extraction-site location in laparoscopic colorectal surgery have an impact on incisional hernia rates? Surg Endosc 22:2596–2600
Lee L, Mappin-Kasirer B, Sender Liberman A, Stein B, Charlebois P, Vassiliou M, Fried GM, Feldman LS (2012) High incidence of symptomatic incisional hernia after midline extraction in laparoscopic colon resection. Surg Endosc 26:3180–3185
Hollander JE, Singer AJ, Valentine S, Henry MC (1995) Wound registry: development and validation. Ann Emerg Med 25:675–685
Duncan JA, Bond JS, Mason T, Ludlow A, Cridland P, O’Kane S, Ferguson MW (2006) Visual analogue scale scoring and ranking: a suitable and sensitive method for assessing scar quality? Plast Reconstr Surg 118:909–918
Rabin R, de Charro F (2001) EQ-5D: a measure of health status from the EuroQol Group. Ann Med 33:337–343
Chew MH, Chang MH, Tan WS, Wong MT, Tang CL (2013) Conventional laparoscopic versus single-incision laparoscopic right hemicolectomy: a case cohort comparison of short-term outcomes in 144 consecutive cases. Surg Endosc 27:471–477
Ahmed J, Lim M, Khan S, McNaught C, Macfie J (2010) Predictors of length of stay in patients having elective colorectal surgery within an enhanced recovery protocol. Int J Surg 8:628–632
Kuhry E, Schwenk WF, Gaupset R, Romild U, Bonjer HJ (2008) Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev 16(2):CD003432
Sadava EE, Kerman Cabo J, Carballo FH, Bun ME, Rotholtz NA (2014) Incisional hernia after laparoscopic colorectal surgery. Is there any factor associated? http://www.ncbi.nlm.nih.gov/pubmed/24939160. Surg Endosc June 2014. Accessed 29 July 2014
Mudge M, Hughes LE (1985) Incisional hernia: a 10 years prospective study of incidence and attitudes. Br J Surg 72:70–71
Claes K, Beckers R, Heindryckx E, Kyle-Leinhase I, Pletinckx P, Claeys D, Muysoms F (2014) Retrospective observational study on the incidence of incisional hernias after colorectal carcinoma resection with follow-up CT scan. http://www.ncbi.nlm.nih.gov/pubmed/24445348. Hernia 2014. Accessed 5 October 2014
Disclosures
Dr. Wah-Siew Tan, Dr. Min-Hoe Chew, Dr. Kok-Sun Ho, Miss Juriyah Binte Yatim, Miss Joanne Siew-Foon Lai and Associate Professor Choong-Leong Tang have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tan, WS., Chew, MH., Ho, KS. et al. Short and long-term outcomes of a randomised controlled trial of vertical periumbilical wound versus transverse left iliac fossa wound for specimen retrieval in laparoscopic anterior resections. Surg Endosc 29, 2720–2727 (2015). https://doi.org/10.1007/s00464-014-3994-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3994-8