Abstract
Background
Currently, task time and errors are often used as performance parameters in laparoscopic training. Training with the focus on task time improvement alone results in fast, but possibly less controlled, instrument movements and therefore suboptimal tissue handling skills.
Methods
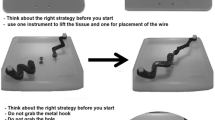
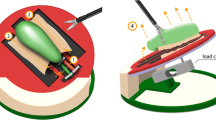
Twenty-five medical students were randomly assigned in two groups. Both groups performed a tissue manipulation task six times. During this training session, the time feedback group (n = 13) received real-time visual feedback of the task time. The force feedback group (n = 12) received real-time visual feedback of the tissue manipulation force. After the training sessions, participants in both groups performed an entirely different task without visual feedback. Task time, force, and motion parameters of this posttest were used to compare the technical skills of the medical students.
Results
The training data of the group that received force feedback showed a learning curve for the mean and max absolute force, max force area, force volume, task time, and path length of both instruments. The data from the group that received time feedback showed a learning curve for the max force, task time, and path length of both instruments. In the posttest, the parameters of mean absolute force (p = 0.039), max force (p = 0.041), and force volume (p = 0.009) showed a significant difference in favor of the group that received force feedback.
Conclusions
The learning curves and the posttest indicate that training with visual force feedback improves tissue handling skills with no negative effect on the task time and instrument motions. Conventional laparoscopic training with visual time feedback improves instrument motion and task time, but it does not improve tissue manipulation skills.






Similar content being viewed by others
References
Crothers IR, Gallagher AG, McClure N, James DTD, McGuigan J (1999) Experienced laparoscopic surgeons are automated to the fulcrum effect: an ergonomic demonstration. Endoscopy 31(5):365–369
Hiemstra E, Chmarra MK, Dankelman J, Jansen FW (2011) Intracorporeal suturing: economy of instrument movements using a box trainer model. J Minim Invasive Gynecol 18(4):494–499
Cotin S, Stylopoulos N, Ottensmeyer M, Neumann P, Rattner D, Dawson S (2002) Metrics for laparoscopic skills trainers: the weakest link! Medical Image Computing and Computer-Assisted Intervention—MICCAI 2002. Lect Notes Comput Sci 2488:35–43
Hofstad EF, Våpenstad C, Chmarra MC, Langø T, Kuhry E, Mårvik R (2013) A study of psychomotor skills in minimally invasive surgery: what differentiates expert and nonexpert performance. Surg Endosc 27(3):854–863
Chmarra MK, Kolkman W, Jansen FW, Grimbergen CA, Dankelman J (2007) The influence of experience and camera holding on laparoscopic instrument movements measured with the TrEndo tracking system. Surg Endosc 21(11):2069–2075
Chmarra MK, Bakker NH, Grimbergen CA, Dankelman J (2006) TrEndo, a device for tracking minimally invasive surgical instruments in training setups. Sensors Actuators A 126(2):328–334
Chmarra MK, Klein S, de Winter JCF, Jansen FW, Dankelman J (2010) Objective classification of residents based on their laparoscopic skills. Surg Endosc 24(5):1031–1039
Moorthy K, Munz Y, Dosis A, Bello F, Darzi A (2003) Motion analysis in the training and assessment of minimally invasive surgery. Minim Invasive Ther Allied Technol 12:137–142
Chmarra MK, Dankelman J, van den Dobbelsteen JJ, Jansen FW (2008) Force feedback and basic laparoscopic skills. Surg Endosc 22(10):2140–2148
Horeman T, Rodrigues SP, Jansen FW, Dankelman J, van den Dobbelsteen JJ (2010) Force measurement platform for training and assessment of laparoscopic skills. Surg Endosc 24(12):3102–3108
Horeman T, Rodrigues SP, van den Dobbelsteen JJ, Jansen FW, Dankelman J (2011) Visual force feedback in laparoscopic training. Surg Endosc 26(1):242–248
Horeman T, Rodrigues SP, Jansen FW, Dankelman J, van den Dobbelsteen JJ (2012) Force parameters for skills assessment in laparoscopy. IEEE 5(4):313–322
Horeman T, Dankelman J, Jansen FW, van den Dobbelsteen JJ (2013) Assessment of laparoscopic skills based on force and motion parameters. IEEE Trans Biomed Eng. doi:10.1109/TBME.2013.2290052
Vassiliou MC, Ghitulescu GA, Feldman LS, Stanbridge D, Leffondre K, Sigman HH, Fried GM (2006) The MISTELS program to measure technical skill in laparoscopic surgery : evidence for reliability. Surg Endosc 20(5):744–747
Rodrigues SP, Horeman T, Dankelman J, van den Dobbelsteen JJ, Jansen FW (2012) Suturing intraabdominal organs: when do we cause tissue damage? Surg Endosc 26(4):1005–1009
Hyltander A, Liljegren E, Rhodin PH, Lönroth H (2002) The transfer of basic skills learnd in laparoscopic simulator to the operating room. Surg Endosc 16(9):1324–1328
Hamilton EC, Scott DJ, Fleming JB, Rege RV, Laycock R, Bergen PC, Tesfay ST, Jones DB (2002) Comparison of video trainer and virtual reality training systems on acquisition of laparoscopic skills. Surg Endosc 16:1324–1328
Grantcharov TP, Kristiansen VB, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P (2004) Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg 91:146–150
Youngblood PL, Srivastava S, Curet M, Heinrichs WL, Dev P, Wren SM (2005) Comparison of training on two laparoscopic simulators and assessment of skills transfer to surgical performance. J Am Coll Surg 200(4):546–551
Scott DJ, Bergen PC, Rege RV, Laycock R, Tesfay ST, Valentine RJ, Euhus DM, Jeyarajah DR, Thompson WM, Jones DB (2000) Laparoscopic training on bench models: better and more cost effective than operating room experience? J Am Coll Surg 191:272–283
Inman T (1860) Foundation for a new theory and practice of medicine (book review). Am J Med Sci 40:450–458
Acknowledgments
The authors would like to thank biomechanical engineering technicians Arjan van Dijke and Hans Drop, Delft University of Technology, for their help in connecting all the electrical components. They thank all surgeons and gynecologists for taking an interest in our study and providing practical information about the learning effects in training. Finally, the authors express special thanks to Gert-Jan Hultzer and René Rodenburg from the skills lab at Leiden University Medical Center for providing us with the necessary instruments, materials, and facilities.
Disclosures
Tim Horeman, Freek van Delft, Mathijs D. Blikkendaal, Jenny Dankelman, John J. van den Dobbelsteen, and Frank-Willem Jansen have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Horeman, T., van Delft, F., Blikkendaal, M.D. et al. Learning from visual force feedback in box trainers: tissue manipulation in laparoscopic surgery. Surg Endosc 28, 1961–1970 (2014). https://doi.org/10.1007/s00464-014-3425-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3425-x