Abstract
Background
Laparo-endoscopic single-site (LESS) surgery involves a single umbilical incision, lending itself to epidural anesthesia. This prospective, randomized study was undertaken to evaluate epidural anesthesia for patients undergoing LESS cholecystectomy, to assess the feasibility, and to analyze all intraoperative and postoperative complications. The secondary objectives were to determine differences in postoperative pain and time until PACU discharge-to-home readiness between patients.
Methods
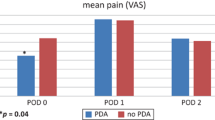
With institutional review board approval, 20 patients with chronic cholecystitis, cholelithiasis, and/or biliary dyskinesia were randomized to receive spinal epidural anesthesia (n = 10) or general anesthesia (n = 10). Postoperative pain at rest was recorded in the PACU every 10 min, and at rest and walking at discharge using the visual analog scale (VAS). Operative time and time until PACU discharge-to-home readiness were recorded. Results are expressed as mean ± SD.
Results
Patient age, American Society of Anesthesiologists class, and body mass index were similar. There were no additional ports/incisions, conversions to “open” operations, or conversions to general anesthesia. There were no differences in operative duration. Time until postanesthesia care unit discharge-to-home ready was not significantly different. The most common postoperative adverse event was urinary retention (1 epidural and 3 general anesthesia patients). Resting postoperative VAS pain score at discharge was 4.7 ± 2.5 vs. 2.2 ± 1.6 (p = 0.02, general versus epidural anesthesia respectively); the stressed VAS pain score at discharge was 6.1 ± 2.3 vs. 3.1 ± 2.8 (p = 0.02, general versus epidural anesthesia respectively).
Conclusions
LESS cholecystectomy with epidural anesthesia was completed with no operative or anesthetic conversions, and less postoperative pain at discharge. Epidural anesthesia appears to be a preferable alternative to general anesthesia for patients undergoing LESS cholecystectomy.



Similar content being viewed by others
References
Hernandez JM, Morton CA, Ross S, Albrink M, Rosemurgy AS (2009) Laparoendoscopic single site cholecystectomy: the first 100 patients. Am Surg 75:681–686
Hernandez J, Ross S, Morton C, McFarlin K, Dahal S, Golkar F, Albrink M, Rosemurgy A (2010) The learning curve of laparoendoscopic single-site (LESS) cholecystectomy: definable, short, and safe. J Am Coll Surg 211:652–657
Hodgett SE, Hernandez JM, Morton CA, Ross S, Albrink M, Rosemurgy AS (2009) Laparoendoscopic single site (LESS) cholecystectomy. J Gastrointest Surg 13:188–192
van Zundert AA, Stultiens G, Jakimowicz JJ, van den Borne BE, van der Ham WG, Wildsmith JA (2006) Segmental spinal anesthesia for cholecystectomy in a patient with severe lung disease. Br J Anaesth 96:464–466
van Zundert AA, Stultiens G, Jakimowicz JJ, Peek D, van der Ham WG, Korsten HH, Wildsmith JA (2007) Laparoscopic cholecystectomy under segmental thoracic spinal anesthesia: a feasibility study. Br J Anaesth 98:682–686
Sinha R, Gurwara AK, Gupta SC (2009) Laparoscopic cholecystectomy under spinal anesthesia: a study of 3492 patients. J Laparoendosc Adv Surg Tech A 19:323–327
Teixeira J, McGill K, Binenbaum S, Forrester G (2009) Laparoscopic single-site surgery for placement of an adjustable gastric band: initial experience. Surg Endosc 23:1409–1414
Yuksek YN, Akat AZ, Gozalan U, Daglar G, Pala Y, Canturk M, Tutuncu T, Kama NA (2008) Laparoscopic cholecystectomy under spinal anesthesia. Am J Surg 195:533–536
Tzovaras G, Fafoulakis F, Pratsas K, Georgopoulou S, Stamatiou G, Hatzitheofilou C (2006) Laparoscopic cholecystectomy under spinal anesthesia: a pilot study. Surg Endosc 20:580–582
Tzovaras G, Zacharoulis D, Georgopoulou S, Pratsas K, Stamatiou G, Hatzitheofilou C (2008) Laparoscopic ventral hernia repair under spinal anesthesia: a feasibility study. Am J Surg 196:191–194
Zhang HW, Chen YJ, Cao MH, Ji FT (2012) Laparoscopic cholecystectomy under epidural anesthesia: a retrospective comparison of 100 patients. Am Surg 78:107–110
Ciofolo MJ, Clergue F, Seebacher J, Lefebvre G, Viars P (1990) Ventilatory effects of laparoscopy under epidural anesthesia. Anesth Analg 70:357–361
Beattie WS, Badner NH, Choi P (2001) Epidural analgesia reduces postoperative myocardial infarction: a meta-analysis. Anesth Analg 93:853–858
Otton PE, Wilson EJ (1966) The cardiocirculatory effects of upper thoracic epidural analgesia. Can Anaesth Soc J 13:541–549
