Abstract
Background
The Pfannenstiel incision, widely used in gynecological surgery, has been reported to be associated with lower rates of wound complications than midline incisions in open surgery. However, its effect on wound complications in minimally invasive surgery (MIS) is not well understood. We hypothesize that use of a Pfannenstiel incision in MIS colorectal cancer resections would be associated with fewer short-term wound complication rates.
Methods
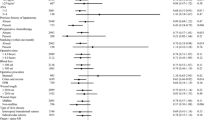
A retrospective cohort study was performed on 171 patients who had undergone MIS colorectal cancer surgery requiring a specimen extraction/hand-access site, divided into a Pfannenstiel and a midline group depending on the type of incision used. Wound complications compared included disruption, infection, dehiscence, evisceration, and fistula formation. The Mann–Whitney U and Fisher’s exact tests were used to analyze differences in risk factors between the groups. Logistic regression was performed to determine factors associated with prevention of wound complications.
Results
Patients in the Pfannenstiel group had significantly lower rates of wound disruption (0 vs. 13%, p = 0.02), superficial surgical site infection (7 vs. 22%, p = 0.03), and overall wound complications (13 vs. 30%, p = 0.04). Using multivariate logistic regression, Pfannenstiel incisions and colon rather than rectal resections were significant predictors of prevention of wound complications.
Conclusions
The use of a Pfannenstiel incision in MIS colorectal cancer resections is associated with a decreased risk of short-term wound complications.
Similar content being viewed by others
References
Abraham NS, Young JM, Solomon MJ (2004) Meta-analysis of short-term outcomes after laparoscopic resection for colorectal cancer. Br J Surg 91:1111–1124
Orenstein SB, Elliott HL, Reines LA, Novitsky YW (2010) Advantages of the hand-assisted versus the open approach to elective colectomies. Surg Endosc 25:1364–1368
Brown SR, Goodfellow PB (2005) Transverse versus midline incisions for abdominal surgery. Cochrane Database Syst Rev 19(4):1–43
Kisielinski K, Conze J, Murken AH, Lenzen NN, Klinge U, Schumpelick V (2004) The Pfannenstiel or so called “bikini cut”: still effective more than 100 years after first description. Hernia 8:177–181
Bergamaschi R, Tuetch JJ, Pessaux P, Arnaud JP (2000) Intracorporeal vs laparoscopic-assisted resection for uncomplicated diverticulitis of the sigmoid. Surg Endosc 14:520–523
Chang YJ, Marcello PW, Rusin LC, Roberts PL, Schoetz DJ (2005) Hand-assisted laparoscopic sigmoid colectomy: helping hand or hindrance? Surg Endosc 19:656–661
Bergamaschi R, Tuech JJ, Cervi C, Arnaud JP (2000) Re-establish pneumoperitoneum in laparoscopic-assisted sigmoid resection? Randomized trial. Dis Colon Rectum 43:771–774
Agha A, Moser C, Iesalnieks I, Piso P, Schlitt HJ (2008) Combination of hand-assisted and laparoscopic proctocolectomy (HALP): technical aspects, learning curve and early postoperative results. Surg Endosc 22:1547–1552
Greene AK, Michetti P, Peppercorn MA, Hodin RA (2000) Laparoscopically assisted ileocolectomy for Crohn’s disease through a pfannenstiel incision. Am J Surg 180:238–240
Fowkes L, Krishna K, Menon A, Greenslade GL, Dixon AR (2008) Laparoscopic emergency and elective surgery for ulcerative colitis. Colorectal Dis 10:373–378
Luijendijk RW, Jeekel J, Storm RK et al (1997) The low transverse Pfannenstiel incision and the prevalence of incisional hernia and nerve entrapment. Ann Surg 225:365–369
Ragupathi M, Ramos-Valadez DI, Yaakovian MD, Haas EM (2011) Single-incision laparoscopic colectomy: a novel approach through a Pfannenstiel incision. Tech Coloproctol 15:61–65
Bratzler DW, Hunt DR (2006) The surgical infection prevention and surgical care improvement projects: national initiatives to improve outcomes for patients having surgery. Clin Infect Dis 43:322–330
Khuri SF, Daley J, Henderson W et al (1998) The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA surgical quality improvement program. Ann Surg 228:491–507
Halm JA, Lip H, Schmitz PI, Jeekel J (2009) Incisional hernia after upper abdominal surgery: a randomised controlled trial of midline versus transverse incision. Hernia 13:275–280
Desouza A, Domajnko B, Park J, Marecik S, Prasad L, Abcarian H (2011) Incisional hernia, midline versus low transverse incision: what is the ideal incision for specimen extraction and hand-assisted laparoscopy? Surg Endosc 25:1031–1036
Singh R, Omiccioli A, Hegge S, McKinley C (2008) Does the extraction-site location in laparoscopic colorectal surgery have an impact on incisional hernia rates? Surg Endosc 22:2596–2600
Konishi T, Watanabe T, Kishimoto J, Nagawa H (2006) Elective colon and rectal surgery differ in risk factors for wound infection: results of prospective surveillance. Ann Surg 244:758–763
Marijnen CA, Kapiteijn E, van de Velde CJ et al (2002) Acute side effects and complications after short-term preoperative radiotherapy combined with total mesorectal excision in primary rectal cancer: report of a multicenter randomized trial. J Clin Oncol 20:817–825
Gendall KA, Raniga S, Kennedy R, Frizelle FA (2007) The impact of obesity on outcome after major colorectal surgery. Dis Colon Rectum 50:2223–2237
Balentine CJ, Wilks J, Robinson C et al (2010) Obesity increases wound complications in rectal cancer surgery. J Surg Res 163:35–39
Acknowledgments
The authors have no disclosures to report. The authors acknowledge financial support and/or resources in the preparation of this manuscript from the Houston Health Services Research and Development Center of Excellence (HF P90-020) at the Michael E. DeBakey VA Medical Center. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Conflict of interests
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Orcutt, S.T., Balentine, C.J., Marshall, C.L. et al. Use of a Pfannenstiel incision in minimally invasive colorectal cancer surgery is associated with a lower risk of wound complications. Tech Coloproctol 16, 127–132 (2012). https://doi.org/10.1007/s10151-012-0808-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-012-0808-7