Aldrete JA (1998) Modifications to the postanesthesia score for use in ambulatory surgery. J Perianesth Nurs 13:148–155
McAuley DF (2009) Opiod (narcotic) analgesic converter. GlobalRPh.com. http://www.globalrph.com/narcoticonv.htm. Accessed 12 Feb 2012
Lal P, Philips P, Saxena KN, Kajla RK, Chander J, Ramteke VK (2007) Laparoscopic total extraperitoneal (TEP) inguinal hernia repair under epidural anesthesia: a detailed evaluation. Surg Endosc 21:595–601
Jackson SA, Laurence AS, Hill JC (19996) Does post-laparoscopy pain relate to residual carbon dioxide. Anaesthesia 51:485-487
Coventry DM (1995) Anaesthesia for laparoscopic surgery. J R Coll Surg Edinb 40:151–160
Imbelloni LE, Fornasari M, Fialho JC, Sant’Anna R, Cordeiro JA (2010) General anesthesia versus spinal anesthesia for laparoscopic cholecystectomy. Rev Bras Anestesiol 60:217–227
Lee JH, Huh J, Kim DK, Gil JR, Min SW, Han SS (2010) Laparoscopic cholecystectomy under epidural anesthesia: a clinical feasibility study. Korean J Anesthesiol 59:383–388
Alkhamesi NA, Peck DH, Lomax D, Darzi AW (2007) Intraperitoneal aerosolization of bupivacaine reduces postoperative pain in laparoscopic surgery: a randomized prospective controlled double-blinded clinical trial. Surg Endosc 21:602–606
Pursnani KG, Bazza Y, Calleja M, Mughal MM (1998) Laparoscopic cholecystectomy under epidural anesthesia in patients with chronic respiratory disease. Surg Endosc 12:1082–1084
Chiu AW, Huang WJ, Chen KK, Chang LS (1996) Laparoscopic ligation of bilateral spermatic varices under epidural anesthesia. Urol Int 57:80–84
Park YH, Kang H, Woo YC, Park SG, Baek CW, Jung YH, Kim JY, Koo GH, Kim SD, Park JS (2011) The effect of intraperitoneal bupivacaine on pain after laparoscopic colectomy: a prospective randomized controlled trial. J Surg Res 171:94–100
Phelps P, Cakmakkaya OS, Apfel CC, Radke OC (2008) A simple clinical maneuver to reduce laparoscopy-induced shoulder pain: a randomized controlled trial. Obstet Gynecol 111:1155–1160
Nishio I, Noguchi J, Konishi M, Ochiai R, Takeda J, Fukushima K (1993) The effects of anesthetic techniques and insufflating gases on ventilation during laparoscopy. Masui 42:862–866
Ooka T, Kawano Y, Kosaka Y, Tanaka A (1993) Blood gas changes during laparoscopic cholecystectomy–comparative study of N2O pneumoperitoneum and CO2 pneumoperitoneum. Masui 42:398–401
Ali Y, Elmasry MN, Negmi H, Al Ouffi H, Fahad B, Rahman SA (2008) The feasibility of spinal anesthesia with sedation for laparoscopic general abdominal procedures in moderate risk patients. Middle East J Anesthesiol 19:1027–1039
Ciofolo MJ, Clergue F, Seebacher J, Lefebvre G, Viars P (1990) Ventilatory effects of laparoscopy under epidural anesthesia. Anesth Analg 70:357–361
Song D, Greilich NB, White PF, Watcha MF, Tongier WK (2000) Recovery Profiles and Costs of Anesthesia For Outpatient Unilateral Inguinal Herniorrhaphy. Anesth Analg 91:876–881
Jensen P, Mikkelsen T, Kehlet H (2002) Postherniorrhaphy urinary retention–effect of local, regional, and general anesthesia: a review. Reg Anesth Pain Med 27:612–617
Kamphuis ET, Ionescu TI, Kuipers PW, de Gier J, van Venrooij GE, Boon TA (1998) Recovery of storage and emptying functions of the urinary bladder after spinal anesthesia with lidocaine and with bupivacaine in men. Anesthesiology 88:310–316
Curtis LA, Dolan TS, Cespedes RD (2001) Acute urinary retention and urinary incontinence. Emerg Med Clin North Am 19:591–619
Kuramochi K, Osuga Y, Yano T, Momoeda M, Fujiwara T, Tsutsumi O, Tamai H, Hanaoka K, Koga K, Yoshino O, Taketani Y (2004) Usefulness of epidural anesthesia in gynecologic laparoscopic surgery for infertility in comparison to general anesthesia. Surg Endosc 18:847–851
Shir Y, Raja SN, Frank SM (1994) The effect of epidural versus general anesthesia on postoperative pain and analgesic requirements in patients undergoing radical prostatectomy. Anesthesiology 80:49–56
Aono H, Takeda A, Tarver SD, Goto H (1998) Stress responses in three different anesthetic techniques for carbon dioxide laparoscopic cholecystectomy. J Clin Anesth 10:546–550
Disclosures
Sharona B. Ross, Devanand Mangar, Rachel Karlnoski, Enrico Camporesi, Katheryne Downes, Kenneth Luberice, Krista Haines, and Alexander S. Rosemurgy have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ross, S.B., Mangar, D., Karlnoski, R. et al. Laparo-endoscopic single-site (LESS) cholecystectomy with epidural vs. general anesthesia. Surg Endosc 27, 1810–1819 (2013). https://doi.org/10.1007/s00464-012-2667-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2667-8